Abstract
Objective
To determine the inter-rater reliability of identifying differences and types of differences in lumbar degenerative findings comparing supine and upright MRI.
Materials and methods
Fifty-nine participants, low back pain patients (LBP) with or without leg pain and no-LBP individuals were consecutively enrolled to receive supine and upright MRI of the lumbar spine. Three raters independently evaluated the MRIs for degenerative spinal pathologies and compared for differences. Presence/absence of degenerative findings were recorded for all supine and upright images, and then differences from the supine to the upright positions were classified into no-change, appeared, disappeared, worsened, or improved at each individual disc level. Reliability and agreement were calculated using Gwet’s agreement coefficients (AC1 or AC2) and absolute agreement.
Results
Inter-rater reliability of evaluating differences in eight degenerative lumbar findings comparing the supine and upright MRI position, ranged from 0.929 to 0.996 according to Gwet’s agreement coefficients (AC2). The total number of positive MRI findings in the supine position ranged from 270 to 453, with an average of 366 per rater. Observed differences from supine to upright MRI ranged from 18 to 80, with an average of 56 per rater.
Conclusion
Inter-rater reliability was found overall acceptable for classification of differences in eight types of degenerative pathology observed with supine and upright MRI of the lumbar spine. Results were primarily driven by high numbers and high reliability of rating negative findings, whereas agreement regarding positive findings and positive positional differences was lower.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
It has been suggested that conventional supine MRI may underestimate the presence and degree of gravity-dependent degenerative spinal pathology due to the dynamic nature of some degenerative entities such as disc herniation and scoliosis [1,2,3,4]. There is evidence that upright MRI improves the correlation between image findings and patient symptoms beyond supine MRI [3, 5]. However, upright MRI may also be associated with lower sensitivity to serious findings, due to increased motion artifact, and lower image quality [5]. There are no systematic and critical reviews that have evaluated these issues, but three recent narrative reviews have argued for the value of upright MRI [6,7,8].
Previous studies have investigated the inter-rater reliability of supine MRI findings of the lumbar spine and identified significant variability across degenerative conditions and raters [9, 10]. Hansen et al., [11] assessed supine and upright MRIs on 56 LBP-patients (224 disc levels) with and without sciatica/radiculopathy and found that inter-rater reliability of upright MRI findings of degenerative lumbar spine pathologies was acceptable (kappa > 0.60) for most findings investigated, whereas positional or grading differences in findings from supine to upright position had unacceptable reliability (kappa < 0.60). Since this reliability study was the only publication, we identified comparing supine and upright MRI of the lumbar spine; the objectives of our study was to determine the inter-rater reliability and absolute agreement of lumbar degenerative findings comparing supine and upright MRI.
Materials and methods
Study design
This is a fully crossed inter-rater reliability study reported according to the Guidelines for Reporting Reliability and Agreement Studies (GRRAS) [12].
The study target population
Participants included in this study were a subset of patients with LBP and persons with no LBP living in the Central Denmark Region and enrolled in our main comparative diagnostic test accuracy study. The study had a paired design for index test A (supine MRI) and index test B (upright MRI) in diagnosis of degenerative findings of the lumbar spine. Both studies (reliability and diagnostic accuracy) were carried out at the Department of Radiology, Diagnostic Centre, University Research Clinic for Innovative Patient Pathways, Silkeborg Regional Hospital, Denmark.
The inclusion criteria for LBP patients were (1) referred for MRI from the primary care sector with LBP (with or without back-related leg pain); (2) presence of LBP symptoms for more than 4 weeks; (3) 18 to 60 years of age at the time of consent; (4) not currently waiting for surgery or another advanced hospital procedure indicating specific disease; (5) no suspicion of serious pathology causing symptoms (i.e., cancer, infection or inflammatory arthritis); (6) able to stand for at least 20 min; and (7) able to read and write Danish.
Excluding (1–3) above, the same criteria were used for no-LBP persons with an additional criterion: No presence of LBP for the previous 12 months causing lost workdays. The LBP patients were recruited consecutively from the list of electronic referrals to MRI at the department. No LBP persons were recruited from either the local school of nursing, employees at the hospital, or workplace environments in Silkeborg Municipality/City, Denmark. Most of the recruitment was carried out using posters and by personal communication. All participants provided informed consent via REDCap (Research Electronic Data Capture) on I-pads and completed the electronic questionnaire before imaging procedures could be carried out. I-pads and questions were dealt with by the MRI staff or secretaries.
Sample selection for the reliability study
A total of 242 individuals accepted the invitation to participate in the main study. Six participants were excluded because of age over 60 years and another six participants because of technical problems with their baseline questionnaires or inability to complete the MRI procedures. The remaining 230 individuals defined the study population. Of these, the first 59 consecutive participants were included in the inter-rater reliability study from February 26 to April 26, 2018. An overview of the recruitment and exclusion procedure of participants is provided in Fig. 1.
MRI-procedures
All participants received MRI in the supine position and the upright position. The LBP patients were scanned in the supine position in either a Siemens Avanto.fit 1.5 T (software release E11c) or a Siemens Skyra 3 T MRI system (Software release E11a, Siemens Healthineers GmbH, Erlangen, Germany) and then in the upright position in an open MRI unit: Paramed MROpen 0.5 T (Paramed Medical Systems, Genoa, Italy). Dedicated spine coils were used for all examinations to ensure optimal image quality. The supine and upright MRI procedures were performed on the same day, but in a few cases, due to technical problems with the OpenMRI unit, the upright procedure was delayed up to 5 days. The no-LBP individuals were scanned supine and upright in the open MRI unit on the same day. The imaging protocols for the two conventional MRI systems (1.5 T and 3.0 T) both included a sagittal 2D T2W Turbo Spin Echo (TSE) sequence as well as an axial 2D T2W TSE sequence. The sagittal sequence on the 3.0 T MRI system included the DIXON fat suppression technique. In addition, a sagittal 2D T1W TSE sequence was added to the 1.5 T protocol, while the 3.0 T protocol also included a sagittal 2D T1W Short TI Inversion Recovery (STIR) sequence. The upright 0.5 T MRI system acquired images using a sagittal 2D T2W Spin Echo (SE) sequence and an axial 2D T2W SE sequence (Fig. 2). All MRI sequence parameters can be found in Table 1.
Raters, training, and consensus
The interpretation of all images were performed by three raters, selected from the department: a medical radiologist consultant with 30 years of experience in musculoskeletal MRI (rater A); a Ph.D. student with 28 years of clinical and radiography experience and 4 years of MRI experience including 1000 supervised spinal MRI reports (rater B), and a senior researcher with 12 years of clinical research and MRI experience, including 1000 supervised spinal MRI reports (rater C). All raters had experience with reliability studies and diagnostic classification models in diagnostic imaging [10, 13,14,15,16].
To ensure consensus regarding the understanding of the diagnostic classification of degenerative MRI findings and differences between supine and upright MRI, an evaluation manual was prepared based on existing literature [17,18,19,20,21,22,23,24,25,26]. For training and identifying practical issues in the evaluation process, all three raters independently analyzed and classified 10 MRIs (not included in the reliability study sample) based on the manual. The raters then met for clarification and adjustments to the assessment and coding process. The evaluation manual was adjusted accordingly, and a second set of 5 MRIs was rated independently to adjust for important disagreements and solidify the final version of the manual.
MRI evaluation and classification of findings
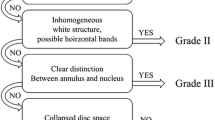
The three raters initially evaluated the three lower lumbar levels: L3/L4, L4/L5, and L5/S1, a total of 177 disc levels, on the supine MRIs for the presence and grading of the following eight degenerative findings using reliable classification methods: spondylolisthesis; scoliosis; annular fissure; disc degeneration; disc contour; nerve root compromise; spinal stenosis; and facet joint degeneration (see classification details in Table 2).
The inter-rater reliability of reporting MRI findings in the supine position has been reported separately and ranged from (Gwet’s AC1 or AC2) 0.64 to 0.99 [10]. According to probabilistic benchmarking to the Landis and Koch scale, this is equivalent to moderate to almost perfect reliability.
The same raters then classified observed differences in findings by comparing images obtained in the supine position to images in the upright position into one of five categories: “No change,” and for positional- or grade-type differences classified into “Appeared,” “Disappeared,” “Worsened,” or “Improved” based on validated methods described in the literature [27] (Fig. 3).
The raters retrieved images in PACS (Picture, Archiving and Communication System: Agfa Impax, version 5.2) and filled in the standardized research evaluation form in REDCap. All images were assessed and analyzed on diagnostic Agfa Impax workstations with high-resolution diagnostic monitors (Totoku Monochrome MS33I2_Pair, 3 million pixels, Barco MDNC-2121 color pair, 2 million pixels, and Barco MDNC-2121 monochrome pair, 2 million pixels). The raters worked independently and were blinded with respect to clinical information and the imaging reports.
Sample size
In a test for agreement between two raters using the Kappa statistic, a sample size of 51 subjects achieves 80% power to detect a true Kappa value of 0.70 in a test of H0: Kappa = κ0 vs. H1: Kappa ≠ κ0, when there are six categories with frequencies equal to 0.48, 0.28, 0.20, 0.03, 0.01, and 0.00. This power calculation was based on a significance level of 0.05 [28].
We decided to include a reasonable sample of 59 individuals, assuming three disc-levels per participant yielding 177 independent units of observation.
Data management and statistical analysis
Data analysis was carried out in Stata, ver.15.1 (StataCorp LLC, 4905 Lakeway Drive, College Station, Texas 77,845, USA) and AgreeStat 2015.1 for Excel Windows/Mac (Advanced Analytics, LLC. PO Box 2696, Gaithersburg, MD 20,886–2696, USA).
In the statistical analysis, inter-rater reliability was determined for nominal data by calculating percent agreement, and a change corrected agreement coefficient: Gwet’s AC1 (unweighted) and AC2 (weighted) for respectively pair-wise raters and for three raters overall [29]. Percent agreement and chance-corrected agreement coefficients (except for marginal totals) were reported with 95% confidence intervals. Proportions of absolute agreement were calculated to evaluate the precision of the strength of reliability. Finally, an additional probabilistic method for benchmarking to an interpretation scale was used and presented as the cumulative probability exceeding 95% for the coefficient to fall into one of the following intervals using the benchmark scale of Landis and Koch: < 0.00 poor; 0.00 to 0.20 slight; 0.21 to 0.40 fair; 0.41 to 0.60 moderate; 0.61 to 0.80 substantial, and 0.81 to 1.00 almost perfect [30]. This method allows for a direct comparison between different agreement coefficients and to what extent they are paradox-resistant, i.e., subject to instability if ratings had very low or very high prevalence.
Results
Sample characteristics
The 59 participants had a mean age of 38.1 years (standard deviation (SD) 14.1), 27 (45.8%) were females, 23 (39.0%) had LBP only, 12 (20.3%) had LBP and leg pain, and 35 (59.3%) had experienced their symptoms for longer than 4 weeks, and 24 (40.7%) did not have LBP. Participant characteristics are presented in Table 3.
Numbers of supine diagnostic MRI findings at disc level
The total number of positive diagnostic findings based on the supine MRI evaluation (presence of degenerative pathology) for rater A was 270 (9.0% of 3009 ratings per rater), rater B was 375 (12.5%), and rater C was 453 (15.1%) (see Table 4).
Number of differences from supine to upright MRI findings at disc level
When comparing all 177 disc levels for observed differences between supine and upright MRI overall, 169 differences were recorded by the three raters (Table 4). Of these, 77 (45.6%) differences in findings were categorized as worsened; 66 (39.0%) appeared, i.e., were not visible on the supine MRI; 12 (7.1%) disappeared, and 14 (8.3%) improved. The number of differences observed per rater across all diagnostic observations were 18 for rater A, 71 for rater B, and 80 for rater C. Summarized, this amount to an average of 56 (15.4%) observed differences on upright MRI per rater, out of 366 observed positive findings on supine MRI.
Proportions of difference in findings from supine to upright position were the following: Nine observed upright differences out of 13 supine findings for scoliosis (0.69), sixty-four observed upright differences out of 189 supine findings of spinal stenosis (0.40), four upright differences out of 15 supine findings of spondylolisthesis (0.27), forty-two upright differences out of 157 supine findings of disc contour (0.27), twenty upright differences out of 76 supine findings of annular fissure (0.26), twenty upright differences out of 87 supine findings of nerve compromise (0.23), and finally, five upright differences out of 199 supine findings of disc degeneration (0.03), and five upright differences out of 362 supine findings of facet degeneration (0.02).
Out of the four sub-categories of observed differences, rater A used “Improved” most often (10 ratings or 55.6% of all observed differences), whereas raters B and C used “Worsened” the most (rater B, 36 ratings or 50.7% and rater C also 36 ratings or 45.0%), followed by “Appeared” (rater B, 29 ratings or 40.8% and rater C, 35 ratings or 43.8%).
Inter-rater reliability of differences and types of difference comparing supine and upright MRI
The reliability of observed difference and type of difference from supine to upright MRI was almost perfect for individual findings, ranging from Gwet’s AC1 = 0.910 for disc contour to 0.998 for spondylolisthesis among individual rater-pairs (Table 5). Overall reliability for the eight degenerative spinal findings was almost perfect (Gwet’s AC2 = 0.966; range: 0.929–0.996). Overall, the variability among rater-pairs was low.
Discussion
In this study sample, taken from a cross-sectional study of participants with and without LBP, we wanted to estimate the inter-rater reliability and absolute agreement of a method identifying presence/absence of differences and types of differences in degenerative MRI findings of the lumbar spine compared in the supine and upright position. The three raters independently evaluated 177 disc levels in 59 participants (for scoliosis, the lumbar spine as one unit). Differences from supine to upright MRI were most often observed in relation to scoliosis, spinal stenosis (central-, lateral recess-, and foraminal-stenosis combined), spondylolisthesis, and disc contour. We attribute this to a relationship between disc degeneration and stenosis, causing the ligamentum flavum to become slack, and presenting as a morphologic change in the weight-bearing position. Scoliosis and spondylolisthesis have been considered a gravity-dependent pathologies, also seen on upright radiographs. The least common degenerative pathologies to show changes from supine to upright position were disc degeneration and facet joint degeneration. The most common pathology to disappear in the upright position was annular fissures. It is generally believed that this can be due to (1) the weightbearing position squeezes the inflammatory fluid away from the lesion, or (2) the dural sac is expanded in the lower portion of the low back, due to spinal fluid collection in the upright position. This can also have an effect by squeezing the inflammatory fluid collection in the disc lesion if located posteriorly
Statistical considerations
Low prevalence rates of positive findings and high prevalence rates of negative findings exposed this study to the Kappa paradoxes. Therefore, we used Gwet’s AC1 and AC2 as being more stable chance-corrected agreement coefficients and better suited for our data [29, 31]. In the Reference section, a link can be found for further information on the probabilistic benchmarking method to the Landis and Koch scale proposed by Kilim L. Gwet [32], making our results comparable to other studies using Kappa statistics and the Landis and Koch scale.
Strength of this study
We think this is an interesting and important topic, and there is a need to establish a more solid piece of evidence to answer whether upright MRI is beneficial for revealing degenerative disease not shown on supine MRI. Also, we found it useful to evaluate if three raters could produce reliable independent readings, not based on consensus. We are in full agreement with Hansen et al., who pointed out, that general high reliability is carried by many patients with no difference between supine and upright position. The grading of fewer patients with differences on the upright MRI is therefore less reliable. This difference can nevertheless be of great importance for the final diagnosis in this group of patients [11]. Maybe most important is the fact that despite the relative lower proportion of MRI findings in this study sample, we found a high proportion of positional differences in the upright position, when a positive degenerative finding was encountered on supine MRI. If disc- and facet joint-degeneration is excluded (0.03 and 0.02 respectively), proportions of positional change ranged from 0.23 to 0.69. These findings are important to research in this field moving forward when designing larger reliability studies with samples of more chronic patients.
Inter-rater reliability and agreement for three raters were found overall acceptable according to Gwet’s Agreement Coefficients for classification of differences and types of differences comparing supine and upright MRI of the lumbar spine (Gwet AC2 ranged 0.929–0.996). An acceptable level of reliability indicates that this classification may be applied by experienced health care professionals or researchers in clinical practice, quality assurance, and research.
This study sample was enrolled consecutively from a comparative diagnostic test accuracy study using a fully paired design (all participants received both index tests A and B), which is considered the most robust with respect to bias [33, 34]. Another strength of this study is that the results reflect a genuine study population of referrals from primary care, and the inclusion of controls (no-LBP participants) is valuable. This was required for validating the method used in our following diagnostic test accuracy study.
Also, there is a lack of studies in the literature of reported reliability on methods to determine differences in degenerative MRI findings of the lumbar spine comparing the supine and upright positions. We have identified only one study by Hansen et al. [11] performing a comprehensive reliability study of differences in degenerative findings observed from supine to upright lumbar MRI. They found differences in only 0.5–1.3% of disc-levels including no differences for disc protrusions and extrusions, and they also found considerable variation in the number of differences recorded between raters evaluating 224 disc levels (n = 56 LBP patients): A total of 17, 39, and 53 differences for readers A, B, and C respectively, with an average absolute agreement of 97.6%; and for comparison, we found a total of 18, 71, and 80 differences in evaluations of 177 disc levels (n = 59 participants) comparing supine and upright MRI for raters A, B, and C respectively, with an average absolute agreement of 96.6%.
Alyas et al. [1], in a pictorial review, concluded that clinically relevant spinal canal stenosis, cauda equina, and nerve root compression might be uncovered by imaging in the erect posture without specifying the type of expected change. Our results differ from some previous studies with respect to the prevalence of differences observed from supine to upright position. In a large retrospective two-rater-study of 4305 LBP patients, Splendiani et al. [2] found differences in 66.6% of the participants from supine to upright MRI when evaluating for types of herniated discs, spinal canal stenosis, lumbar segmental transitional movements, and postural abnormalities of the lumbar spine. In 11%, disc protrusions appeared only on upright MRI. Inter-rater agreement was substantial to almost perfect, with κ values ranging from 0.62 to 0.88. We achieved almost perfect agreement (AC2 ranging from 0.929 to 0.996), although not easily compared to Splendiani et al., because they did not report percent agreement and reported prevalences, where we, like Hansen et al., reported frequency distributions of the MRI outcomes and positional differences according to the rater (Fig. 4).
Limitations
All no-LBP persons received supine MRI procedures in a 0.5-T open MRI unit. Raters could possibly identify no-LBP persons since the image quality was lower, and certain sequences were used specifically for the 0.5-T unit. For the 1.5 T and 3 T systems, the sagittal T2-weighted sequence also included T2 fatsat (DIXON). A possible source of bias was that raters could be inclined to observe fewer positive findings in the no-LBP group. However, our primary aim in this study was related to reliability of reporting change between the two positions rather than the presence of MRI degenerative findings, and we believe the unblinding was less likely to impact this outcome. Rater A seemed to have a higher threshold for detecting change compared to raters B and C. The same was reported by Hansen et al. [1]) in their reliability study of upright MRI findings. In both cases, the most experienced rater had a higher threshold. We assume it represents the routines in a busy radiology department, where radiologists most commonly are looking for the presence of pathology that may change management of the patients. In clinical practice of spinal MRI and LBP, these changes generally need to be pronounced and larger than what was seen in this study. Therefore, we concluded that future studies that involve the evaluation of more discrete changes should emphasize training in agreeing on items relevant for the study aims instead of focusing on “normal” radiology procedures.
This study was initiated to investigate the reliability of a three rater analysis to be used in our main study of larger scale. We also included healthy participants, for the sample to resemble the main study for the same reason. Patient numbers might be considered to be low; however, the included number of participants in our study (59) is comparable to other reliability studies. In fact, we identified only one other reliability study on upright MRI (Hansen et al.), which included 56 participants. The low proportion of differences between supine and upright MRI was a challenge, so we decided to use Gwett’s agreement coefficient (AC1 and AC2), which has proved to be robust, when proportions are very low or very high (see also additional files), and we suggest that future reliability studies focus on more chronic patients and include larger samples.
The raters were not randomly selected, and they worked in the same imaging department. Thus, our results may not generalize to other raters with different training.
Due to ethical considerations concerning stability problems and periodic suboptimal image quality of the upright MRI unit, we had to perform a diagnostic MRI procedure in our conventional 1.5 T or 3.0 T tunnel scanner for all LBP patients. The upright MRI unit was considered an experimental device and was mainly used for research purposes. During this project, we encountered numerous shutdowns due to technical issues. However, despite many delays, we managed to schedule most participants on the same day for both procedures and to obtain an acceptable image quality. The stability issues with the upright MRI unit spanned from abrupt magnet quenches, patient table not working, broken coils to severe image artifacts making the images non-optimal for diagnostic use. These issues caused the upright MRI system to be out of production for extended periods of time. Ideally, no-LBP persons should have had the supine MRI procedure performed in the tunnel scanners. However, the hospital policy did not allow us to use the 1.5 T or 3.0 T scanners for persons without indications for diagnostic imaging. This was due to a generally high workload on the conventional scanners.
Clinical and research implications
Reliability studies are rater and population dependent, and therefore these results may not apply to all the settings and populations where upright MRI technology is used. An acceptable level of reliability carried by almost perfect reliability of negative findings indicates that interpretation and classification of types of differences is difficult and should be used with caution. However, clinically, it is of concern that inter-rater agreement of categorizing positive positional differences is lower. Similar conclusions have been made in another recent study [11]. In recent narrative reviews, Baker et al., Botchu et al., and Michelini et al., concluded that the scanning position is important in the outcome of the MRI examination of the lumbar spine and can be a complementary investigation when there are negative results in conventional MRI in symptomatic patients [6,7,8].
In conclusion, inter-rater reliability according to Gwet’s agreement coefficients for classification of positive and negative findings for eight degenerative pathologies of the lumbar spine comparing supine and upright MRI scans using three raters was found to be overall acceptable. The raters in this study were in good agreement on the classification of negative and positive findings, but less so for the classification of types of changes between supine and upright positions. The classifications used in this study may be sufficiently comprehensible to be applied by health care professionals and in clinical practice, quality assurance, and research, but while the sample size seemed reasonable, our results were driven by a high reliability of the many negative findings. Larger studies or studies including carefully selected patients with specific (and more chronic) degenerative pathologies are needed to investigate the reliability of changes in findings comparing supine and upright MRI. Upright MRI is a supplementary modality that may offer a diagnostic imaging solution in situations where inconsistency is found between clinical findings, patient symptoms, and conventional MRI. It is noteworthy, that in our study, 85% of identified changes between supine and upright position were either not seen or underestimated on supine MRI. The remaining 15% of changes was only seen on supine MRI or underestimated on upright MRI.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- MRI:
-
Magnetic resonance imaging
- AC1:
-
Agreement coefficient (unweighted, two raters)
- AC2:
-
Agreement coefficient (weighted, more than two raters)
- LBP:
-
Low back pain
- REDCap:
-
Research Electronic Data Capture program
- PACS:
-
Picture archiving and communication system (i.e. Agfa Impax)
- CSF:
-
Cerebrospinal fluid
References
Alyas F, Connell D, Saifuddin A. Upright positional MRI of the lumbar spine. Clin Radiol. 2008;63(9):1035–48.
Splendiani A, Perri M, Grattacaso G, Di Tunno V, Marsecano C, Panebianco L, et al. Magnetic resonance imaging (MRI) of the lumbar spine with dedicated G-scan machine in the upright position: a retrospective study and our experience in 10 years with 4305 patients. Radiol Med (Torino). 2016;121(1):38–44.
Tarantino U, Fanucci E, Iundusi R, Celi M, Altobelli S, Gasbarra E, et al. Lumbar spine MRI in upright position for diagnosing acute and chronic low back pain: statistical analysis of morphological changes. J Orthop traumatol Off J Italian Soc Orthop Traumatol. 2013;14(1):15–22.
Hansen BB. Introducing standing weight-bearing MRI in the di-agnostics of low back pain and degenerative spinal disorders. Dan Med J. 2017;64(10).
Khalil JG, Nassr A, Maus TP. Physiologic imaging of the spine. Radiol Clin North Am. 2012;50(4):599–611.
Michelini G, Corridore A, Torlone S, Bruno F, Marsecano C, Capasso R, et al. Dynamic MRI in the evaluation of the spine: state of the art. Acta Biomed. 2018;89(1-S):89–101.
Baker MA, MacKay S. Please be upstanding - a narrative review of evidence comparing upright to supine lumbar spine MRI. Radiography Lond. 2021;27(2):721–6.
Botchu R, Bharath A, Davies AM, Butt S, James SL. Current concept in upright spinal MRI. Eur Spine J Off Publ Eur Spine Soc Eur Spinal Deformity Soc Eur Sect Cervical Spine Res Soc. 2018;27(5):987–93.
Fu MC, Buerba RA, Long WD 3rd, Blizzard DJ, Lischuk AW, Haims AH, et al. Interrater and intrarater agreements of magnetic resonance imaging findings in the lumbar spine: significant variability across degenerative conditions. Spine J. 2014;14(10):2442–8.
Doktor K, Jensen TS, Christensen HW, Fredberg U, Kindt M, Boyle E, et al. Degenerative findings in lumbar spine MRI: an inter-rater reliability study involving three raters. Chiropr Man Therap. 2020;28(1):8.
Hansen BB, Hansen P, Christensen AF, Trampedach C, Rasti Z, Bliddal H, et al. Reliability of standing weight-bearing (0.25T) MR imaging findings and positional changes in the lumbar spine. Skeletal Radiol. 2018;47(1):25–35.
Kottner J, Audige L, Brorson S, Donner A, Gajewski BJ, Hrobjartsson A, et al. Guidelines for Reporting Reliability and Agreement Studies (GRRAS) were proposed. J Clin Epidemiol. 2011;64(1):96–106.
Doktor K, Vilholm ML, Hardardottir A, Christensen HW, Lauritsen J. European guidelines on quality criteria for diagnostic radiographic images of the lumbar spine - an intra- and inter-observer reproducibility study. Chiropr Man Therap. 2019;27:20.
Moll LT, Kindt MW, Stapelfeldt CM, Jensen TS. Degenerative findings on MRI of the cervical spine: an inter- and intra-rater reliability study. Chiropr Man Therap. 2018;26:43.
Masharawi Y, Kjaer P, Bendix T, Manniche C, Wedderkopp N, Sorensen JS, et al. 2008 The reproducibility of quantitative measurements in lumbar magnetic resonance imaging of children from the general population. Spine Phila Pa 1976. 1976;33(19):2094–100.
Jensen TS, Sorensen JS, Kjaer P. Intra- and interobserver reproducibility of vertebral endplate signal (modic) changes in the lumbar spine: the Nordic Modic Consensus Group classification. Acta Radiol. 2007;48(7):748–54.
Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. 2001 Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine Phila Pa 1976. 1976;26(17):1873–8.
Aprill C, Bogduk N. High-intensity zone: a diagnostic sign of painful lumbar disc on magnetic resonance imaging. Br J Radiol. 1992;65(773):361–9.
Lee S, Lee JW, Yeom JS, Kim KJ, Kim HJ, Chung SK, et al. A practical MRI grading system for lumbar foraminal stenosis. AJR Am J Roentgenol. 2010;194(4):1095–8.
Wildermuth S, Zanetti M, Duewell S, Schmid MR, Romanowski B, Benini A, et al. Lumbar spine: quantitative and qualitative assessment of positional (upright flexion and extension) MR imaging and myelography. Radiology. 1998;207(2):391–8.
Modic MT, Masaryk TJ, Ross JS, Carter JR. Imaging of degenerative disk disease. Radiology. 1988;168(1):177–86.
Meyerding HW. Spondylolisthesis; surgical fusion of lumbosacral portion of spinal column and interarticular facets; use of autogenous bone grafts for relief of disabling backache. J Int Coll Surg. 1956;26(5 Part 1):566–91.
Goldstein LA, Waugh TR. Classification and terminology of scoliosis. Clin Orthop Relat Res. 1973;93:10–22.
Cobb JR. Scoliosis; quo vadis. J Bone Joint Surg Am. 1958;40-A(3):507–10.
Carrino JA, Lurie JD, Tosteson AN, Tosteson TD, Carragee EJ, Kaiser J, et al. Lumbar spine: reliability of MR imaging findings. Radiology. 2009;250(1):161–70.
Fardon DF, Williams AL, Dohring EJ, Murtagh FR, Gabriel Rothman SL, Sze GK. Lumbar disc nomenclature: version 2.0: recommendations of the combined task forces of the North American Spine Society, the American Society of Spine Radiology and the American Society of Neuroradiology. Spine J. 2014;14(11):2525–45.
Panagopoulos J, Magnussen JS, Hush J, Maher CG, Crites-Battie M, Jarvik JG, et al. Prospective comparison of changes in lumbar spine MRI findings over time between individuals with acute low back pain and controls: an exploratory study. AJNR Am J Neuroradiol. 2017;38(9):1826–32.
Flack VF, Afifi AA, Lachenbruch PA, Schouten HJA. Sample size determinations for the two rater kappa statistic. Psychometrika. 1988;53(No.3):321–5.
Gwet KL. Handbook of inter-rater reliability - the definitive guide to measuring the extent of agreement among raters/by Kilem Li Gwet - 4th ed. Gaithersburg, MD 20886–2696. United States of America: Advanced Analytics, LLC. 2014.
Landis JR, Koch GG. An application of hierarchical kappa-type statistics in the assessment of majority agreement among multiple observers. Biometrics. 1977;33(2):363–74.
Wongpakaran N, Wongpakaran T, Wedding D, Gwet KL. A comparison of Cohen’s Kappa and Gwet’s AC1 when calculating inter-rater reliability coefficients: a study conducted with personality disorder samples. BMC Med Res Methodol. 2013;13:61.
Gwet KL. K. Gwet's Inter-Rater Reliability Blog 2014 [cited 2019 18–10]. Available from: http://inter-rater-reliability.blogspot.com/2014/12/benchmarking-agreement-coefficients.html.
Yang B WP Davenport CF Deeks JJ Hyde CJ Mallett S Takwoingi Y Leeflang MMG. Guidance on how to use QUADAS-C. Available from University of Bristol Working Group, Guidance on diagnostic accuracy studies. https://www.osfio/hq8mf/files/2020.
Yang B, Vali Y, Dehmoobad Sharifabadi A, Harris IM, Beese S, Davenport C, et al. Risk of bias assessment of test comparisons was uncommon in comparative accuracy systematic reviews: an overview of reviews. J Clin Epidemiol. 2020;127:167–74.
Ross JS Moore KR. Diagnostic Imaging Spine, 3rd edition. 3rd ed. Philadelphia, PA 19103–2899, USA: Elsevier; 2015.
Pathria M. Imaging of spine instability. Semin Musculoskelet Radiol. 2005;9(1):88–99.
Acknowledgements
The authors would like to thank radiographers and others participating in the organization of the project: Annette Kryger Jensen, Jonas Knudsen, Birgitte Hornbæk Korsholm, Maria Jendritska Randlev, Brian Højgaard, and Hanne la Cour Ginnerup, Diagnostic Centre, Silkeborg Regional Hospital; Orla Lund Nielsen, Chiropractic Knowledge Hub, and University of Southern Denmark, for support in data handling. Line Thorndal Moll, Department of Public Health, Aarhus University, Denmark, kindly shared her research and Sara Lisa Doktor for proofreading the manuscript.
Funding
Funding was provided from the Foundation for Advancement of Chiropractic Research and Postgraduate Education in Denmark.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All persons participating in this project provided written informed consent. Approval by the local ethical committee was not needed due to the study’s methodological nature. A letter of exemption from Regional Committee on Health Research Ethics is available from the author on request (case no. 48336). According to journal number 2015–414037, the Danish Data Protection Agency has approved the project. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Authors’ information
Information on authors’ affiliations is found on the first page of this article.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Doktor, K., Hartvigsen, J., Hancock, M. et al. Reliability of reporting differences in degenerative MRI findings of the lumbar spine from the supine to the upright position. Skeletal Radiol 51, 2141–2154 (2022). https://doi.org/10.1007/s00256-022-04060-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-022-04060-2