Abstract
Objective
To investigate the performance of contrast-enhanced MRI for predicting avascular necrosis (AVN) of the treated femoral head after surgical reduction for developmental dysplasia of the hip (DDH) using qualitative and quantitative methods.
Methods and materials
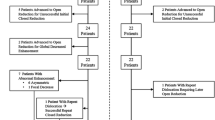
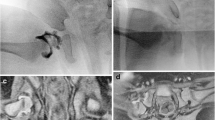
This IRB-approved, HIPAA compliant retrospective study included 47 children who underwent same-day contrast-enhanced MRI following unilateral surgical hip reduction between April 2009 and June 2018. Blinded to the clinical outcome, 3 reviewers (2 pediatric radiologists and 1 pediatric orthopedist) independently categorized the enhancement pattern of the treated femoral head. Signal intensities, measured using regions of interest (ROI), were compared between treated and untreated hips and percent enhancements were compared between hips that developed and did not develop AVN. Post-reduction radiographs were evaluated using Salter’s criteria for AVN and Kalmachi and MacEwen’s classification for growth disturbance. Non-parametric tests and Fisher exact test were used to compare enhancement values between AVN and non-AVN hips. Bonferroni correction was used for multiple comparisons.
Results
Ten (21%) out of the 47 children (7 boys and 40 girls; mean age 9.0 ± 4.7 months) developed AVN. Age at surgical reduction was significantly higher (p = 0.03) for hips that developed AVN. No significant differences were found in gender (p = 0.61), laterality (p = 0.46), surgical approach (p = 0.08), history of pre-operative bracing (p = 0.72), abduction angle (p = 0.18–0.44), enhancement pattern (p = 0.66–0.76), or percent enhancement (p = 0.41–0.88) between AVN and non-AVN groups.
Conclusion
Neither enhancement pattern nor percent enhancement predicted AVN, suggesting that post-reduction conventional MRI does not accurately distinguish between reversible and permanent vascular injury.



Similar content being viewed by others
References
Patel H. Preventive health care, 2001 update: screening and management of developmental dysplasia of the hip in newborns. Cmaj. 2001;164(12):1669–77.
Shipman SA, Helfand M, Moyer VA, Yawn BP. Screening for developmental dysplasia of the hip: a systematic literature review for the US Preventive Services Task Force. Pediatrics. 2006;117(3):e557–76.
Lee MC, Eberson CP. Growth and development of the child’s hip. Orthop Clin North Am. 2006;37(2):119–32 v.
American Academy of Orthopaedic Surgeons. Detection and nonoperative management of pediatric developmental dysplasia of the hip in infants up to six months of age. Evidence-based clinical practice guideline. Rosemont: American Academy of Orthopaedic Surgeons; 2014.
American College of Radiology. AIUM-ACR-SPR-SRU practice parameter for the performance of an ultrasound examination for detection and assessment of developmental dysplasia of the hip. J Ultrasound Med. 2018;37(11):E1–e5.
American Academy of Pediatrics. Clinical practice guideline: early detection of developmental dysplasia of the hip. Committee on Quality Improvement, Subcommittee on Developmental Dysplasia of the Hip. American Academy of Pediatrics. Pediatrics. 2000;105(4 Pt 1):896–905.
American College of Radiology. ACR appropriateness criteria - developmental dysplasia of the hip (DDH)–Child. 2019.
Wenger D, Duppe H, Tiderius CJ. Acetabular dysplasia at the age of 1 year in children with neonatal instability of the hip. Acta Orthop. 2013;84(5):483–8.
Sankar WN, Nduaguba A, Flynn JM. Ilfeld abduction orthosis is an effective second-line treatment after failure of Pavlik harness for infants with developmental dysplasia of the hip. J Bone Joint Surg Am. 2015;97(4):292–7.
Ucar DH, Isiklar ZU, Kandemir U, Tumer Y. Treatment of developmental dysplasia of the hip with Pavlik harness: prospective study in Graf type IIc or more severe hips. J Pediatr Orthop B. 2004;13(2):70–4.
Nguyen JC, Dorfman SR, Rigsby CK, Iyer RS, Alazraki AL, Anupindi SA, et al. ACR appropriateness criteria((R)) developmental dysplasia of the hip-child. J Am Coll Radiol. 2019;16(5s):S94–s103.
Haruno LS, Kan JH, Rivlin MJ, Rosenfeld SB, Schallert EK, Zhu H, et al. Spica MRI predictors for epiphyseal osteonecrosis after closed reduction treatment of dysplasia of the hip. J Pediatr Orthop B. 2019.
Sankar WN, Gornitzky AL, Clarke NMP, Herrera-Soto JA, Kelley SP, Matheney T, et al. Closed reduction for developmental dysplasia of the hip: early-term results from a prospective. Multicenter Cohort J Pediatr Orthop. 2019;39(3):111–8.
Novais EN, Hill MK, Carry PM, Heyn PC. Is age or surgical approach associated with osteonecrosis in patients with developmental dysplasia of the hip? A Meta-analysis. Clin Orthop Relat Res. 2016;474(5):1166–77.
Thomas IH, Dunin AJ, Cole WG, Menelaus MB. Avascular necrosis after open reduction for congenital dislocation of the hip: analysis of causative factors and natural history. J Pediatr Orthop. 1989;9(5):525–31.
Gornitzky AL, Georgiadis AG, Seeley MA, Horn BD, Sankar WN. Does perfusion MRI after closed reduction of developmental dysplasia of the hip reduce the incidence of avascular necrosis? Clin Orthop Relat Res. 2016;474(5):1153–65.
Novais EN, Kestel LA, Carry PM, Meyers ML. Higher Pavlik harness treatment failure is seen in Graf type IV Ortolani-positive hips in males. Clin Orthop Relat Res. 2016;474(8):1847–54.
Brougham DI, Broughton NS, Cole WG, Menelaus MB. Avascular necrosis following closed reduction of congenital dislocation of the hip. Review of influencing factors and long-term follow-up. J Bone Joint Surg British Vol. 1990;72(4):557–62.
Kalamchi A, MacEwen GD. Avascular necrosis following treatment of congenital dislocation of the hip. J Bone Joint Surg Am. 1980;62(6):876–88.
Tiderius C, Jaramillo D, Connolly S, Griffey M, Rodriguez DP, Kasser JR, et al. Post-closed reduction perfusion magnetic resonance imaging as a predictor of avascular necrosis in developmental hip dysplasia: a preliminary report. J Pediatr Orthop. 2009;29(1):14–20.
Haruno LS, Kan JH, Rivlin MJ, Rosenfeld SB, Schallert EK, Zhu H, et al. Spica MRI predictors for epiphyseal osteonecrosis after closed reduction treatment of dysplasia of the hip. J Pediatr Orthop B. 2019;28(5):424–9.
Jaramillo D, Villegas-Medina O, Laor T, Shapiro F, Millis MB. Gadolinium-enhanced MR imaging of pediatric patients after reduction of dysplastic hips: assessment of femoral head position, factors impeding reduction, and femoral head ischemia. AJR Am J Roentgenol. 1998;170(6):1633–7.
Jaramillo D, Villegas-Medina OL, Doty DK, Dwek JR, Ransil BJ, Mulkern RV, et al. Gadolinium-enhanced MR imaging demonstrates abduction-caused hip ischemia and its reversal in piglets. AJR Am J Roentgenol. 1996;166(4):879–87.
DeFrancesco CJ, Blumberg TJ, Chauvin NA, Sankar WN. An improved method for measuring hip abduction in spica after surgical reduction for developmental dysplasia of the hip. J Child Orthop. 2017;11(4):277–83.
Bedoya MA, Jaimes C, Khrichenko D, Delgado J, Dardzinski BJ, Jaramillo D. Dynamic gadolinium-enhanced MRI of the proximal femur: preliminary experience in healthy children. AJR Am J Roentgenol. 2014;203(4):W440–6.
Salter RB, Kostuik J, Dallas S. Avascular necrosis of the femoral head as a complication of treatment for congenital dislocation of the hip in young children: a clinical and experimental investigation. Can J Surg. 1969;12(1):44–61.
Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–74.
Nguyen JC, Markhardt BK, Merrow AC, Dwek JR. Imaging of pediatric growth plate disturbances. Radiographics. 2017;37(6):1791–812.
Segal LS, Boal DK, Borthwick L, Clark MW, Localio AR, Schwentker EP. Avascular necrosis after treatment of DDH: the protective influence of the ossific nucleus. J Pediatr Orthop. 1999;19(2):177–84.
Roposch A, Odeh O, Doria AS, Wedge JH. The presence of an ossific nucleus does not protect against osteonecrosis after treatment of developmental dysplasia of the hip. Clin Orthop Relat Res. 2011;469(10):2838–45.
Roposch A, Stohr KK, Dobson M. The effect of the femoral head ossific nucleus in the treatment of developmental dysplasia of the hip. A meta-analysis. J Bone Joint Surg Am. 2009;91(4):911–8.
Luhmann SJ, Bassett GS, Gordon JE, Schootman M, Schoenecker PL. Reduction of a dislocation of the hip due to developmental dysplasia. Implications for the need for future surgery. J Bone Joint Surg Am. 2003;85(2):239–43.
Shin CH, Yoo WJ, Park MS, Kim JH, Choi IH, Cho TJ. Acetabular remodeling and role of osteotomy after closed reduction of developmental dysplasia of the hip. J Bone Joint Surg Am. 2016;98(11):952–7.
Luhmann SJ, Schoenecker PL, Anderson AM, Bassett GS. The prognostic importance of the ossific nucleus in the treatment of congenital dysplasia of the hip. J Bone Joint Surg Am. 1998;80(12):1719–27.
Xu M, Gao S, Sun J, Yang Y, Song Y, Han R, et al. Predictive values for the severity of avascular necrosis from the initial evaluation in closed reduction of developmental dysplasia of the hip. J Pediatr Orthop B. 2013;22(3):179–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the Children’s Hospital of Philadelphia’s institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was not required for this retrospective study according to the Children’s Hospital of Philadelphia’s IRB.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Nguyen, J.C., Back, S.J., Barrera, C.A. et al. Developmental dysplasia of the hip: can contrast-enhanced MRI predict the development of avascular necrosis following surgery?. Skeletal Radiol 50, 389–397 (2021). https://doi.org/10.1007/s00256-020-03572-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-020-03572-z