Abstract
Background
Hepatocellular carcinoma (HCC) is rare in children and there is limited data on its imaging features.
Objective
To describe imaging features of pediatric HCC and correlate them with clinical and laboratory findings.
Materials and methods
We retrospectively reviewed imaging in all pediatric HCC cases seen between January 2000 and January 2019. Imaging features defined in LI-RADS (Liver Imaging Reporting and Data System) and tumor extent by PRETEXT (pretreatment extent of disease) criteria were noted by two radiologists. Patient charts were reviewed to collect clinical features, alpha-fetoprotein (AFP) level and pathology findings.
Results
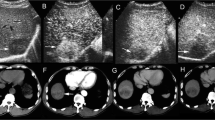
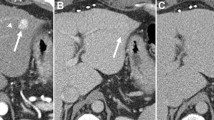
Of the 15 children (7 boys, 8 girls; mean age: 11.8 years, age range: 6–17 years) included in the study, 12/15 had computed tomography, 9/15 had magnetic resonance imaging and 9/15 had ultrasound exams available for review. Pathological types of HCC included classic (11/15, 73%), fibrolamellar (3/15, 20%) and mixed cholangiocarcinoma-HCC (1/15, 7%). Eighty percent occurred de novo in normal liver and 67% showed elevated AFP levels. Arterial phase hyperenhancement was seen in 83% of cases, washout in 86%, capsule in 50% and tumor-in-vein in 33%. The mean tumor size was 9.8 cm and 40% were multifocal on imaging. Staging revealed PRETEXT II tumors in 47%, III in 20% and IV in 33%. There were no PRETEXT I tumors. The two most common PRETEXT annotation factors were portal vein and caudate lobe involvement in 71% and 43% of cases, respectively. Fibrolamellar HCC demonstrated central scar, normal AFP levels and normal background liver.
Conclusion
Pediatric HCC are large heterogeneous tumors, as reflected by high PRETEXT staging, and commonly include portal vein and caudate involvement. This affects resectability of these tumors at presentation. Central scar, normal AFP level and normal liver background may help differentiate fibrolamellar HCC from other types of HCC.




Similar content being viewed by others
References
Meyers RL (2007) Tumors of the liver in children. Surg Oncol 16:195–203
López-Terrada D, Alaggio R, de Dávila MT et al (2014) Towards an international pediatric liver tumor consensus classification: proceedings of the los Angeles COG liver tumors symposium. Mod Pathol 27:472–491
Gupta AA, Gerstle JT, Ng V et al (2011) Critical review of controversial issues in the management of advanced pediatric liver tumors. Pediatr Blood Cancer 56:1013–1018
Chung EM, Lattin GE Jr, Cube R et al (2011) From the archives of the AFIP: pediatric liver masses: radiologic-pathologic correlation. Part 2. Malignant tumors. Radiographics 31:483–507
Chavhan GB, Siddiqui I, Ingley KM, Gupta AA (2019) Rare malignant liver tumors in children. Pediatr Radiol 49:1404–1421
Czauderna P (2002) Adult type vs. childhood hepatocellular carcinoma — are they the same or different lesions? Biology, natural history, prognosis, and treatment. Med Pediatr Oncol 39:519–523
Khanna R, Verma SK (2018) Pediatric hepatocellular carcinoma. World J Gastroenterol 24:3980–3999
Sindhi R, Rohan V, Bukowinski A et al (2020) Liver transplantation for pediatric liver cancer. Cancers (Basel) 12:720
Czauderna P, Zbrzezniak G, Narozanski W et al (2006) Preliminary experience with arterial chemoembolization for hepatoblastoma and hepatocellular carcinoma in children. Pediatr Blood Cancer 46:825–828
Lau CS, Mahendraraj K, Chamberlain RS (2015) Hepatocellular carcinoma in the pediatric population: a population based clinical outcomes study involving 257 patients from the surveillance, epidemiology, and end result (SEER) database (1973-2011). HPB Surg 2015:670728
Chavhan GB, Shelmerdine S, Jhaveri K, Babyn PS (2016) Liver MR imaging in children: current concepts and technique. Radiographics 36:1517–1532
LI-RADS Steering Committee (2018) CT/MRI LI-RADS v2018 Core. https://www.acr.org/-/media/ACR/Files/RADS/LI-RADS/LI-RADS-2018-Core.pdf. Accessed 15 April 2020
Towbin AJ, Meyers RL, Woodley H et al (2018) 2017 PRETEXT: radiologic staging system for primary hepatic malignancies of childhood revised for the Paediatric Hepatic International Tumour Trial (PHITT). Pediatr Radiol 48:536–554
Allan BJ, Wang B, Davis JS et al (2014) A review of 218 pediatric cases of hepatocellular carcinoma. J Pediatr Surg 49:166–171
D'Souza AM, Shah R, Gupta A et al (2018) Surgical management of children and adolescents with upfront completely resected hepatocellular carcinoma. Pediatr Blood Cancer 65:e27293
Ludwig DR, Romberg EK, Fraum TJ et al (2019) Diagnostic performance of liver imaging reporting and data system (LI-RADS) v2017 in predicting malignant liver lesions in pediatric patients: a preliminary study. Pediatr Radiol 49:746–758
Almotairi M, Oudjhane K, Chavhan GB (2015) Pediatric multifocal liver lesions evaluated by MRI. Indian J Radiol Imaging 25:296–302
Shaohua L, Qiaoxuan W, Peng S et al (2015) Surgical strategy for hepatocellular carcinoma patients with portal/hepatic vein tumor thrombosis. PLoS One 10:e0130021
Rummeny E, Weissleder R, Sironi S et al (1989) Central scars in primary liver tumors: MR features, specificity, and pathologic correlation. Radiology 171:323–326
Meyers RL, Maibach R, Hiyama E et al (2017) Risk-stratified staging in paediatric hepatoblastoma: a unified analysis from the Children's Hepatic Tumors International Collaboration. Lancet Oncol 18:122–131
Zhou S, Venkatramani R, Gupta S et al (2017) Hepatocellular malignant neoplasm, NOS: a clinicopathological study of 11 cases from a single institution. Histopathology 71:813–822
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Arias, G.A., Siddiqui, I., Navarro, O.M. et al. Imaging and clinical features of pediatric hepatocellular carcinoma. Pediatr Radiol 51, 1339–1347 (2021). https://doi.org/10.1007/s00247-021-04989-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-021-04989-x