Abstract
Background
When postoperative multi-slice computed tomography (MSCT) imaging of patients with craniosynostosis is used, it is usually performed a few days after surgery in a radiology department. This requires additional anesthesia for the patient. Recently, intraoperative mobile cone-beam CT (CBCT) devices have gained popularity for orthopedic and neurosurgical procedures, which allows postoperative CT imaging in the operating room.
Objective
This single-center retrospective study compared radiation dose and image quality of postoperative imaging performed using conventional MSCT scanners and O-arm CBCT.
Materials and methods
A total of 104 pediatric syndromic and non-syndromic patients who were operated on because of single- or multiple-suture craniosynostosis were included in this study. The mean volumetric CT dose index (CTDIvol) and dose-length product (DLP) values of optimized craniosynostosis CT examinations (58 MSCT and 46 CBCT) were compared. Two surgeons evaluated the subjective image quality.
Results
CBCT resulted in significantly lower CTDIvol (up to 14%) and DLP (up to 33%) compared to MSCT. Multi-slice CT image quality was considered superior to CBCT scans. However, all scans were considered to be of sufficient quality for diagnosis.
Conclusion
The O-arm device allowed for an immediate postoperative CBCT examination in the operating theater using the same anesthesia induction. Radiation exposure was lower in CBCT compared to MSCT scans, thus further encouraging the use of O-arms. Cone-beam CT imaging with an O-arm is a feasible method for postoperative craniosynostosis imaging, yielding less anesthesia to patients, lower health costs and the possibility to immediately evaluate results of the surgical operation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Craniosynostosis is a disturbance in head and skull development in which premature fusion of one or more cranial sutures results in abnormal skull growth [1, 2]. The prevalence of craniosynostosis is 3.1 to 7.2 per 10,000 live births [3,4,5]. Early diagnosis and surgical management are essential for craniosynostosis patients to achieve acceptable clinical outcomes and to reduce the number of recurrent surgical interventions. Surgical procedures allow the brain to grow and expand normally and improve the esthetics and function of the craniofacial region [6]. Untreated craniosynostosis typically leads to ongoing deformity and sometimes an increase in intracranial pressure with possible neurological consequences [2, 7].
Currently, multi-slice computed tomography (MSCT) imaging is widely used together with cranial X-ray imaging, ultrasound and magnetic resonance imaging (MRI) for the diagnosis and follow-up of craniosynostosis patients. The sutures of the calvaria and the skull base are most accurately identified on axial and 3-dimensional (D) surface-rendered CT images, which is currently considered the gold standard in the radiological diagnosis of craniosynostosis [8,9,10]. Preoperative CT images are used to confirm clinical diagnosis, assess structural anomalies and neurovascular anatomy and facilitate accurate surgical planning [10, 11]. Postoperatively, CT images can be used to detect possible complications and evaluate the surgical outcome and adequacy of calvarial expansion [10, 11]. Additionally, postoperative evaluation is beneficial for the assessment of new surgical techniques and in medicolegal disputes. As the contrast of the skull compared to the cranial soft tissues is higher than the contrast between cranial soft tissues, CT examinations of the skull can be performed with a significantly lower radiation level than that of routine head CT scans. This is highly important as the entire diagnostic chain in craniosynostosis typically includes repeated CT examinations (pre- and postoperative) with associated exposure to ionizing radiation, which is harmful to health [12, 13]. In addition to longer life expectancy, children are also more radiosensitive than adults, which increases the requirement for dose optimization [14, 15]. Depending on the level of exposure, radiation from CT imaging increases brain cancer risk in children up to five fold [16]. When postoperative CT scans for craniosynostosis are used, these are typically performed a few days after surgery in the radiology department. This requires an additional anesthesia for the patient, which increases healthcare costs and risks. Recently, 3-D intraoperative cone-beam CT (CBCT) imaging performed either with a mobile C-arm or an O-arm has become increasingly common, especially for orthopedic and neurosurgical procedures. This provides possibilities not only for intraoperative but also for postoperative CT scans in the operating theater [17,18,19,20,21,22,23].
Replacing a conventional MSCT examination performed in the radiology department with a time- and cost-effective CBCT examination performed with a mobile intraoperative O-arm system in the surgical department offers multiple benefits. This study aimed to assess the feasibility of postoperative CBCT by evaluating the differences in image quality and radiation dose between the two CT techniques.
Materials and methods
This single-center retrospective study included 104 pediatric syndromic and non-syndromic patients who were operated on because of single- or multiple-suture craniosynostosis at Helsinki University Hospital between January 2014 and July 2020. All patients were examined with preoperative head CT, MRI or both before the procedure. The postoperative CT scans were performed either with a conventional MSCT scanner (see next section) in a radiology department (n=58) or with a mobile intraoperative O-arm CBCT system (Medtronic, Minneapolis, MN) in a surgical department (n=46). The study was approved by the Ethics Committee of the Hospital District of Helsinki and Uusimaa (HUS/221/2017 §47) and was performed according to the principles outlined in the Declaration of Helsinki. Because of the retrospective nature of the study, no informed patient consent was required. Individual-level data cannot be shared openly due to restrictions imposed by the research permit.
Postoperative computed tomography scans performed with multi-slice computed tomograhy machines
The postoperative MSCT head examinations were performed in a head-first supine position using the following four CT systems: two 64-slice GE LightSpeed VCT (GE Healthcare, Milwaukee, WI), a 64-slice GE Discovery CT750 HD (GE Healthcare), and a 256-slice GE Revolution CT (GE Healthcare). The scan ranges of the postoperative CT examinations were typically adjusted to cover the patient anatomy from the bottom of the chin to the top of the head. Low-dose helical scan protocols developed and optimized for craniosynostosis imaging were used for all MSCT systems. All the scanners utilized a dynamic collimation mechanism for helical CT scans to prevent overranging and increased dose. The device-specific scanning parameters are presented in Table 1. For one postoperative CT examination with a GE LightSpeed VCT system, a routine axial head CT scan protocol for children was unintentionally used. This CT examination, with a mean volumetric CT dose index (CTDIvol) value of 28.67 mGy and dose-length product (DLP) of 466.6 mGy·cm, was excluded from further dose evaluations. For the GE Revolution CT, an organ-dose modulation technique (ODM, GE Healthcare, Milwaukee, WI) was used to reduce radiation exposure to the patient’s eye lens. Axial images were reconstructed using either adaptive statistical iterative reconstruction (ASiR) or ASiR-V with 20% to 40% ASiR-FBP (filtered back projection) blending. The following two sets of axial images were reconstructed: 0.625mm and 1.25mm thicknesses with soft and bone detail reconstruction filters, respectively. The image matrix was 512 × 512 and the display field of view (FOV) in the image plane was 20 × 20 cm2 or 22 × 22 cm2, resulting in voxel sizes of 0.39 × 0.39 × 0.63 mm3 or 0.43 × 0.43 × 0.63 mm3 for patients ≤18 months old and >18 months old, respectively. In addition to the axial images, 3-D surface-rendered images were created from the 0.625 mm soft reconstruction kernel images on a multi-modality image processing workstation (GE Advanced Workstation, version 4.4, Milwaukee, WI).
Postoperative cone-beam computed tomography scans performed with an O-arm device
The O-arm is a mobile intraoperative CBCT device designed for both 2-D and 3-D imaging. The equipment is specifically optimized for imaging of bony structures in spinal and orthopedic surgery, but has also been widely used for neurosurgical procedures of the brain [17, 19,20,21,22,23]. The CBCT system used in this study was a second-generation O-arm with a 40 cm × 30 cm amorphous silicon flat-panel detector and a conventional X-ray tube. For 3-D scanning of the head with a standard operating mode, a total of 196 2-D projection images were acquired during a 360° rotation with a rotation time of 13 s. The exposure time per rotation was 3.9 s due to pulsed irradiation. The 3-D scans were performed in a head-first supine position as a final step of cranial surgery. A Magnus operating table system (Maquet, Rastatt, Germany) with carbon-fiber tabletops was used for the procedures. The scan range was set using lateral and posterior-to-anterior fluoroscopic images to cover the entire skull. The FOV edge was aligned to cover the top of the head. The tube current (10 mA in all scans) and tube voltage were set manually instead of using predefined 3-D scan protocols from the vendor. The tube voltage was set to 70 kVp for patients <2-years-old, 80 kVp for patients from 2–10-years-old and 90 kVp for patients >10-years-old. The CBCT voxel size provided by the equipment was 0.42 × 0.42 × 0.83 mm3. In addition to the axial images, 3-D volume-rendered images were reconstructed either on IMPAX Volume Viewing 3-D clinical application tool (Agfa HealthCare, Mortsel, Belgium, version 6.6) or on the GE Advanced Workstation.
Dose comparisons
The volumetric CT dose index (CTDIvol) and dose-length product (DLP) values for each examination were retrospectively retrieved from the dose reports. Both the O-arm and the MSCT devices used a 16-cm reference head phantom for calculating and expressing the dose indices. The dose display accuracies of the systems were confirmed from the maintenance reports. The CTDIvol, DLP and tube voltages used in the postoperative CT scans were compared between the MSCT devices and between techniques (i.e, MSCT vs. CBCT). The radiation doses in terms of kerma-area product (KAP) of the O-arm 2-D lateral and posterior-to-anterior (fluoroscopic) planning images were also obtained from the dose reports.
Subjective image quality
Two board-certified surgeons, a plastic surgeon (surgeon 1 [J.L.] with 18 years of experience) and an oral and maxillofacial surgeon (surgeon 2 [J.S.] with 8 years of experience), examined the reconstructed images independently in a blinded manner using a pair of digital imaging and communications in medicine (DICOM)-calibrated diagnostic monitors. The combination of general image quality appearance (noise, contrast and sharpness) and appropriateness of the images for confident diagnosis of each patient examination were evaluated using a 5-point Likert scale (1, extremely poor and clinically useless image quality, defined as excessive image noise, poor contrast and image sharpness preventing delineation of critical anatomical structures; 2, poor to suboptimal but still diagnostic image quality, defined as somewhat poor contrast and sharpness and extensive but still tolerable image noise for the indication; 3, suboptimal but diagnostic image quality, defined as tolerable contrast, sharpness and noise; 4, good image quality, defined as good contrast and sharpness and very little noise for the indication; 5, excellent image quality, defined as good contrast, excellent sharpness and little to no image noise). Moreover, from the whole 3-D image stack, the presence of image artefacts, 3-D image quality and interpretation of both orbital and skull base structures were each separately evaluated using a 3-point Likert scale (1, insufficient image quality, images do not allow diagnostic interpretation; 2, limited but still tolerable image quality, moderate image artefacts; 3, good image quality, no artefacts).
Statistical analysis
Numeric results are presented as mean ± standard deviation where appropriate. Variable comparisons between the systems were performed using an independent sample Kruskal–Wallis test with a post hoc Bonferroni correction. Mann–Whitney U test was used in pairwise comparisons of MSCT (all MSCT systems combined) and CBCT (O-arm). Inter-rater reliability was evaluated using a linearly weighted Cohen’s κ correlation between the two readers. All statistical tests were two-sided, and a P-value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS statistical software (IBM, Armonk, NY, version 25.0).
Results
Baseline characteristics
A total of 104 pediatric syndromic and non-syndromic patients (mean age 1.8 ± 2.2 years, range 0.3–10.4 years) who were operated on because of single- or multiple-suture craniosynostosis were included in the study. No significant differences in patient age on day of surgery (1.6 ± 1.7 years and 2.0 ± 2.7 years; P=0.88) or sex (n=40 males (69%) and n=36 males (78%); P=0.29) were observed between the MSCT and CBCT groups.
Dose comparisons
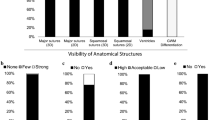
The dose display accuracies of all imaging systems were within ± 10% for the X-ray tube voltage ranges used in the patient examinations. Figure 1 and Table 2 summarize the CTDIvol and DLP values of the postoperative CT scans. The low number of patients scanned with the GE Discovery CT750 HD (n=1) and GE Revolution CT (n=2) systems prevented a reliable statistical analysis of these devices. The mean CTDIvol was up to 16% lower with the O-arm than with the GE LightSpeed VCT devices. Nevertheless, pairwise comparisons with Bonferroni correction did not reveal significant differences in the measured CTDIvol values between the five systems. However, the O-arm device resulted in significantly lower DLP values (up to 34%) compared to GE Revolution LightSpeed VCT systems (P ≤ 0.002), reflecting a shorter craniocaudal scan range used with the O-arm system. The pairwise comparisons of the postoperative 3-D imaging techniques revealed significant differences in the mean CTDIvol (1.79 ± 0.39 mGy vs. 2.09 ± 0.70 mGy; P=0.022) and DLP (28.62 ± 6.21 mGy·cm vs. 42.71 ± 18.23 mGy·cm; P < 0.001) values between the CBCT and MSCT techniques. The O-arm system used significantly lower tube voltages (70 kVp in 35/46 [76.1%] of the patients) for 3-D imaging than the MSCT systems (P < 0.001). Lower variation in dose indices were seen with the O-arm device than with the MSCT scanners utilizing tube current modulation. In O-arm 3-D scans, only the selected tube voltage affected patient exposure, as the tube current was manually set and was constant for all scans. In a single patient scanned with the O-arm, the CBCT scan with equal imaging parameters and radiation dose was performed twice due to improperly set FOV for the first scan (FOV did not reach the top of the skull). This doubled the exposure for this patient. The mean KAP from the fluoroscopy-guided FOV planning step prior to the O-arm CBCT scan was 400.5 ± 361.6 mGy·cm2.
Subjective image quality
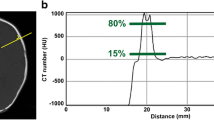
Examples of postoperative axial and surface-rendered 3-D images from a MSCT system and from the CBCT device are shown in Fig. 2 and Fig. 3, respectively. The conventional MSCT systems resulted in significantly higher subjective image quality ratings for all evaluated criteria compared with the CBCT. The ratings were 4.11 ± 0.65 and 4.91 ± 0.21 (P < 0.001) for general image quality (image noise, contrast and sharpness), 2.36 ± 0.69 and 2.72 ± 0.33 (P = 0.018) for image artefacts, 2.68 ± 0.43 and 2.95 ± 0.15 (P < 0.001) for 3-D image quality, 2.29 ± 0.75 and 2.98 ± 0.09 (P < 0.001) for the interpretation of orbital structure and 2.38 ± 0.63 and 2.96 ± 0.17 (P < 0.001) for the interpretation of skull base structures for the CBCT and MSCT, respectively. Neither surgeon rated general image quality insufficient for diagnoses for any of the scans. However, insufficient image quality was observed with the O-arm when evaluating the entire 3-D image stack for the presence of image artefacts (9/46 and 5/46 examinations [surgeon 1 and surgeon 2, respectively]), 3-D image quality (0/46 and 1/46 examinations), interpretation of orbital structures (7/46 and 11/46 examinations) and interpretation of skull base structures (4/46 and 4/46 examinations). The non-diagnostic areas in the images were not relevant for the required postoperative diagnoses.
Postoperative non-contrast-enhanced computed tomography (CT) images of a 4-month-old boy with sagittal craniosynostosis. Three-dimensional surface-rendered (a) intracranial surface-rendered (b) and axial (c) CT images clearly show the cranial sutures. Even though a low-dose CT protocol was used, the conventional multi-slice CT shows the ventricles due to sufficient soft tissue contrast of the imaging technique
Postoperative non-contrast-enhanced cone-beam computed tomography (CBCT) images of a 5-month-old boy with sagittal craniosynostosis. Three-dimensional surface-rendered (a) intracranial surface-rendered (b) and axial (c) images clearly show the cranial sutures. However, the low-dose CBCT images did not have sufficient soft tissue contrast to show the ventricles
The inter-rater reliability between the two surgeons varied from moderate to almost perfect depending on the evaluated criteria. The linearly weighted Cohen’s κ values were 0.53 (95% confidence interval [CI], 0.39 to 0.66; P < 0.001) for general image quality, 0.42 (95% CI, 0.26 to 0.58; P < 0.001) for image artefacts, 0.44 (95% CI, 0.39 to 0.66; P < 0.001) for 3-D image quality, 0.80 (95% CI, 0.68 to 0.91; P < 0.001) for the interpretation of orbital structures and 0.83 (95% CI, 0.72 to 0.95; P < 0.001) for the interpretation of skull base structures.
Discussion
Postoperative CT imaging of patients with craniosynostosis is often performed a few days after surgery in the radiology department using MSCT. This usually requires additional anesthesia and thus increases both the risks to the patient and healthcare costs. From the perspectives of patient safety and economics, it would be beneficial to perform postoperative cranial CT examinations in the operating theater, although radiation dose and image quality may differ from that of MSCT examinations. This study aimed to verify a time- and cost-effective method of performing postoperative CBCT scans for craniosynostosis by replacing MSCT examinations with O-arm CBCT scans performed in the operating theater. The radiation dose and subjective image quality were compared between the methods.
Using an intraoperative O-arm CBCT imaging system for postoperative 3-D imaging can improve patient safety, as a second induction of anesthesia for the patient is not required. Moreover, the surgeon may reposition the skull structures immediately after the intraoperative 3-D imaging. In extreme cases of severe displacement of bony structures, an immediate correction can be performed avoiding, e.g., compression and subdural hemorrhage. The results of this retrospective study show that economic savings are also possible not only due to the reduced number of anesthesia inductions required but also because no manpower or equipment resources from radiology or other departments are required for the postoperative CT.
Patient radiation exposure from the CBCT scans was comparable to that of the MSCT scanners. Pairwise analysis revealed significantly lower mean CTDIvol (1.79 ± 0.39 mGy vs. 2.09 ± 0.70 mGy; P = 0.022) and DLP (28.62 ± 6.21 mGy·cm vs. 42.71 ± 18.23 mGy·cm; P < 0.001) values for the CBCT compared to the MSCT protocol. The CBCT scan FOV was adjusted to cover the entire skull. For the MSCT scans performed in the radiology department, the scan range was usually adjusted to cover patient anatomy from the bottom of the chin to the top of the head (retrospectively it was found that there were two user instructions for postoperative MSCT scans, which were contradictory in terms of setting the scan range: one was correctly instructing the scan range to be from the upper jaw to the top of the head, while the other instructed the scan range to be from the bottom of the chin to the top of the head—the latter instruction was unfortunately followed more often). Thus, the scan range was typically longer for the MSCT examinations than for the CBCT scans, which increased the DLP. However, for purposes of postoperative imaging, covering the skull from the upper jaw to the top of the head typically provides sufficient information for the surgeon. Dose savings could therefore be achieved by limiting the MSCT scan length.
The subjective image quality of MSCT examinations was superior to that of CBCT scans. Generally, CBCT produces more image noise and lower soft tissue contrast than fan-beam CT technology used in MSCT systems [24,25,26,27]. In this study, the conventional MSCT technique especially improved the interpretation of orbital and skull base structures and reduced the number of image artefacts. Regardless, image quality was also considered sufficient for the craniosynostosis indication in all CBCT scans. Based on our image quality results, MSCT doses can be lowered even further to follow the ALARA principle (as low as reasonably achievable).
For craniosynostosis patients, a relatively high accumulated radiation dose for a child is common due to repeated CT examinations at the time of diagnosis and at various stages of surgical correction. The effective dose from a standard head CT varies from 0.5 mSv to 2 mSv. However, due to the inherent contrast of the skull, a CT examination when suspected craniosynostosis is the indication may be performed with a significantly lower exposure level. Previous studies have reported effective doses from craniosynostosis MSCT to vary widely from 0.02 mSv to 2.8 mSv [28,29,30,31,32,33]. By using the age-specific conversion factors given by Deak et al. (2010) [15] to determine effective doses from DLP values (mean k of 0.0087, 0.0054, 0.0035, and 0.0027 mSv/[mGy·cm] for newborn, 1-year-old, 5-year-old and 10-year-old children, respectively), the craniosynostosis patients in this retrospective study were exposed to effective doses ranging from 0.08 mSv to 0.27 mSv for the O-arm CBCT scans and from 0.12 mSv to 0.40 mSv for the MSCT scans. Notably, the KAP in the 2-D fluoroscopy mode to plan the CBCT scan FOV varied between patients (400.5 ± 361.6 mGy·cm2). By using conversion factors from KAP to effective dose (0.034 mSv/[Gy·cm2], 0.37 mSv/[Gy·cm2] and 0.058 mSv/[Gy·cm2] for posterior-to-anterior, lateral and anterior-to-posterior head radiographs, respectively) from Wall et al. (2011) [34], fluoroscopy resulted in an effective dose of 0.01 mSv to 0.04 mSv. Note that the conversion factors depend not only on patient age but also, for example, on the X-ray tube voltage and filtration. Thus, the effective doses reported above are only approximations and should be adopted with caution.
This study has some limitations. First, the total number of patients was small. Specifically, the small number of patients imaged with two of the four MSCT systems prevented device-specific analysis. However, the reported dose indices and scan parameters were comparable between the CT devices, and therefore, it is assumed that no remarkable differences occurred. Second, the study results are not based on a comparison of a postoperative MSCT and CBCT in the same patient. This would, however, not have been ethically justifiable. Third, the MSCT systems being studied were limited to only one manufacturer and a few models. As CT optimization methods and scan geometries differ between vendors (and between CT models from the same vendor), the conclusions from the scan protocols used here cannot be directly generalized to other MSCT systems. Moreover, older versions of GE CT scanners might also have influenced the MSCT doses negatively as detectors, iterative reconstructions etc. have improved and reduced doses. For example, deep-learning image reconstructions, such as GE’s TrueFidelity, may reduce patient doses even further, while maintaining sufficient image quality for diagnosis [35]. Fourth, only two surgeons evaluated the subjective image quality and radiologist raters were not used. This decision was made as, in our hospital, surgeons report the postoperative O-arm CBCT scans performed in our surgical unit. Pediatric radiologists are no longer involved in the immediate postoperative 3-D imaging of patients with craniosynostosis unless a CT scan needs to be performed in the radiology department due to O-arm equipment failure or lack of qualified O-arm users working on the shift in the surgery department (pediatric radiologists report the preoperative MSCT scans performed in the radiology department). Finally, image quality was only analyzed subjectively. Objective image quality analysis with, for example, more comprehensive image noise, contrast-to-noise, spatial resolution and noise power spectra analysis is likely to have revealed more differences between the methods. For example, it is commonly known that CBCT systems, which are designed specifically for imaging of bony structures, generate more image noise than MSCT systems. However, this study was mainly designed to determine the feasibility and clinical applications of the O-arm device for postoperative craniosynostosis CT imaging. In the future, phantom measurements with more comprehensive image quality analysis may be performed to further optimize the scan protocols.
Conclusion
The patient radiation doses of the craniosynostosis imaging protocols studied were comparable between the CBCT and MSCT systems, with slightly lower doses reported for the former. Based on a subjective evaluation considering image noise, contrast, sharpness, presence of artefacts, 3-D image quality and interpretability of orbital and skull base structures, the CBCT technique showed a lower but diagnostic image quality compared to MSCT for postoperative CT imaging of patients with craniosynostosis. Thus, CBCT imaging using an O-arm device is a feasible option and may replace conventionally performed MSCT examinations for this indication. The most important benefits of intraoperative CBCT include less anesthesia, lower health costs and the possibility of evaluating the immediate postoperative results.
Data availability
Individual-level data cannot be shared openly due to restrictions imposed by the research permit.
References
Twigg SR, Wilkie AO (2015) A genetic-pathophysiological framework for craniosynostosis. Am J Hum Genet 97:359–377
Kajdic N, Spazzapan P, Velnar T (2018) Craniosynostosis – recognition, clinical characteristics, and treatment. Bosn J Basic Med Sci 18:110–116
French LR, Jackson IT, Melton LJ 3rd (1990) A population-based study of craniosynostosis. J Clin Epidemiol 43:69–73
Boulet SL, Rasmussen SA, Honein MA (2008) A population-based study of craniosynostosis in metropolitan Atlanta, 1989–2003. Am J Med Genet A 146A:984–991
Cornelissen M, den Ottelander B, Rizopoulos D et al (2016) Increase of prevalence of craniosynostosis. J Craniomaxillofac Surg 44:1273–1279
Boyle CM, Rosenblum JD (1997) Three-dimensional CT for pre- and postsurgical imaging of patients with craniosynostosis: correlation of operative procedure and radiological imaging. AJR Am J Roentgenol 169:1173–1177
Panchal J, Uttchin V (2003) Management of craniosynostosis. Plast Reconstr Surg 111:2032–2048
Binaghi S, Gudinchet F, Rilliet B (2000) Three-dimensional spiral CT of craniofacial malformations in children. Pediatr Radiol 30:856–860
Furuya Y, Edwards MSB, Alpers CE et al (1984) Computerized tomography of cranial sutures. Part 1: Comparison of suture anatomy in children and adults. J Neurosurg 61:53–58
Massimi L, Bianchi F, Calandrelli R et al (2019) Imaging in craniosynostosis: when and what? Childs Nerv Syst 35:2055–2069
Makar KG, Garavaglia HE, Muraszko KM et al (2021) Computed tomography in patients with craniosynostosis: a survey to ascertain practice patterns among craniofacial surgeons. Ann Plast Surg 87:569–574
Brenner DJ, Hall EJ (2007) Computed tomography–an increasing source of radiation exposure. N Engl J Med 357:2277–2284
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505
Huda W, Vance A (2007) Patient radiation doses from adult and pediatric CT. AJR Am J Roentgenol 188:540–546
Deak PD, Smal Y, Kalender WA (2010) Multisection CT protocols: sex and age-specific conversion factors used to determine effective dose from dose-length product. Radiology 257:158–166
Hauptmann M, Byrnes G, Cardis E et al (2022) Brain cancer after radiation exposure from CT examinations of children and young adults: results from the EPI-CT cohort study. Lancet Oncol 24:45–53
Katisko JPA, Kauppinen MT, Koivukangas JP, Heikkinen ER (2012) Stereotactic operations using the O-arm. Stereotact Funct Neurosurg 90:401–409
Schnetzke M, Fuchs J, Vetter SY et al (2016) Intraoperative 3D imaging in the treatment of elbow fractures–a retrospective analysis of indications, intraoperative revision rates, and implications in 36 cases. BMC Med Imaging 16:24
Feng W, Wang W, Chen S et al (2020) O-arm navigation versus C-arm guidance for pedicle screw placement in spine surgery: a systematic review and meta-analysis. Int Orthop 44:919–926
Verhofste BP, Glotzbecker MP, Hresko MT et al (2020) Intraoperative use of O-arm in pediatric cervical spine surgery. J Pediatr Orthop 40:e266–e271
Katati MJ, Jover VA, Iañez VB et al (2020) An initial experience with intraoperative O-arm for deep brain stimulation surgery: can it replace post-operative MRI? Acta Neurol Belg 120:295–301
Banat M, Wach J, Salemdawod A et al (2021) The role of intraoperative image guidance systems (three-dimensional c-arm versus O-arm) in spinal surgery: results of a single-center study. World Neurosurg 146:e817–e821
Furlanetti L, Hasegawa H, Oviedova A et al (2021) O-arm stereotactic imaging in deep brain stimulation surgery workflow: a utility and cost-effectiveness analysis. Stereotact Funct Neurosurg 99:93–106
Yu L, Vrieze TJ, Bruesewitz MR et al (2010) Dose and image quality evaluation of a dedicated cone-beam CT system for high-contrast neurologic applications. AJR Am J Roentgenol 194:W193–W201
Schegerer AA, Lechel U, Ritter M et al (2014) Dose and image quality of cone-beam computed tomography as compared with conventional multislice computed tomography in abdominal imaging. Invest Radiol 49:675–684
Lechuga L, Weidlich GA (2016) Cone beam CT vs. fan beam CT: a comparison of image quality and dose delivered between two differing CT imaging modalities. Cureus 8:e778
Posadzy M, Desimpel J, Vanhoenacker F (2018) Cone beam CT of the musculoskeletal system: clinical applications. Insights Imaging 9:35–45
Cerovac S, Neil-Dwyer JG, Rich P et al (2002) Are routine preoperative CT scans necessary in the management of single suture craniosynostosis? Br J of Neurosurg 16:348–354
Jaffurs D, Denny A (2009) Diagnostic pediatric computed tomographic scans of the head: actual dosage versus estimated risk. Plast Reconstr Surg 124:1254–1260
Didier RA, Kuang AA, Schwartz DL et al (2010) Decreasing the effective radiation dose in pediatric craniofacial CT by changing head position. Pediatr Radiol 40:1910–1917
Calandrelli R, D’Apolito G, Gaudino S et al (2014) Identification of skull base sutures and craniofacial anomalies in children with craniosynostosis: utility of multidetector CT. Radiol Med 119:694–704
Kaasalainen T, Palmu K, Lampinen A et al (2015) Limiting CT radiation dose in children with craniosynostosis: phantom study using model-based iterative reconstruction. Pediatr Radiol 45:1544–1553
Barreto IL, Tuna IS, Rajderkar DA et al (2022) Pediatric craniosynostosis computed tomography: an institutional experience in reducing radiation dose while maintaining diagnostic image quality. Pediatr Radiol 52:85–96
Wall BF, Haylock RG, Jansen JT, et al (2011) Radiation risks from medical X-ray examinations as a function of the age and sex of the patient. Report HPACRCE-028. Health Protection Agency, Chilton. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/340147/HPA-CRCE-028_for_website.pdf. Accessed 12 January 2023
Franck C, Zhang G, Deak P, Zanca F (2021) Preserving image texture while reducing radiation dose with a deep learning image reconstruction algorithm in chest CT: a phantom study. Phys Med 81:86–93
Funding
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital.
Author information
Authors and Affiliations
Contributions
All authors participated in planning the study and drafting the manuscript. T.K. gathered and analyzed the dose data, performed statistical analysis and drafted the initial manuscript. V.M. and A.N. collected the patient and procedural data. T.M. participated in drafting the initial manuscript and produced the figures. J.S. performed the subjective image quality evaluations. A.H. supervised and supported the study. J.L. performed the surgical procedures, initiated the study concept and performed subjective image quality evaluations. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Hospital District of Helsinki and Uusimaa (HUS/221/2017 §47).
Consent to participate
Due to the retrospective nature of the study, no informed patient consent was required for this study. The authors affirm that human research participants provided informed consent for publication of the images in both Figs. 2 and 3.
Conflicts of interest
None
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kaasalainen, T., Männistö, V., Mäkelä, T. et al. Postoperative computed tomography imaging of pediatric patients with craniosynostosis: radiation dose and image quality comparison between multi-slice computed tomography and O-arm cone-beam computed tomography. Pediatr Radiol 53, 1704–1712 (2023). https://doi.org/10.1007/s00247-023-05644-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-023-05644-3