Abstract
Background
While large-bore mechanical thrombectomy provides effective venous thrombus removal, often with avoidance of thrombolytics, literature surrounding the application of these devices in pediatric patients is sparse.
Objective
To report technical success and outcomes following large-bore thrombectomy systems in adolescent patients with deep venous thrombosis.
Materials and Methods
A retrospective review identified all patients less than 18 years of age undergoing mechanical venous thrombectomy at a single institution between 2018 and 2022. No patients were excluded. Technical success was defined as extraction of thrombus sufficient to restore unimpeded flow in affected segments. Clinical success was defined as resolution of presenting symptoms.
Results
Nine consecutive patients (6 females, 3 males; age range 15–17 years) underwent 10 thrombectomy procedures using ClotTriever (n=6; 60%), FlowTriever (n=2; 20%), or both (n=2; 20%). Chronicity of thrombus was categorized as acute (<2 weeks) in 6 (60%), subacute (2–6 weeks) in 1 (10%), and chronic (>6 weeks) in 3 (30%). Distribution of thrombus was lower extremity and/or inferior vena cava (IVC) in 9 (90%) and unilateral axillo-subclavian in 1 (10%). Technical success was achieved in 9 interventions (90%). Clinical success was achieved in 8 patients (88.9%). No patients received thrombolytics. There were no intraprocedural adverse events (AE). Minor complications (Society of Interventional Radiology mild adverse events) were observed in a delayed fashion following 2 interventions (20%).
Conclusions
This preliminary experience demonstrated high rates of technical and clinical success with large-bore deep venous thrombectomy in adolescent patients across a range of thrombus chronicity and locations.
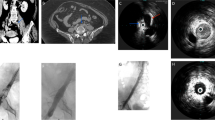
Graphical Abstract



Similar content being viewed by others
Data availability
The data generated during the study are available from the corresponding author on reasonable request.
References
Jaffray J, Young G (2018) Deep vein thrombosis in pediatric patients. Pediatr Blood Cancer 65:e26881
Benarroch-Gampel J, Pujari A, Aizpuru M et al (2020) Technical success and short-term outcomes after treatment of lower extremity deep vein thrombosis with the ClotTriever system: A preliminary experience. J Vasc Surg Venous Lymphat Disord 8:174–181
Greenberg C, Shin DS, Abad-Santos M et al (2022) Endovascular Tissue Sampling Using the ClotTriever Thrombectomy System: Histopathologic Analysis in 26 Consecutive Patients. CardioVasc Intervent Radiol 45:898–901
Bertino FJ, Shin DS, Monroe EJ et al (2021) Thrombectomy of Malignant Thoracic Central Venous Occlusive Disease Using Inari ClotTriever System. J Vasc Interv Radiol 32:1398–1400
Khalilzadeh O, Baerlocher MO, Shyn PB et al (2017) Proposal of a new adverse event classification by the Society of Interventional Radiology Standards of Practice Committee. J Vasc Intervent Radiol 28:1432–1437
Shin DS, Abad-Santos M, Kuyumcu G et al (2023) Embolic Protection During Malignant Inferior Vena Caval Thrombectomy Using the Protrieve Sheath. CardioVasc Intervent Radiol 46:535–537
Eksioglu AS, Yildiz YT, Senel S (2014) Normal sizes of internal jugular veins in children/adolescents aged birth to 18 years at rest and during the Valsalva maneuver. Eur J Radiol 83:673–679
Tadphale SD, Zurakowski D, Bird LE et al (2020) Construction of femoral vessel nomograms for planning cardiac interventional procedures in children 0–4 years old. Pediatr Cardiol 41:1135–1144
Kutty S, Li L, Hasan R, Peng Q et al (2014) Systemic venous diameters, collapsibility indices, and right atrial measurements in normal pediatric subjects. J Am Soc Echocardiogr 27:155–162
Shin DS, Monroe EJ, Hua EW et al (2023) Single Sweep Transjugular Thrombectomy (Declot) of a Hemodialysis Graft Using the InThrill Thrombectomy System. CardioVasc Intervent Radiol 6:1–3
Sharathkumar AA, Pipe SW (2008) Post-thrombotic syndrome in children: a single center experience. J Pediatr Hematol 30:261–266
Goldenberg NA, Donadini MP, Kahn SR et al (2010) Post-thrombotic syndrome in children: a systematic review of frequency of occurrence, validity of outcome measures, and prognostic factors. Haematologica 95:1952–1959
Funding
This study was not supported by any funding. This study was conducted with institutional review board approval and complied with the Health Insurance Portability and Accountability Act. Informed consent was waived for retrospective, no patient contact methodology. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Contributions
E.J.M. and M.A.W. conceived the study, collated and analyzed the data, and drafted the manuscript. All authors contributed to, reviewed, and approved the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
E.J.M. is a scientific advisor and speaker for Biogen. J.F.B.C. is a consultant and speaker for Inari Medical, Guerbet, C. R. Bard, Argon Medical Devices, Boston Scientific, and NXT Biomedical. None of the other authors have identified a conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Monroe, E.J., Woods, M.A., Shin, D.S. et al. Percutaneous treatment of symptomatic deep vein thrombosis in adolescents using large-bore thrombectomy systems. Pediatr Radiol 53, 2692–2698 (2023). https://doi.org/10.1007/s00247-023-05785-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05785-5