Abstract
Background
Lung ultrasound (US) in the evaluation of suspected pediatric pneumonia is increasingly used and has a recognized role in evaluating pleural effusions, although there are no detailed studies specifically addressing its use in the pediatric population.
Objectives
To define lung US findings of severe pediatric community-acquired pneumonia that required surgical procedures during admission.
Materials and methods
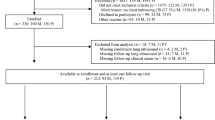
Our prospective case-control study compared lung US findings in patients ages 1 month to 17 years admitted with community-acquired pneumonia that required surgical procedures from findings those who did not. Lung US was performed at admission and always before surgical procedures. Medical treatment, laboratory and microbiological findings, chest X-ray, computed tomography scan and surgical procedures are described.
Results
One hundred twenty-one children with community-acquired pneumonia were included; of these, 23 underwent surgical intervention. Compared with the control group, children requiring a surgical procedure had a significantly higher rate of large consolidations (52.2%; 95% confidence interval [CI]: 30.6% to 73.2%), larger and complicated pleural effusions (100%; 95% CI: 85.2% to 100%), and both liquid and air bronchograms (73.9%; 95% CI: 51.6% to 89.8%).
Conclusion
Larger consolidations, larger and more complicated pleural effusions, and liquid and air bronchograms were associated with surgical treatment.



Similar content being viewed by others
References
World Health Organization (2019) Pneumonia. http://www.who.int/mediacentre/factsheets/fs331/en/index.html. Accessed 17 October 2019
Rudan I, O'Brien KL, Nair H et al (2013) Epidemiology and etiology of childhood pneumonia in 2010: estimates of incidence, severe morbidity, mortality, underlying risk factors and causative pathogens for 192 countries. J Glob Health 3:010401
McAllister DA, Liu L, Shi T et al (2019) Global, regional, and national estimates of pneumonia morbidity and mortality in children younger than 5 years between 2000 and 2015: a systematic analysis. Lancet Glob Health 7:e47–e57
Bradley JS, Byington CL, Shah SS et al (2011) The management of community-acquired pneumonia in infants and children older than 3 months of age: clinical practice guidelines by the Pediatric Infectious Diseases Society and the Infectious Diseases Society of America. Clin Infect Dis 53:e25–e76
United Nations, Department of Economic and Social Affairs, Population Division (2015) World population prospects: the 2015 revision, key findings and advance tables. https://esa.un.org/unpd/wpp/publications/files/key_findings_wpp_2015.pdf. Accessed 12 August 2019
Nair H, Simoes EA, Rudan I et al (2013) Global and regional burden of hospital admissions for severe acute lower respiratory infections in young children in 2010: a systematic analysis. Lancet 381:1380–1390
Sawicki GS, Lu FL, Valim C et al (2008) Necrotising pneumonia is an increasingly detected complication of pneumonia in children. Eur Respir J 31:1285–1291
Gerdung CA, Ross BC, Dicken BJ, Bjornson CL (2019) Pneumonectomy in a child with multilobar pneumatocele secondary to necrotizing pneumonia: case report and review of the literature. Case Rep Pediatr 2019:2464390
De Marco R, Accordini S, Marcon A et al (2011) Risk factors for chronic obstructive pulmonary disease in a European cohort of young adults. Am J Respir Crit Care Med 183:891–897
Svanes C, Sunyer J, Plana E et al (2010) Early life origins of chronic obstructive pulmonary disease. Thorax 65:14–20
Edmond K, Scott S, Korczak V et al (2012) Long term sequelae from childhood pneumonia; systematic review and meta-analysis. PLoS One 7:e31239
Le Roux DM, Zar HJ (2017) Community-acquired pneumonia in children - a changing spectrum of disease. Pediatr Radiol 47:1392–1398
Musolino AM, Tomà P, Supino MC et al (2019) Lung ultrasound features of children with complicated and noncomplicated community acquired pneumonia: a prospective study. Pediatr Pulmonol 54:1479–1486
Buonsenso D, Curatola A, Valentini P et al (2019) Chest ultrasound findings in children with confirmed pulmonary tuberculosis in low tuberculosis incidence country. Pediatr Pulmonol 54:1348–1350
Buonsenso D, Musolino AM, Gatto A et al (2019) Lung ultrasound in infants with bronchiolitis. BMC Pulm Med 19:159
Supino MC, Buonsenso D, Musolino AM (2019) Correspondence on "ultrasound as diagnosis tool for grading bronchiolitis. Where are your limits lost?". Eur J Pediatr 178:1447
Supino MC, Buonsenso D, Scateni S et al (2019) Point-of-care lung ultrasound in infants with bronchiolitis in the pediatric emergency department: a prospective study. Eur J Pediatr 178:623–632
Buonsenso D, Musolino A (2018) Point of care diaphragm ultrasound in infants with bronchiolitis. Pediatr Pulmonol 53:1597
Buonsenso D, Supino MC, Giglioni E et al (2018) Point of care diaphragm ultrasound in infants with bronchiolitis: a prospective study. Pediatr Pulmonol 53:778–786
Berce V, Tomazin M, Gorenjak M et al (2019) The usefulness of lung ultrasound for the aetiological diagnosis of community-acquired pneumonia in children. Sci Rep 9:17957
Lissaman C, Kanjanauptom P, Ong C et al (2019) Prospective observational study of point-of-care ultrasound for diagnosing pneumonia. Arch Dis Child 104:12–18
Maffey A, Colom A, Venialgo C et al (2019) Clinical, functional, and radiological outcome in children with pleural empyema. Pediatr Pulmonol 54:525–530
Pacilli M, Nataraja RM (2019) Management of paediatric empyema by video-assisted thoracoscopic surgery (VATS) versus chest drain with fibrinolysis: systematic review and meta-analysis. Paediatr Respir Rev 30:42–48
Marhuenda C, Barceló C, Fuentes I et al (2014) Urokinase versus VATS for treatment of empyema: a randomized multicenter clinical trial. Pediatrics 134:e1301–e1307
Cobanoglu U, Sayir F, Bilici S, Melek M (2011) Comparison of the methods of fibrinolysis by tube thoracostomy and thoracoscopic decortication in children with stage II and III empyema: a prospective randomized study. Pediatr Rep 3:e29
Kurt BA, Winterhalter KM, Connors RH et al (2006) Therapy of parapneumonic effusions in children: video-assisted thoracoscopic surgery versus conventional thoracostomy drainage. Pediatrics 118:e547–e553
Sonnappa S, Cohen G, Owens CM et al (2006) Comparison of urokinase and video-assisted thoracoscopic surgery for treatment of childhood empyema. Am J Respir Crit Care Med 174:221–227
Chiu CY, Wong KS, Huang YC et al (2006) Echo-guided management of complicated parapneumonic effusion in children. Pediatr Pulmonol 41:1226–1232
James CA, Braswell LE, Pezeshkmehr AH et al (2017) Stratifying fibrinolytic dosing in pediatric parapneumonic effusion based on ultrasound grade correlation. Pediatr Radiol 47:89–95
Kushner LE, Nieves DJ, Osborne S et al (2019) Oral antibiotics for treating children with community-acquired pneumonia complicated by empyema. Clin Pediatr (Phila) 58:1401–1408
De Benedictis FM, Carloni I (2019) Management of necrotizing pneumonia in children: time for a patient-oriented approach. Pediatr Pulmonol 54:1351–1353
Acknowledgements
We are grateful to Dr. Caterina Bock from Bambino Gesù Children Hospital for her support in reviewing images. We are thankful to the members of the Italian Academy of Thoracic Ultrasound (Accademia Di Ecografia Toracica, ADET) for training and inspiring Italian and international researchers in the field of lung ultrasound.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Buonsenso, D., Tomà, P., Scateni, S. et al. Lung ultrasound findings in pediatric community-acquired pneumonia requiring surgical procedures: a two-center prospective study. Pediatr Radiol 50, 1560–1569 (2020). https://doi.org/10.1007/s00247-020-04750-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-020-04750-w