Abstract
Background
A resident working under the entrustable professional activity of a graduated independent coverage model must identify nonaccidental trauma and notify clinicians of this concern to facilitate potential removal of the child from harm. The resident’s role in identifying child abuse has not previously been studied.
Objective
The purpose of this study was to assess radiology residents’ ability to identify radiographic imaging findings of nonaccidental trauma in a simulated call environment.
Materials and methods
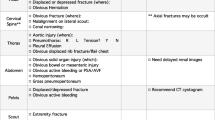
The Wisdom in Diagnostic Imaging Emergent/Critical Care Radiology Simulation (WIDI SIM) is a strategically designed computer-aided simulation of an emergency imaging experience that has been rigorously tested and proven to be a reliable means for assessing resident preparedness to competently and independently cover radiology call. The residents are provided with 65 cases of varying difficulty, including normal studies. Those cases include ones that require the resident to accurately identify skeletal findings of nonaccidental trauma. The residents respond using free text that is then scored manually by faculty members utilizing a robust grading rubric. Missed cases are then categorized by observation error and/or interpretative errors.
Results
A total of 675 radiology residents were given a case of nonaccidental trauma using the WIDI simulation web-based test platform between 2014 and 2017. Child abuse was consistently underdiagnosed by radiology residents being tested for call readiness irrespective of the numbers of years in training. Correct diagnostic score averages per year ranged from 10% to 79%. In year 1, 71% of residents correctly diagnosed nonaccidental trauma with a total of 101 participants. In year 2, 130 residents participated with only 20% answering correctly. In year 3, there were 201 participants with 79% correctly diagnosing nonaccidental trauma. In year 4, only 10% of 243 residents accurately diagnosed nonaccidental trauma. Residents from various stages of training were tested. Cases used with leading histories provided, accounted for a higher correct call rate.
Conclusion
Radiology residency programs may be deficient in teaching residents to accurately recognize and report child abuse. This deficiency has potential implications for programs where a radiology attending is not present after hours as it raises the concern that child abuse may be missed by residents taking independent call. These data further question whether graduating radiologists are competent to recognize nonaccidental trauma and demonstrates the need for additional mandatory training during radiology residency.








Similar content being viewed by others
References
U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children et al (2020) Child maltreatment 2018. https://www.acf.hhs.gov/ch/research-data-technology/statistics-research/child-maltreatment. Accessed 12 April 2020
U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children et al (2019) Mandatory reporters of child abuse and neglect. https://www.childwelfare.gov/pubPDFs/manda.pdf. Accessed 12 April 2020
Woolf A, Taylor L, Melnicoe L et al (1988) What residents know about child abuse: implications of knowledge and attitudes. Am J Dis Child 42:668–672
Dubowitz H (1988) Child abuse programs and pediatric residency training. Pediatrics 82:477–480
Socolar RR (1996) Physician knowledge of child sexual abuse. Child Abuse Negl 20:783–790
Ward MGK, Bennett S, Plint AC et al (2004) Child protection: a neglected area of pediatric residency training. Child Abuse Negl 28:1113–1122
Accreditation Council for Graduate Medical Education (2020) Diagnostic radiology case log requirements. https://www.acgme.org/Portals/0/PFAssets/ProgramResources/DR_Case_Log_Categories.pdf. Accessed 15 September 2020
Accreditation Council for Graduate Medical Education (2019) Common program requirements. https://www.acgme.org/Portals/0/PFAssets/ProgramRequirements/CPRResidency2019.pdf. Accessed 13 April 2020
Sistrom CL, Slater RM, Rajderkar DA et al (2020) Full resolution simulation for evaluation of critical care imaging interpretation; part 1: fixed effects identify influences of exam, specialty, fatigue and training on resident performance. Acad Radiol 27:1006–1015
Sistrom CL, Slater RM, Rajderkar DA et al (2020) Full resolution simulation for evaluation of critical care imaging interpretation; part 2: random effects reveal the interplay between case difficulty, resident competence, and the training environment. Acad Radiol 27:1016–1024
American College of Radiology (2016) ACR-SPR practice parameter for the performance and interpretation of skeletal surveys in children. http://acr.org/-/media/ACR/Files/Practice-Parameters/Skeletal-Survey.pdf. Accessed 13 April 2020
Kleinman PK, Marks SC Jr, Richmond JM, Blackbourne BD (1995) Inflicted skeletal injury: a postmortem radiologic-histopathologic study in 31 infants. AJR Am J Roentgenol 163:647–650
King J, Diefendorf D, Apthorp J et al (1998) Analysis of 429 fractures in 189 battered children. J Pediatr Orthop 8:585–589
Flaherty EG, Perez-Rossello JM, Levine MA et al (2014) Evaluating children with fractures for child physical abuse. Pediatrics 133:477–489
Kleinman P (2015) Diagnostic imaging of child abuse. Cambridge University Press, New York
Kemp AM, Dunstan F, Harrison S et al (2008) Patterns of skeletal fractures in child abuse: systematic review. BMJ 337:a1518
Wood JN, Fakeye O, Mondestin V et al (2015) Development of hospital-based guidelines for skeletal survey in young children with bruises. Pediatrics 135:312–320
Kamarzyn B, Wanner MR, Marine MB et al (2019) The added value of a second read by pediatric radiologists for outside skeletal surveys. Pediatr Radiol 49:203–209
Cooper VF, Goodhartz LA, Nemcek AA Jr, Ryu RK (2008) Radiology resident interpretations of on-call imaging studies: the incidence of major discrepancies. Acad Radiol 15:1198–1204
Narayan AP, Socolar RRS, St Claire K (2006) Pediatric residency training in child abuse and neglect in the United States. Pediatrics 117:2215–2221
Christian CW (2008) Professional education in child abuse and neglect. Pediatrics 122:S13–S17
Acknowledgments
Thank you to Dr. Christopher Sistrom for his assistance and review of the statistical analysis in this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Sharma, P.G., Rajderkar, D.A., Slater, R.M. et al. Rate of resident recognition of nonaccidental trauma: how well do residents perform?. Pediatr Radiol 51, 773–781 (2021). https://doi.org/10.1007/s00247-020-04908-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-020-04908-6