Abstract
Objective
To assess the degree of narrowing of the popliteal artery during active ankle plantar flexion in healthy volunteers using a non-contrast quiescent-interval single-shot (QISS) magnetic resonance angiography (MRA) technique.
Materials and methods
Following IRB approval, 10 healthy volunteers were recruited and following informed consent underwent QISS MRA of the lower extremity at rest and during ankle plantarflexion. Two pediatric musculoskeletal radiologists independently reviewed MR images in random order and recorded a number of subjective and objective anatomic variables including branch pattern, proximity of vessel to bony structures, gastrocnemius bulk, and presence of accessory muscle. Arterial narrowing with plantarflexion was recorded by a subjective assessment of 3D reconstructions (negligible or non-negligible) and objectively by measuring the narrowest diameter during plantarflexion and at rest. Agreement between reader scores was assessed using the concordance correlation coefficient (CCC) for continuous variables, and kappa and the proportion of agreement for categorical variables.
Results
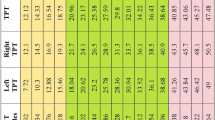
Mean reduction in arterial diameter during plantar flexion was 17.1% (min 1.9%, max 64.1%, SD 16.7%) for reader 1 and 17.2% (min 1.7%, max 50.0%, SD 14.3%.) for reader 2 with high agreement between readers: CCC = 0.92 and CI = 0.82, 0.96. Arterial narrowing was described subjectively as “non-negligible” in 7/20 legs by reader 1 and 5/20 legs by reader 2 with proportion of agreement = 0.90, CI (0.77, 1.00).
Conclusion
We observed a wide range of popliteal arterial narrowing with plantarflexion in asymptomatic volunteers. Larger studies, for which QISS is well suited, may be invaluable for distinguishing physiologic from pathologic arterial narrowing in patients with suspected popliteal artery entrapment syndrome (PAES).








Similar content being viewed by others
References
Stuart TP. Note on a variation in the course of the popliteal artery. J Anat Physiol. 1879;13(Pt 2):162.
Love JW, Whelan TJ. Popliteal artery entrapment syndrome. Am J Surg. 1965;109(5):620–4.
Rignault DP, Pailler JL, Lunel F. The “functional” popliteal entrapment syndrome. Int Angiol. 1985;4(3):341–3.
di Marzo L, Cavallaro A. Popliteal vascular entrapment. World J Surg. 2005;29(Suppl 1):S43–5.
Turnipseed WD. Functional popliteal artery entrapment syndrome: a poorly understood and often missed diagnosis that is frequently mistreated. J Vasc Surg. 2009;49(5):1189–95.
Wady H, Badar Z, Farooq Z, Shaw P, Kobayashi K. Avoiding the trap of misdiagnosis: valuable teaching points derived from a case of longstanding popliteal artery entrapment syndrome. Case Rep Med. 2018;2018:3214561.
Sinha S, Houghton J, Holt PJ, Thompson MM, Loftus IM, Hinchliffe RJ. Popliteal entrapment syndrome. J Vasc Surg. 2012;55(1):252–62.e30.
Kumar R, Warren P, Mannava K. Popliteal artery entrapment syndrome presenting with critical limb ischemia in an adolescent. J Pediatr. 2020;217:215-.e1.
Tsilogianni Z, Grapatsas K, Papanikolaou Z, Kokkini-Paschou A, Tsantilas A, Tsiligiris V, et al. Popliteal artery entrapment syndrome: a common cause of a rare clinical entity--critical leg ischemia in the young. Mil Med. 2014;179(1):e124–6.
Sellers W, Obmann M, Nikam S, Song B, Mariner D. Popliteal artery entrapment syndrome presenting as acute limb ischemia in pregnancy. J Vasc Surg Cases Innov Tech. 2017;3(4):232–5.
Shahi N, Arosemena M, Kwon J, Abai B, Salvatore D, DiMuzio P. Functional popliteal artery entrapment syndrome: a review of diagnosis and management. Ann Vasc Surg. 2019;59:259–67.
Offerman EJ, Hodnett PA, Edelman RR, Koktzoglou I. Nonenhanced methods for lower-extremity MRA: a phantom study examining the effects of stenosis and pathologic flow waveforms at 1.5T. J Magn Reson Imaging. 2011;33(2):401–8.
Edelman RR, Carr M, Koktzoglou I. Advances in non-contrast quiescent-interval slice-selective (QISS) magnetic resonance angiography. Clin Radiol. 2019;74(1):29–36.
Edelman RR, Sheehan JJ, Dunkle E, Schindler N, Carr J, Koktzoglou I. Quiescent-interval single-shot unenhanced magnetic resonance angiography of peripheral vascular disease: technical considerations and clinical feasibility. Magn Reson Med. 2010;63(4):951–8.
Klasen J, Blondin D, Schmitt P, Bi X, Sansone R, Wittsack HJ, et al. Nonenhanced ECG-gated quiescent-interval single-shot MRA (QISS-MRA) of the lower extremities: comparison with contrast-enhanced MRA. Clin Radiol. 2012;67(5):441–6.
Altaha MA, Jaskolka JD, Tan K, Rick M, Schmitt P, Menezes RJ, et al. Non-contrast-enhanced MR angiography in critical limb ischemia: performance of quiescent-interval single-shot (QISS) and TSE-based subtraction techniques. Eur Radiol. 2017;27(3):1218–26.
Arendt CT, Leithner D, Lenga L, Wichmann JL, Albrecht MH, Czwikla R, et al. Multi-observer comparison study between unenhanced quiescent-interval single-shot magnetic resonance angiography and invasive carbon dioxide angiography in patients with peripheral arterial disease and chronic renal insufficiency. Eur J Radiol. 2018;108:140–6.
Hodnett PA, Koktzoglou I, Davarpanah AH, Scanlon TG, Collins JD, Sheehan JJ, et al. Evaluation of peripheral arterial disease with nonenhanced quiescent-interval single-shot MR angiography. Radiology. 2011;260(1):282–93.
Koktzoglou I, Huang R, Ong AL, Aouad PJ, Aherne EA, Edelman RR. Feasibility of a sub-3-minute imaging strategy for ungated quiescent interval slice-selective MRA of the extracranial carotid arteries using radial k-space sampling and deep learning-based image processing. Magn Reson Med. 2020;84(2):825–37.
Edelman RR, Silvers RI, Thakrar KH, Metzl MD, Nazari J, Giri S, et al. Nonenhanced MR angiography of the pulmonary arteries using single-shot radial quiescent-interval slice-selective (QISS): a technical feasibility study. J Cardiovasc Magn Reson. 2017;19(1):48.
Shen D, Edelman RR, Robinson JD, Haji-Valizadeh H, Messina M, Giri S, et al. Single-shot coronary quiescent-interval slice-selective magnetic resonance angiography using compressed sensing: a feasibility study in patients with congenital heart disease. J Comput Assist Tomogr. 2018;42(5):739–46.
Okur A, Kantarci M, Karaca L, Yildiz S, Sade R, Pirimoglu B, et al. Non-contrast-enhanced imaging of haemodialysis fistulas using quiescent-interval single-shot (QISS) MRA: a feasibility study. Clin Radiol. 2016;71(3):244–9.
Kim D, Orron DE, Skillman JJ. Surgical significance of popliteal arterial variants: a unified angiographic classification. Ann Surg. 1989;210(6).
Bidgood WD Jr, Horii SC. Introduction to the ACR-NEMA DICOM standard. Radiographics. 1992;12(2):345–55.
Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45(1):255–68.
Fliess J. Statistical methods for rates and proportions. New York; 1981.
Agresti A. Categorical data analysis. 3rd ed. Hoboken: Wiley; 2013.
Uebersax JS. Diversity of decision-making models and the measurement of interrater agreement. Psychol Bull. 1987;101(1):140.
SAS Institute Inc. SAS/STAT® 14.1 User Guide. Cary: SAS Institute Inc; 2015.
Pillai J, Levien LJ, Haagensen M, Candy G, Cluver MD, Veller MG. Assessment of the medial head of the gastrocnemius muscle in functional compression of the popliteal artery. J Vasc Surg. 2008;48(5):1189–96.
de Almeida MJ, Bonetti Yoshida W, Habberman D, Medeiros EM, Giannini M, Ribeiro de Melo N. Extrinsic compression of popliteal artery in asymptomatic athlete and non-athlete individuals. A comparative study using duplex scan (color duplex sonography). Int Angiol. 2004;23(3):218–29.
Gourgiotis S, Aggelakas J, Salemis N, Elias C, Georgiou C. Diagnosis and surgical approach of popliteal artery entrapment syndrome: a retrospective study. Vasc Health Risk Manag. 2008;4(1):83–8.
Akkersdijk WL, de Ruyter JW, Lapham R, Mali W, Eikelboom BC. Colour duplex ultrasonographic imaging and provocation of popliteal artery compression. Eur J Vasc Endovasc Surg. 1995;10(3):342–5.
Hoffmann U, Vetter J, Rainoni L, Leu AJ, Bollinger A. Popliteal artery compression and force of active plantar flexion in young healthy volunteers. J Vasc Surg. 1997;26(2):281–7.
Chernoff DM, Walker AT, Khorasani R, Polak JF, Jolesz FA. Asymptomatic functional popliteal artery entrapment: demonstration at MR imaging. Radiology. 1995;195(1):176–80.
Hodnett PA, Ward EV, Davarpanah AH, Scanlon TG, Collins JD, Glielmi CB, et al. Peripheral arterial disease in a symptomatic diabetic population: prospective comparison of rapid unenhanced MR angiography (MRA) with contrast-enhanced MRA. AJR Am J Roentgenol. 2011;197(6):1466–73.
Hansmann J, Morelli JN, Michaely HJ, Riester T, Budjan J, Schoenberg SO, et al. Nonenhanced ECG-gated quiescent-interval single shot MRA: image quality and stenosis assessment at 3 tesla compared with contrast-enhanced MRA and digital subtraction angiography. J Magn Reson Imaging. 2014;39(6):1486–93.
Varga-Szemes A, Wichmann JL, Schoepf UJ, Suranyi P, De Cecco CN, Muscogiuri G, et al. Accuracy of noncontrast quiescent-interval single-shot lower extremity MR angiography versus CT angiography for diagnosis of peripheral artery disease: comparison with digital subtraction angiography. JACC Cardiovasc Imaging. 2017;10(10 Pt A):1116–24.
Keller S, Yamamura J, Sedlacik J, Wang Z, Gebert P, Starekova J, et al. Diffusion tensor imaging combined with T2 mapping to quantify changes in the skeletal muscle associated with training and endurance exercise in competitive triathletes. Eur Radiol. 2020;30(5):2830–42.
Mathew RC, Kramer CM. Recent advances in magnetic resonance imaging for peripheral artery disease. Vasc Med. 2018;23(2):143–52.
Ledermann HP, Heidecker HG, Schulte AC, Thalhammer C, Aschwanden M, Jaeger KA, et al. Calf muscles imaged at BOLD MR: correlation with TcPO2 and flowmetry measurements during ischemia and reactive hyperemia--initial experience. Radiology. 2006;241(2):477–84.
Filli L, Boss A, Wurnig MC, Kenkel D, Andreisek G, Guggenberger R. Dynamic intravoxel incoherent motion imaging of skeletal muscle at rest and after exercise. NMR Biomed. 2015;28(2):240–6.
Acknowledgements
The authors wish to extend their gratitude to James Connors RT(MR) and MRI Quality Improvement Coordinator at Boston Children’s Hospital with his assistance in this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Breen, M.A., Hassan, M.M., Johnston, P. et al. Quantification of popliteal artery narrowing with QISS MRA during active ankle plantarflexion in healthy, asymptomatic volunteers and its potential application in the diagnosis of popliteal artery entrapment syndrome (PAES). Skeletal Radiol 50, 2091–2102 (2021). https://doi.org/10.1007/s00256-021-03751-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-021-03751-6