Abstract
Objective
To describe the normal motion pattern at the midcarpal compartment during active radial–ulnar deviation of the wrist using dynamic MRI, and to determine the observer performance for measurements obtained in asymptomatic volunteers.
Methods
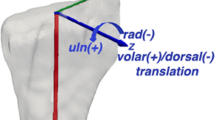
Dynamic MRI of 35 wrists in 19 asymptomatic volunteers (age mean 30.4 years, SD 8.6) was performed during active radial–ulnar deviation using a fast gradient-echo pulse sequence with 315 ms temporal resolution (acquisition time, 19 s). Two independent readers measured the transverse translation of the trapezium at the scaphotrapezium joint (STJ) and the capitate-to-triquetrum distance (CTD). Relationships between these measurements and laterality, sex, lunate type, and wrist kinematic pattern were evaluated.
Results
At the STJ, the trapezium moved most in radial deviation, with an overall translation of 2.3 mm between ulnar and radial deviation. Mean CTD measurements were the greatest in ulnar deviation and varied 2.4 mm between ulnar and radial deviation. Mean CTD was greater in men than women in the neutral position (p = 0.019), and in wrists with type II lunate morphology during radial and ulnar deviation (p = 0.001, p = 0.014). There were no significant differences in trapezium translation or CTD with wrist laterality and kinematic pattern. Intraobserver and interobserver correlation coefficients were 0.97 and 0.87 for trapezium translation and 0.84 and 0.67 for CTD.
Conclusion
This study is the first to demonstrate the performance of dynamic MRI to quantify STJ motion and CTD. Dynamic MRI with a short acquisition time may be used as a tool to supplement static MRI in evaluation of the midcarpal compartment.



Similar content being viewed by others
References
Wetherell R. Special issue: the unstable wrist. J Hand Surg Eur Vol. 2016;41(1):5–6.
Hargreaves DG. Midcarpal instability. J Hand Surg Eur Vol. 2016;41(1):86–93.
Lichtman DM, Wroten ES. Understanding midcarpal instability. J Hand Surg Am. 2006;31(3):491–8.
Mulders MAM, Sulkers GSI, Videler AJ, Strackee SD, Smeulders MJC. Long-term functional results of a wrist exercise program for patients with palmar midcarpal instability. J Wrist Surg. 2018;7(3):211–8.
Ho PC, Tse WL, Wong CW. Palmar midcarpal instability: an algorithm of diagnosis and surgical management. J Wrist Surg. 2017;6(4):262–75.
Shiga SA, Werner FW, Garcia-Elias M, Harley BJ. Biomechanical analysis of palmar midcarpal instability and treatment by partial wrist arthrodesis. J Hand Surg Am. 2018;43(4):331–338.e2.
Niacaris T, Ming BW, Lichtman DM. Midcarpal instability: a comprehensive review and update. Hand Clin. 2015;31(3):487–93.
Higgin RPC, Hargreaves DG. Midcarpal instability: the role of wrist arthroscopy. Hand Clin. 2017;33(4):717–26.
Moritomo H, Viegas SF, Elder K, Nakamura K, Dasilva MF, Patterson RM. The scaphotrapezio-trapezoidal joint. II. A kinematic study. J Hand Surg Am. 2000;25(5):911–20.
Sonenblum SE, Crisco JJ, Kang L, Akelman E. In vivo motion of the scaphotrapezio-trapezoidal (STT) joint. J Biomech. 2004;37(5):645–52.
Rainbow MJ, Wolff AL, Crisco JJ, Wolfe SW. Functional kinematics of the wrist. J Hand Surg Eur Vol. 2016;41(1):7–21.
McLean JM, Bain GI, Watts AC, Mooney LT, Turner PC, Moss M. Imaging recognition of morphological variants at the midcarpal joint. J Hand Surg Am. 2009;34(6):1044–55.
Nakamura K, Beppu M, Patterson RM, Hanson CA, Hume PJ, Viegas SF. Motion analysis in two dimensions of radial-ulnar deviation of type I versus type II lunates. J Hand Surg Am. 2000;25(5):877–88.
Malik AM, Schweitzer ME, Culp RW, Osterman LA, Manton G. MR imaging of the type II lunate bone: frequency, extent, and associated findings. AJR Am J Roentgenol. 1999;173(2):335–8.
Borgese M, Boutin RD, Bayne CO, Szabo RM, Chaudhari AJ. Association of lunate morphology, sex, and lunotriquetral interosseous ligament injury with radiologic measurement of the capitate-triquetrum joint. Skeletal Radiol. 2017;46(12):1729–37.
Harley BJ, Werner FW, Boles SD, Palmer AK. Arthroscopic resection of arthrosis of the proximal hamate: a clinical and biomechanical study. J Hand Surg Am. 2004;29(4):661–7.
Lee SK, Desai H, Silver B, Dhaliwal G, Paksima N. Comparison of radiographic stress views for scapholunate dynamic instability in a cadaver model. J Hand Surg Am. 2011;36(7):1149–57.
Sulkers GS, Strackee SD, Schep NW, Maas M. Wrist cineradiography: a protocol for diagnosing carpal instability. J Hand Surg Eur Vol. 2018;43(2):174–8.
Braunstein EM, Louis DS, Greene TL, Hankin FM. Fluoroscopic and arthrographic evaluation of carpal instability. AJR Am J Roentgenol. 1985;144(6):1259–62.
Gondim Teixeira PA, Badr S, Hossu G, et al. Quantitative analysis of scapholunate diastasis using stress speckle-tracking sonography: a proof-of-concept and feasibility study. Eur Radiol. 2017;27(12):5344–51.
Abou Arab W, Rauch A, Chawki MB, et al. Scapholunate instability: improved detection with semi-automated kinematic CT analysis during stress maneuvers. Eur Radiol. 2018;28(10):4397–406.
Mat Jais IS, Tay SC. Kinematic analysis of the scaphoid using gated four-dimensional CT. Clin Radiol. 2017;72(9):794.e1–9.
Demehri S, Hafezi-Nejad N, Morelli JN, et al. Scapholunate kinematics of asymptomatic wrists in comparison with symptomatic contralateral wrists using four-dimensional CT examinations: initial clinical experience. Skeletal Radiol. 2016;45(4):437–46.
Boutin RD, Buonocore MH, Immerman I, Ashwell Z, Sonico GJ, Szabo RM, et al. Real-time magnetic resonance imaging (MRI) during active wrist motion—initial observations. PLoS One. 2013;8(12):e84004.
Langner I, Fischer S, Eisenschenk A, Langner S. Cine MRI: a new approach to the diagnosis of scapholunate dissociation. Skeletal Radiol. 2015;44(8):1103–10.
Borotikar B, Lempereur M, Lelievre M, Burdin V, Ben Salem D, Brochard S. Dynamic MRI to quantify musculoskeletal motion: a systematic review of concurrent validity and reliability, and perspectives for evaluation of musculoskeletal disorders. PLoS One. 2017;12(12):e0189587.
Garcia-Elias M, Ribe M, Rodriguez J, Cots M, Casas J. Influence of joint laxity on scaphoid kinematics. J Hand Surg Br. 1995;20(3):379–82.
Cicchetti DV. Guidelines, criteria, and rules of thumb for evaluating normed and standardized assessment instruments in psychology. Psychol Assess. 1994;6(4):284–90.
Yukioka C, Arimitsu S, Moritomo H. Three-dimensional kinematic analysis of a scaphoid-trapezium coalition: a case report. J Hand Surg Eur Vol. 2016;41(5):554–5.
Pegoli L, Pozzi A, Pivato G, Luchetti R. Arthroscopic resection of distal pole of the scaphoid for scaphotrapeziotrapezoid joint arthritis: comparison between simple resection and implant interposition. J Wrist Surg. 2016;5(3):227–32.
McLean JM, Turner PC, Bain GI, Rezaian N, Field J, Fogg Q. An association between lunate morphology and scaphoid-trapezium-trapezoid arthritis. J Hand Surg Eur Vol. 2009;34(6):778–82.
Scordino LE, Bernstein J, Nakashian M, et al. Radiographic prevalence of scaphotrapeziotrapezoid osteoarthrosis. J Hand Surg Am. 2014;39(9):1677–82.
Tay SC, Moran SL, Shin AY, Linscheid RL. The clinical implications of scaphotrapezium-trapezoidal arthritis with associated carpal instability. J Hand Surg Am. 2007;32(1):47–54.
Kapoutsis DV, Dardas A, Day CS. Carpometacarpal and scaphotrapeziotrapezoid arthritis: arthroscopy, arthroplasty, and arthrodesis. J Hand Surg Am. 2011;36(2):354–66.
Kim BJ, Kovacevic D, Lee YM, Seol JH, Kim MS. The role of lunate morphology on scapholunate instability and fracture location in patients treated for scaphoid nonunion. Clin Orthop Surg. 2016;8(2):175–80.
Dimitriadis A, Paraskevas G, Kanavaros P, Barbouti A, Vrettakos A, Kitsoulis P. Association between the capitate-triquetrum distance and carpal collapse in static scapholunate instability. Acta Orthop Belg. 2018;84(1):68–72.
Park JH, Jang WY, Kwak DH, Park JW. Lunate morphology as a risk factor of idiopathic ulnar impaction syndrome. Bone Joint J. 2017;99-B(11):1508–14.
Andersson JK. Treatment of scapholunate ligament injury: current concepts. EFORT Open Rev. 2017;2(9):382–93.
Watson HK, Sorelle JR, Wollstein R, EAL H. STT arthrodesis. In: Gelberman RH, editor. Master techniques in orthopaedic surgery: the wrist. Philadelphia: Lippincott Williams & Wilkins; 2012. p. 263–70.
Farr S, Schachinger F, Girsch W. Palmar capsuloligamentous plication in dorsal capitolunate instability: technique and preliminary results. Tech Hand Up Extrem Surg. 2019;23(1):22–6.
Von Schroeder HP. Dorsal wrist plication for midcarpal instability. J Hand Surg Am. 2018;43(4):354–9.
Shunmugam M, Phadnis J, Watts A, Bain GI. Lunate fractures and associated radiocarpal and midcarpal instabilities: a systematic review. J Hand Surg Eur Vol. 2018;43(1):84–92.
Kane PM, Vopat BG, Mansuripur PK, et al. Relative contributions of the midcarpal and radiocarpal joints to dart-thrower's motion at the wrist. J Hand Surg Am. 2018;43(3):234–40.
McNary SM, Heyrani N, Volk I, Szabo RM, Bayne CO. The effect of radioscapholunate fusion with and without distal scaphoid and triquetrum excision on capitolunate contact pressures. J Hand Surg Am. 2019;44(5):420.e1–7.
Dimitris C, Werner FW, Joyce DA, Harley BJ. Force in the scapholunate interosseous ligament during active wrist motion. J Hand Surg Am. 2015;40(8):1525–33.
De Roo MGA, Muurling M, Dobbe JGG, Brinkhorst ME, Streekstra GJ, Strackee SD. A four-dimensional-CT study of in vivo scapholunate rotation axes: possible implications for scapholunate ligament reconstruction. J Hand Surg Eur Vol. 2019;44(5):479–87.
Kelly PM, Hopkins JG, Furey AJ, Squire DS. Dynamic CT scan of the normal scapholunate joint in a clenched fist and radial and ulnar deviation. Hand (N Y). 2018;13(6):666–70.
Kakar S, Breighner RE, Leng S, et al. The role of dynamic (4D) CT in the detection of scapholunate ligament injury. J Wrist Surg. 2016;5(4):306–10.
Carr R, MacLean S, Slavotinek J, Bain GI. Four-dimensional computed tomography scanning for dynamic wrist disorders: prospective analysis and recommendations for clinical utility. J Wrist Surg. 2019;8(2):161–7.
Foster BH, Shaw CB, Boutin RD, et al. A principal component analysis-based framework for statistical modeling of bone displacement during wrist maneuvers. J Biomech. 2019;85:173–81.
Acknowledgements
The authors gratefully acknowledge the assistance of John Brock in assisting with IRB compliance, Julie Ostoich-Prather in assisting with graphic design, in addition to Gerald Sonico, B.S., Costin Tanase, PhD, and Sinyeob Ahn, PhD in assisting with optimizing real-time pulse sequence parameters.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Grant support
National Institutes of Health (K12 HD051958 and R03 EB015099) to Abhijit J. Chaudhari, and National Science Foundation (GRFP Grant No. 1650042) to Brent Foster.
Conflicts of interest
The authors declare that they have no related conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Henrichon, S.S., Foster, B.H., Shaw, C. et al. Dynamic MRI of the wrist in less than 20 seconds: normal midcarpal motion and reader reliability. Skeletal Radiol 49, 241–248 (2020). https://doi.org/10.1007/s00256-019-03266-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00256-019-03266-1