Abstract
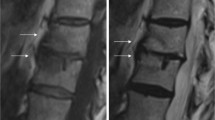
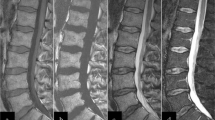
The paediatric metaphysis is afflicted by a wide range of pathological processes as it is the most metabolically active and well-vascularised part of the developing skeleton. This review focuses on metaphyseal marrow signal change detected with magnetic resonance imaging, which is most often occult on radiographs. When bilateral, these imaging appearances frequently present a diagnostic quandary. This review assists the radiologist to confidently dismiss physiological signal change and confidently work through the differential diagnosis. This is achieved by illustrating a practical method of classifying signal change into four categories: physiological red marrow, red marrow reconversion, marrow infiltration, and oedema-like marrow signal intensity. In doing so, various pathological entities are reviewed along with imaging pearls and next-step investigations.
Graphical abstract


















Similar content being viewed by others
References
Laor T, Jaramillo D (1993) Metaphyseal abnormalities in children: pathophysiology and radiologic appearance. AJR Am J Roentgenol 161:1029–1036
Chan BY, Gill KG, Rebsamen SL, Nguyen JC (2016) MR imaging of pediatric bone marrow. Radiographics 36:1911–1930
Zadig PK, von Brandis E, Flatø B et al (2022) Whole body magnetic resonance imaging in healthy children and adolescents: bone marrow appearances of the appendicular skeleton. Eur J Radiol 153:110365
Laor T, Jaramillo D (2009) MR imaging insights into skeletal maturation: what is normal? Radiology 250:28–38
Person A, Janitz E, Thapa M (2021) Pediatric bone marrow: normal and abnormal MRI appearance. Semin Roentgenol 56:325–337
Nguyen JC, Markhardt BK, Merrow AC, Dwek JR (2017) Imaging of pediatric growth plate disturbances. Radiographics 37:1791–1812
Augusto ACL, Goes PCK, Flores DV et al (2022) Imaging review of normal and abnormal skeletal maturation. Radiographics 42:861–879
Vande Berg BC, Malghem J, Lecouvet FE, Maldague B (1998) Magnetic resonance imaging of the normal bone marrow. Skeletal Radiol 27:471–483
Małkiewicz A, Dziedzic M (2012) Bone marrow reconversion - imaging of physiological changes in bone marrow. Pol J Radiol 77:45–50
Fletcher BD (1997) Effects of pediatric cancer therapy on the musculoskeletal system. Pediatr Radiol 27:623–636
Ryan SP, Weinberger E, White KS et al (1995) MR imaging of bone marrow in children with osteosarcoma: effect of granulocyte colony-stimulating factor. AJR Am J Roentgenol 165:915–920
Altehoefer C, Bertz H, Ghanem NA, Langer M (2001) Extent and time course of morphological changes of bone marrow induced by granulocyte-colony stimulating factor as assessed by magnetic resonance imaging of healthy blood stem cell donors. J Magn Reson Imaging 14:141–146
Gu L, Madewell JE, Aslam R, Mujtaba B (2019) The effects of granulocyte colony-stimulating factor on MR images of bone marrow. Skeletal Radiol 48:209–218
Shellock FG, Morris E, Deutsch AL et al (1992) Hematopoietic bone marrow hyperplasia: high prevalence on MR images of the knee in asymptomatic marathon runners. AJR Am J Roentgenol 158:335–338
Disler DG, McCauley TR, Ratner LM et al (1997) In-phase and out-of-phase MR imaging of bone marrow: prediction of neoplasia based on the detection of coexistent fat and water. AJR Am J Roentgenol 169:1439–1447
Akman B, Ata Korkmaz HA, Sarı A (2019) Efficacy of chemical shift MRI for differentiating diffuse red bone marrow reconversion and hematological malignancies. Turk J Med Sci 49:644–652
Winfeld M, Ahlawat S, Safdar N (2016) Utilization of chemical shift MRI in the diagnosis of disorders affecting pediatric bone marrow. Skeletal Radiol 45:1205–1212
Maraghelli D, Brandi ML, Matucci Cerinic M et al (2021) Edema-like marrow signal intensity: a narrative review with a pictorial essay. Skeletal Radiol 50:645–663
Chaturvedi A (2021) Pediatric skeletal diffusion-weighted magnetic resonance imaging, part 2: current and emerging applications. Pediatr Radiol 51:1575–1588
Khoo MM, Tyler PA, Saifuddin A, Padhani AR (2011) Diffusion-weighted imaging (DWI) in musculoskeletal MRI: a critical review. Skeletal Radiol 40:665–681
Raissaki M, Demetriou S, Spanakis K et al (2017) Multifocal bone and bone marrow lesions in children - MRI findings. Pediatr Radiol 47:342–360
Zaveri J, La Q, Yarmish G et al (2014) More than just Langerhans cell histiocytosis: a radiological review of histiocytic disorders. Radiographics 34:2008–2024
Stull MA, Kransdorf MJ, Devaney KO (1992) Langerhans cell histiocytosis of bone. Radiographics 12:801–823
Gorbachova T, Amber I, Beckmann NM et al (2019) Nomenclature of subchondral nonneoplastic bone lesions. AJR Am J Roentgenol 213:963–982
Saifuddin A, Tyler P, Rajakulasingam R (2023) Imaging of bone marrow pitfalls with emphasis on MRI. Br J Radiol 96:20220063
Offiah AC (2006) Acute osteomyelitis, septic arthritis and discitis: differences between neonates and older children. Eur J Radiol 60:221–232
Browne LP, Guillerman RP, Orth RC et al (2012) Community-acquired staphylococcal musculoskeletal infection in infants and young children: necessity of contrast-enhanced MRI for the diagnosis of growth cartilage involvement. AJR Am J Roentgenol 198:194–199
Jaramillo D, Dormans JP, Delgado J et al (2017) Hematogenous osteomyelitis in infants and children: imaging of a changing disease. Radiology 283:629–643
Resnik R, Lockwood C, Moore T et al (2019) Creasy and Resnik’s maternal-fetal medicine: principles and practice, 8th edn. Elsevier, Philadelphia
Sebag GH (1998) Disorders of the hip. Magn Reson Imaging Clin N Am 6:627–641
Simpson WL, Hermann G, Balwani M (2014) Imaging of Gaucher disease. World J Radiol 26:657–668
Skaggs DL, Kim SK, Greene NW et al (2001) Differentiation between bone infarction and acute osteomyelitis in children with sickle-cell disease with use of sequential radionuclide bone-marrow and bone scans. J Bone Joint Surg Am 83:1810–1813
Solomon N, Segaran N, Badawy M et al (2022) Manifestations of sickle cell disorder at abdominal and pelvic imaging. Radiographics 42:1103–1122
Khanna G, Sato TS, Ferguson P (2009) Imaging of chronic recurrent multifocal osteomyelitis. Radiographics 29:1159–1177
Mandell G, Contreras SJ, Conard K et al (1998) Bone scintigraphy in the detection of chronic recurrent multifocal osteomyelitis. J Nucl Med 39:1778–1783
de Horatio LT, Casazza I, Savelli S et al (2015) Chronic recurrent multifocal osteomyelitis (CRMO): typical patterns of bone involvement on MRI with particular emphasis on whole body MRI (WBMRI). Pediatr Rheumatol. https://doi.org/10.1186/1546-0096-13-S1-P53
Schaal MC, Gendler L, Ammann B et al (2021) Imaging in non-bacterial osteomyelitis in children and adolescents: diagnosis, differential diagnosis and follow-up-an educational review based on a literature survey and own clinical experiences. Insights Imaging. https://doi.org/10.1186/s13244-021-01059-6
Zulian F, Marigo E, Ardenti-Morini F et al (2021) Osteoperiostitis in children: proposal for a diagnostic algorithm. Eur J Pediatr 180:3229–3235
Taddio A, Ferrara G, Insalaco A et al (2017) Dealing with chronic non-bacterial osteomyelitis: a practical approach. Pediatr Rheumatol Online J. https://doi.org/10.1186/s12969-017-0216-7
Musa H, Ismail II, Abdul Rashid NH (2021) Paediatric scurvy: frequently misdiagnosed. Paediatr Int Child Health 41:158–161
Ganske A, Kolbe AB, Thomas K, Hull N (2021) Pediatric Scurvy MRI appearance. Radiol Case Rep 16:1148–1152
Chang CY, Rosenthal DI, Mitchell DM et al (2016) Imaging findings of metabolic bone disease. Radiographics 36:1871–1887
Abbas F, Ha LD, Sterns R, von Doenhoff L (2016) Reversible right heart failure in scurvy rediscovery of an old observation. Circ Heart Fail. https://doi.org/10.1161/CIRCHEARTFAILURE.116.003497
Abe K, Kibe R, David K et al (2021) Reversible right-sided heart failure and pulmonary hypertension caused by scurvy in a 7-year-old boy with autism spectrum disorder and a review of the literature. Paediatr Int Child Health 25:1–5
Rethore S, Leblond P, Thebaud E et al (2011) Unusual presentation of scurvy mimicking a neuroblastoma. Arch Pediatr 18:37–40. French
Mannes I, Rothenbuhler A, Merzoug V et al (2022) Imaging patterns in pediatric hypophosphatasia. Pediatr Radiol 52:998–1006
Author information
Authors and Affiliations
Contributions
All authors contributed to the essay conception and design. The first and revised drafts of the manuscript were written by S.B. and all authors commented and edited previous versions of the manuscript. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Booth, S.M., Kapadia, T.H., Tang, V. et al. Pictorial review: challenges in distinguishing bilateral metaphyseal marrow abnormalities on magnetic resonance imaging. Pediatr Radiol (2024). https://doi.org/10.1007/s00247-024-05896-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00247-024-05896-7