Abstract
Objective
Compare a two sequence protocol to a standard protocol in the detection of pedal osteomyelitis (OM) and abscesses and to identify patients that benefit from a full protocol.
Materials and methods
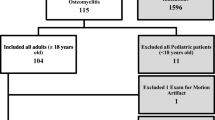
One hundred thirty-two foot MRIs ordered to assess for OM were enrolled, and the following items were extracted from the clinical reports: use of IV contrast, the presence of OM, reactive osteitis, and a soft tissue abscess. Using only one T1 nonfat-suppressed and one fluid sensitive fat-suppressed sequences, two experienced musculoskeletal radiologists reviewed each case for the presence of OM, reactive osteitis, or an abscess. A Kappa test was calculated to assess for interobserver agreement, and diagnostic performance was determined. The McNemar test was used to assess for the effect of contrast.
Results
Agreement between both observers and the clinical report on the presence of osteomyelitis was substantial ( k = 0.63 and 0.72, p < 0.001), while the agreement for abscess was fair (k = 0.29 and 0.38, p < 0.001). For osteomyelitis, both observers showed good accuracy (0.85 and 0.86). When screening bone for a normal versus abnormal case, this method was highly sensitive (0.97–0.98), but was less sensitive for abscess (0.63–0.75). Fifty-one percent of exams used contrast, and it did impact the diagnosis of abscess for one observer.
Conclusion
This rapid protocol is accurate in making the diagnosis of OM, and its high sensitivity makes it useful to screen for patients that would benefit from a full protocol.




Similar content being viewed by others
Abbreviations
- OM:
-
Osteomyelitis
- RO:
-
Reactive osteitis
- EO:
-
Early osteomyelitis
- DFU:
-
Diabetic foot ulcer
- IV:
-
Intravenous
- ACR:
-
American College of Radiology
- BKA:
-
Below the knee amputation
- STIR:
-
Short tau inversion recovery
References
Geraghty T, LaPorta G. Current health and economic burden of chronic diabetic osteomyelitis. Expert Rev Pharmacoecon Outcomes Res. 2019;19(3):279–86.
Armstrong DG, Boulton AJM, Bus SA. Diabetic foot ulcers and their recurrence. N Engl J Med. 2017;376(24):2367–75.
Schweitzer ME, Daffner RH, Weissman BN, Bennett DL, Blebea JS, Jacobson JA, et al. ACR appropriateness criteria on suspected osteomyelitis in patients with diabetes mellitus. J Am Coll Radiol. 2008;5(8):881–6.
Al-Khawari HA, Al-Saeed OM, Jumaa TH, Chishti F. Evaluating diabetic foot infection with magnetic resonance imaging: Kuwait experience. Med Princ Pract. 2005;14(3):165–72.
Ledermann HP, Morrison WB, Schweitzer ME. Pedal abscesses in patients suspected of having pedal osteomyelitis: analysis with MR imaging. Radiology. 2002;224(3):649–55.
Kapoor A, Page S, Lavalley M, Gale DR, Felson DT. Magnetic resonance imaging for diagnosing foot osteomyelitis: a meta-analysis. Arch Intern Med. 2007;167(2):125–32.
Mahendra M, Singh R. Diagnostic accuracy and surgical utility of MRI in complicated diabetic foot. J Clin Diagn Res. 2017;11(7):RC01–4.
Chow I, Lemos EV, Einarson TR. Management and prevention of diabetic foot ulcers and infections: a health economic review. Pharmacoeconomics. 2008;26(12):1019–35.
Kan JH, Estrada C, Hasan U, Bracikowski A, Shyr Y, Shakhtour B, et al. Management of occult fractures in the skeletally immature patient: cost analysis of implementing a limited trauma magnetic resonance imaging protocol. Pediatr Emerg Care. 2009;25(4):226–30.
May LA, Chen DC, Bui-Mansfield LT, O'Brien SD. Rapid magnetic resonance imaging evaluation of femoral neck stress fractures in a U.S. active duty military population. Mil Med. 2017;182(1):e1619–25.
May DA, Disler DG. Screening for avascular necrosis of the hip with rapid MRI: preliminary experience. J Comput Assist Tomogr. 2000;24(2):284–7.
Ross AB, Chan BY, Yi PH, Repplinger MD, Vanness DJ, Lee KS. Diagnostic accuracy of an abbreviated MRI protocol for detecting radiographically occult hip and pelvis fractures in the elderly. Skelet Radiol. 2019;48(1):103–8.
Khurana B, Okanobo H, Ossiani M, Ledbetter S, Al Dulaimy K, Sodickson A. Abbreviated MRI for patients presenting to the emergency department with hip pain. AJR Am J Roentgenol. 2012;198(6):W581–8.
Khoury NJ, Birjawi GA, Chaaya M, Hourani MH. Use of limited MR protocol (coronal STIR) in the evaluation of patients with hip pain. Skelet Radiol. 2003;32(10):567–74.
Kotecha HM, Lo HS, Vedantham S, Shin H, Cerniglia CA. Abbreviated MRI of the foot in patients with suspected osteomyelitis. Emerg Radiol. 2019.
Hallgren KA. Computing Inter-Rater Reliability for Observational Data: An Overview and Tutorial. Tutor Quant Methods Psychol. 2012;8(1):23–34.
Duryea D, Bernard S, Flemming D, Walker E, French C. Outcomes in diabetic foot ulcer patients with isolated T2 marrow signal abnormality in the underlying bone: should the diagnosis of "osteitis" be changed to "early osteomyelitis"? Skelet Radiol. 2017;46(10):1327–33.
Ledermann HP, Schweitzer ME, Morrison WB. Nonenhancing tissue on MR imaging of pedal infection: characterization of necrotic tissue and associated limitations for diagnosis of osteomyelitis and abscess. AJR Am J Roentgenol. 2002;178(1):215–22.
Morrison WB, Schweitzer ME, Wapner KL, Hecht PJ, Gannon FH, Behm WR. Osteomyelitis in feet of diabetics: clinical accuracy, surgical utility, and cost-effectiveness of MR imaging. Radiology. 1995;196(2):557–64.
Meyr AJ, Singh S, Zhang X, Khilko N, Mukherjee A, Sheridan MJ, et al. Statistical reliability of bone biopsy for the diagnosis of diabetic foot osteomyelitis. J Foot Ankle Surg. 2011;50(6):663–7.
Chadayammuri V, Herbert B, Hao J, Mavrogenis A, Quispe JC, Kim JW, et al. Diagnostic accuracy of various modalities relative to open bone biopsy for detection of long bone posttraumatic osteomyelitis. Eur J Orthop Surg Traumatol. 2017;27(7):871–5.
Elmarsafi T, Kumar A, Cooper PS, Steinberg JS, Evans KK, Attinger CE, et al. Concordance between bone pathology and bone culture for the diagnosis of osteomyelitis in the presence of Charcot neuro-osteoarthropathy. J Foot Ankle Surg. 2018;57(5):919–23.
Meyr AJ, Seo K, Khurana JS, Choksi R, Chakraborty B. Level of agreement with a multi-test approach to the diagnosis of diabetic foot osteomyelitis. J Foot Ankle Surg. 2018;57(6):1137–9.
Ramanujam CL, Han D, Zgonis T. Medical imaging and laboratory analysis of diagnostic accuracy in 107 consecutive hospitalized patients with diabetic foot osteomyelitis and partial foot amputations. Foot Ankle Spec. 2018;11(5):433–43.
Author information
Authors and Affiliations
Contributions
Drs. Umpierrez and Kakarala did the review of the 132 cases. Drs. Maceroli and Rajani provided the surgical insight for the project from an orthopedic and vascualar surgery perspective, respectively. Dr. Schechter provided insight from an infectious disease perspective. Dr. Sharma helped with statistics. All authors were involved in drafting and editing the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Level of evidence
Level III, Retrospective Cohort
The author(s) declare(s) that they had full access to all of the data in this study and the author(s) take(s) complete responsibility for the integrity of the data and the accuracy of the data analysis.
Rights and permissions
About this article
Cite this article
Singer, A.D., Umpierrez, M., Kakarala, A. et al. Performance of a rapid two-sequence screening protocol for osteomyelitis of the foot. Skeletal Radiol 49, 977–984 (2020). https://doi.org/10.1007/s00256-019-03367-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03367-x