Abstract
Background
The diagnosis of adolescent idiopathic scoliosis requires clinical and radiographic evaluation; the management options vary depending on the severity of the curve and potential for progression. Identifying predictors of scoliosis progression is crucial to avoid incorrect management; clinical and radiographic factors have been studied as potential predictors. The present study aims to review the literature on radiological indexes for the peak height velocity or curve acceleration phase to help clinicians manage treatment of patients with adolescent idiopathic scoliosis.
Methods
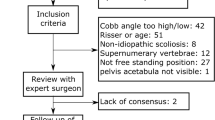
This systematic review was carried out in accordance with Preferential Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) guidelines. The search was carried out including only peer-reviewed articles written in English that described the radiological indexes assessing skeletal maturity in patients with adolescent idiopathic scoliosis and evaluated their correlation with curve progression, expressed as peak height velocity and/or curve acceleartion phase.
Results
Thirteen studies were included and showed promising results in terms of reliable radiological indexes. Risser staging gives a general measure of skeletal maturity, but it cannot be used as a primary index for driving the treatment of patients with adolescent idiopathic scoliosis since more reliable indexes are available.
Conclusion
Skeletal maturity quantification for adolescent idiopathic scoliosis has the potential to significantly modify disease management. However, idiopathic scoliosis is a complex and multifactorial disease: therefore, it is unlikely that a single index will ever be sufficient to predict its evolution. Therefore, as more adolescent idiopathic scoliosis progression-associated indexes are identified, a collective scientific effort should be made to develop a therapeutic strategy based on reliable and reproducible algorithms.







Similar content being viewed by others
Data availability
The data that support the findings of this study are available from the corresponding author, [M.M.], upon reasonable request.
Change history
05 February 2024
A Correction to this paper has been published: https://doi.org/10.1007/s00247-024-05871-2
References
Faldini C, Perna F, Geraci G et al (2018) Triplanar correction of adolescent idiopathic scoliosis by asymmetrically shaped and simultaneously applied rods associated with direct vertebral rotation: clinical and radiological analysis of 36 patients. Eur Spine J 27:165–174
Barile F, Ruffilli A, Manzetti M et al (2021) Resumption of sport after spinal fusion for adolescent idiopathic scoliosis: a review of the current literature. Spine Deform 9:1247–1251
Konieczny MR, Senyurt H, Krauspe R (2013) Epidemiology of adolescent idiopathic scoliosis. J Child Orthop 7:3–9
Lonstein JE (1994) Adolescent idiopathic scoliosis. Lancet 344:1407–1412
Lonstein JE, Carlson JM (1984) The prediction of curve progression in untreated idiopathic scoliosis during growth. J Bone Jt Surg - Ser A 66:1061–1071
Sanders JO, Khoury JG, Kishan S et al (2008) Predicting scoliosis progression from skeletal maturity: a simplified classification during adolescence. J Bone Jt Surg 90:540–553
Negrini S, Donzelli S, Aulisa AG, et al (2018) 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 13:3. https://doi.org/10.1186/s13013-017-0145-8
Pérez-Machado G, Berenguer-Pascual E, Bovea-Marco M et al (2020) From genetics to epigenetics to unravel the etiology of adolescent idiopathic scoliosis. Bone 140:115563. https://doi.org/10.1016/j.bone.2020.115563
García-Cano E, Arámbula Cosío F, Duong L et al (2018) Prediction of spinal curve progression in adolescent idiopathic scoliosis using random forest regression. Comput Biol Med 103:34–43
Faldini C, Manzetti M, Neri S et al (2022) Epigenetic and Genetic Factors Related to Curve Progression in Adolescent Idiopathic Scoliosis: A Systematic Scoping Review of the Current Literature. Int J Mol Sci. 23(11):5914. https://doi.org/10.3390/ijms23115914
Nault ML, Parent S, Phan P et al (2010) A modified risser grading system predicts the curve acceleration phase of female adolescent idiopathic scoliosis. J Bone Jt Surg 92:1073–1081
Cheung PWH, Canavese F, Chan CYW et al (2022) The utility of a novel proximal femur maturity index for staging skeletal growth in patients with idiopathic scoliosis. J Bone Jt Surg 104:630–640
Cheung JPY, Cheung PWH, Samartzis D, Luk KDK (2018) Curve progression in adolescent idiopathic scoliosis does not match skeletal growth. Clin Orthop Relat Res 476:429–436
Hung ALH, Chau WW, Shi B et al (2017) Thumb ossification composite index (TOCI) for predicting peripubertal skeletal maturity and peak height velocity in idiopathic scoliosis. J Bone Jt Surg - Am 99:1438–1446
Sanders JO, Browne RH, McConnell SJ et al (2007) Maturity assessment and curve progression in girls with idiopathic scoliosis. J Bone Jt Surg 89:64–73
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372. https://doi.org/10.1136/BMJ.N71
Howick J, Chalmers I, Glasziou P et al (2011) The Oxford 2011 Levels of Evidence. Oxford Centre Evidence-Based Medicine. In: Group. http://www.cebm.net/index.aspx?o=5653
Sideri S, Papageorgiou SN, Eliades T (2018) Registration in the international prospective register of systematic reviews (PROSPERO) of systematic review protocols was associated with increased review quality. J Clin Epidemiol 100:103–110
Little DG, Song KM, Katz D, Herring JA (2000) Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J Bone Jt Surg 82:685–693
Sitoula P, Verma K, Holmes L et al (2015) Prediction of curve progression in idiopathic scoliosis: validation of the sanders skeletal maturity staging system. Spine (Phila Pa 1976) 40:1006–1013
Cheung JPY, Cheung PWH, Samartzis D et al (2016) The use of the distal radius and ulna classification for the prediction of growth peak growth spurt and growth cessation. Bone Jt J 98-B:1689–1696
Shi B, Mao S, Xu L et al (2017) Integrated multidimensional maturity assessments predicting the high-risk occurrence of peak angle velocity during puberty in progressive female idiopathic scoliosis. Clin Spine Surg 30:E491–E496
Neal KM, Shirley ED, Kiebzak GM (2018) Maturity indicators and adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 43:E406–E412
Cheung PWH, Mannem A, Cheung JPY (2021) Prediction of final body height for female patients with adolescent idiopathic scoliosis. Glob Spine J 11:833–844
Chazono M, Obata S (2021) A simplified skeletal maturity scale and thumb ossification composite index to assess skeletal maturity and predict height velocity in japanese females with adolescent idiopathic scoliosis. Spine Surg Relat Res 5:244–251
NIH National Heart, Lung and Blood Institute. Study quality assessment tools [cited 2022, May 12]. Available from: https://www.nhlbi.nih.gov/health-topics/assessing-cardiovascular-risk
Song KM, Little DG (2000) Peak height velocity as a maturity indicator for males with idiopathic scoliosis. J Pediatr Orthop 20:286–288
Risser JC, Ferguson AB (1936) Scoliosis: its prognosis. J Bone Jt Surg 18:667–670
Luk KDK, Saw LB, Grozman S et al (2014) Assessment of skeletal maturity in scoliosis patients to determine clinical management: a new classification scheme using distal radius and ulna radiographs. Spine J 14:315–325
SRS (2016) SRS Bracing Manual | Scoliosis Research Society. https://www.srs.org/professionals/online-education-and-resources/srs-bracing-manual. Accessed 14 May 2023
Charles YP, Diméglio A, Canavese F, Daures JP (2007) Skeletal age assessment from the olecranon for idiopathic scoliosis at risser grade 0. J Bone Jt Surg 89 A:2737–2744
Ryan PM, Puttler EG, Stotler WM, Ferguson RL (2007) Role of the triradiate cartilage in predicting curve progression in adolescent idiopathic scoliosis. J Pediatr Orthop 27:671–676
Cheung PWH, Cheung JPY (2021) Does the use of sanders staging and distal radius and ulna classification avoid mismatches in growth assessment with Risser staging alone? Clin Orthop Relat Res 479:2516–2530
Izumi Y (1995) The accuracy of Risser staging. Spine (Phila Pa 1976) 20:1868–1871
Kotwicki T (2008) Risser sign: the value of the lateral spinal radiograph to assess the excursion of the iliac apophysis. Stud Health Technol Inform 140:44–47
Kotwicki T (2008) Improved accuracy in Risser sign grading with lateral spinal radiography. 17:1676–1685
Verma K, Sitoula P, Gabos P et al (2014) Simplified skeletal maturity scoring system: learning curve and methods to improve reliability. Spine (Phila Pa 1976) 39:E1592–E1598
Akpolat AO, Gültekin O, Kılınç BE et al (2021) Does the choice of the growth potential classification affect the non-surgical treatment of the adolescent idiopathic scoliosis? İstanbul Kanuni Sultan Süleyman Tıp Derg 13:123–128
Vira S, Husain Q, Jalai C et al (2017) The interobserver and intraobserver reliability of the Sanders classification versus the Risser stage. J Pediatr Orthop 37:e246–e249
Jackson TJ, Miller D, Nelson S et al (2018) Two for one: a change in hand positioning during low-dose spinal stereoradiography allows for concurrent, reliable Sanders skeletal maturity staging. Spine Deform 6:391–396
Luan FJ, Wan Y, Mak KC et al (2020) Cancer and mortality risks of patients with scoliosis from radiation exposure: a systematic review and meta-analysis. Eur Spine J 29:3123–3134
Simony A, Hansen EJ, Christensen SB et al (2016) Incidence of cancer in adolescent idiopathic scoliosis patients treated 25 years previously. Eur Spine J 25:3366–3370
Marshall WA, Tanner JM (1970) Variations in pattern of pubertal changes in girls. Obstet Gynecol Surv 25:694–696
Sanders JO, Qiu X, Lu X et al (2017) The uniform pattern of growth and skeletal maturation during the human adolescent growth spurt. Sci Rep 7:1–9
Diméglio A, Charles YP, Daures JP et al (2005) Accuracy of the Sauvegrain method in determining skeletal age during puberty. J Bone Jt Surg 87:1689–1696
Sanders JO, Browne RH, Cooney TE et al (2006) Correlates of the peak height velocity in girls with idiopathic scoliosis. Spine (Phila Pa 1976) 31:2289–2295. https://doi.org/10.1097/01.brs.0000236844.41595.26
Marshall WA (1981) Geographical and ethnic variations in human growth. Br Med Bull 37:273–279
Natale V, Rajagopalan A (2014) Worldwide variation in human growth and the World Health Organization growth standards: a systematic review. BMJ Open 4
Mittal M, Gupta P, Kalra S et al (2021) Short stature: understanding the stature of ethnicity in height determination. Indian J Endocrinol Metab 25:381–388
Hirschhorn JN, Lettre G (2009) Progress in genome-wide association studies of human height. Horm Res 71:5–13
Allen H, Estrada K, Lettre G (2010) Hundreds of variants influence human height and cluster within genomic loci and biological pathways. … Genet Var …
Gibran H, Jian Y, Anna V et al (2013) Inference of the genetic architecture underlying BMI and height with the use of 20,240 sibling pairs. Am J Hum Genet 93:865–875
Pemberton TJ, Verdu P, Becker NS et al (2018) A genome scan for genes underlying adult body size differences between Central African hunter-gatherers and farmers. Hum Genet 137:487–509
Cheung JPY, Cheung PWH, Luk KDK (2019) When should we wean bracing for adolescent idiopathic scoliosis? Clin Orthop Relat Res 477:2145–2157
Grothaus O, Molina D, Jacobs C et al (2020) Is it growth or natural history? Increasing spinal deformity after Sanders Stage 7 in females with AIS. J Pediatr Orthop 40:E176–E181
Li DT, Linderman GC, Cui JJ et al (2019) The proximal humeral ossification system improves assessment of maturity in patients with scoliosis. J Bone Jt Surg - Am 101:1868–1874
Thodberg HH, Thodberg B, Ahlkvist J, Offiah AC (2022) Autonomous artificial intelligence in pediatric radiology: the use and perception of BoneXpert for bone age assessment. Pediatr Radiol 52:1338–1346
Funding
This work was funded by CRUI-CARE and CNR Compact agreement and Alma Mater Studiorum - University of Bologna as a participating institution.
Author information
Authors and Affiliations
Contributions
Conceptualization: M.M.; data curation: M.M., F.B., and V.V.; formal analysis: M.M., E.A., and A.A.; investigation: M.M., A.M., and T.C.; project administration: C. and A.R.; resources, F.B., M. M., and M.T.; supervision: C.F., A.R., and A.M.; validation: M.M.; visualization: M.M. and G.V.; writing original draft: M.M., G.V., and F.B.; writing, review, and editing: F.B., M.M., A.R., and A. M. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Ethical approval and institutional review board approval were not required for this synthesis of data from published studies.
Informed consent
Informed consent was not required for this synthesis of data from published studies.
Conflicts of interest
None
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: The original article contains a spelling error in author name. The author “Alberto Arcieri” should read as “Alberto Arceri”.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Manzetti, M., Ruffilli, A., Barile, F. et al. Is there a skeletal age index that can predict accurate curve progression in adolescent idiopathic scoliosis? A systematic review. Pediatr Radiol 54, 299–315 (2024). https://doi.org/10.1007/s00247-023-05834-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05834-z