Abstract
Background
Neurocutaneous melanosis is a rare disorder in which children with large cutaneous melanotic nevi have associated melanosis in the brain. Although many affected children have structurally normal brains, some have associated developmental disorders or brain anomalies.
Objectives
To determine the range of extent of brain melanosis as assessed by magnetic resonance imaging (MRI) and to investigate the frequency and types of associated brain anomalies.
Materials and methods
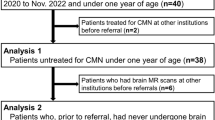
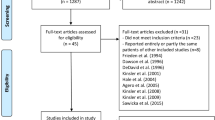
We retrospectively reviewed brain and spine MRIs of 80 patients with congenital melanocytic nevi (range: 1 day to 22 years of age) affiliated with Nevus Outreach Inc. from 1998 to 2017. Central nervous system (CNS) melanosis was diagnosed when a mass with abnormal parenchymal T1 hyperintensity was seen. The locations of abnormal signal, associated malformations, the presence of contrast enhancement and, in patients with more than one MRI, changes over time were recorded. Associations among findings were analyzed using chi-square test or Fisher exact test.
Results
Brain abnormalities were identified in 33 patients. The most common finding was melanosis in the amygdala, which was found in 31 patients (an isolated finding in 14 patients). Nineteen patients had melanosis in the brainstem, cerebellum, cerebral cortex or thalamus. Cerebral and/or spinal leptomeningeal enhancement was uncommon (five patients). Hindbrain melanosis was associated with cerebellar and pontine hypoplasia (P=0.012). Brain melanosis was most easily seen on T1 images prior to myelination; reduced/loss of visibility was noted as the CNS matured.
Conclusion
Brain melanosis is a common manifestation in children with large cutaneous melanotic nevi, most commonly found in the anterior temporal lobes (amygdala), brainstem, cerebellum and cerebral cortex. Hindbrain melanosis is associated with hypoplasia of the affected structures. Early imaging is optimal to provide the greatest sensitivity for diagnosis and to guide proper management.






Similar content being viewed by others
References
Kadonaga JN, Frieden IJ (1991) Neurocutaneous melanosis: definition and review of the literature. J Am Acad Dermatol 24(5 Pt 1):747–755
Rokitansky J (1861) Ein ausgezeichneter fall von pigment-mal mit ausgebreiteter pigmentierung der inneren hirn- und ruchenmarkshaute. [An excellent instance of pigmentation of the inner cerebral layers and skin]. Allg Wien Med Z 6:113–116
Maclachlan WW (1914) Extensive pigmentation of the brain associated with nevi pigmentosi of the skin. J Med Res 29:433–446.1
DeDavid M, Orlow SJ, Provost N et al (1996) Neurocutaneous melanosis: clinical features of large congenital melanocytic nevi in patients with manifest central nervous system melanosis. J Am Acad Dermatol 35:529–538
Hale EK, Stein J, Ben-Porat L et al (2005) Association of melanoma and neurocutaneous melanocytosis with large congenital melanocytic naevi--results from the NYU-LCMN registry. Br J Dermatol 152:512–517
Lovett A, Maari C, Decarie JC et al (2009) Large congenital melanocytic nevi and neurocutaneous melanocytosis: one pediatric center's experience. J Am Acad Dermatol 61:766–774
Kinsler VA, Thomas AC, Ishida M et al (2013) Multiple congenital melanocytic nevi and neurocutaneous melanosis are caused by postzygotic mutations in codon 61 of NRAS. J Invest Dermatol 133:2229–2236
Reyes-Mugica M, Chou P, Byrd S et al (1993) Nevomelanocytic proliferations in the central nervous system of children. Cancer 72:2277–2285
Frieden IJ, Williams ML, Barkovich AJ (1994) Giant congenital melanocytic nevi: brain magnetic resonance findings in neurologically asymptomatic children. J Am Acad Dermatol 31(3 Pt 1):423–429
Foster RD, Williams ML, Barkovich AJ et al (2001) Giant congenital melanocytic nevi: the significance of neurocutaneous melanosis in neurologically asymptomatic children. Plast Reconstr Surg 107:933–941
Kinsler VA, Birley J, Atherton DJ (2008) Great Ormond Street Hospital for Children Registry for Congenital Melanocytic Naevi: prospective study 1988–2007. Part 1—epidemiology, phenotype and outcomes. Br J Dermatol 160:143–150
Kadonaga JN, Barkovich AJ, Edwards MS, Frieden IJ (1992) Neurocutaneous melanosis in association with the Dandy-Walker complex. Pediatr Dermatol 9:37–43
Watt AJ, Kotsis SV, Chung KC (2004) Risk of melanoma arising in large congenital melanocytic nevi: a systematic review. Plast Reconstr Surg 113:1968–1974
Waelchli R, Aylett SE, Atherton D et al (2015) Classification of neurological abnormalities in children with congenital melanocytic naevus syndrome identifies magnetic resonance imaging as the best predictor of clinical outcome. Br J Dermatol 173:739–750
Shah KN (2010) The risk of melanoma and neurocutaneous melanosis associated with congenital melanocytic nevi. Semin Cutan Med Surg 29:159–164
Gaviani P, Mullins ME, Braga TA et al (2006) Improved detection of metastatic melanoma by T2*-weighted imaging. AJNR Am J Neuroradiol 27:605–608
Gramsch C, Goricke SL, Behrens F et al (2013) Isolated cerebral susceptibility artefacts in patients with malignant melanoma: metastasis or not? Eur Radiol 23:2622–2627
Bolande RP (1997) Neurocristopathy: its growth and development in 20 years. Pediatr Pathol Lab Med 17:1–25
Basch ML, Selleck MA, Bronner-Fraser M (2000) Timing and competence of neural crest formation. Dev Neurosci 22:217–227
Cramer SF (1988) The melanocytic differentiation pathway in congenital melanocytic nevi: theoretical considerations. Pediatr Pathol 8:253–265
Takayama H, Nagashima Y, Hara M et al (2001) Immunohistochemical detection of the c-met proto-oncogene product in the congenital melanocytic nevus of an infant with neurocutaneous melanosis. J Am Acad Dermatol 44:538–540
Kos L, Aronzon A, Takayama H et al (1999) Hepatocyte growth factor/scatter factor-MET signaling in neural crest-derived melanocyte development. Pigment Cell Res 12:13–21
Fox H (1972) The phakomatoses, vol 4. Neurocutaneous melanosis. Elsevier, New York
Enochs WS, Petherick P, Bogdanova A et al (1997) Paramagnetic metal scavenging by melanin: MR imaging. Radiology 204:417–423
Ramaswamy V, Delaney H, Haque S et al (2012) Spectrum of central nervous system abnormalities in neurocutaneous melanocytosis. Dev Med Child Neurol 54:563–568
Bekiesinska-Figatowska M, Sawicka E, Zak K, Szczygielski O (2016) Age related changes in brain MR appearance in the course of neurocutaneous melanosis. Eur J Radiol 85:1427–1431
Barkovich AJ, Frieden IJ, Williams ML (1994) MR of neurocutaneous melanosis. AJNR Am J Neuroradiol 15:859–867
Fox H (1972) Neurocutaneous melanosis. In: Vinken PJ, Bruyn GW (edd) Handbook of clinical neurology. North-Holland, Amsterdam, pp 414–428
Marin-Padilla M (1988) Embryonic vascularization of the mammalian cerebral cortex. In: Peters A, Jones EG (eds) Cerebral cortex: Development and maturation of the cerebral cortex, vol 4. Plenum, New York, pp 79–509
Fox H, Emery JL, Goodbody RA, Yates PO (1964) Neuro-cutaneous melanosis. Arch Dis Child 39:508–516
Woodruff WW Jr, Djang WT, McLendon RE et al (1987) Intracerebral malignant melanoma: high-field-strength MR imaging. Radiology 165:209–213
Haldipur P, Gillies GS, Janson OK et al (2014) Foxc1 dependent mesenchymal signalling drives embryonic cerebellar growth. Elife 3. https://doi.org/10.7554/eLife.03962
De Luca A, Cerrato V, Fuca E et al (2016) Sonic hedgehog patterning during cerebellar development. Cell Mol Life Sci 73:291–230
Narayanan HS, Gandhi DH, Girimaji SR (1987) Neurocutaneous melanosis associated with Dandy-Walker syndrome. Clin Neurol Neurosurg 89:197–200
Peretti-Viton P, Gorincour G, Feuillet L et al (2002) Neurocutaneous melanosis: radiological-pathological correlation. Eur Radiol 12:1349–1353
Chu WC, Lee V, Chan YL et al (2003) Neurocutaneous melanomatosis with a rapidly deteriorating course. AJNR Am J Neuroradiol 24:287–290
D'Souza MM, Prasad A, Sachdev N et al (2011) Neurocutaneous melanosis: assessment on F-18 FDG and [11C]-methionine PET/CT and MRI. Clin Nucl Med 36:906–909
Dupuis F, Sigal R, Margulis A et al (2000) Cerebral magnetic resonance imaging (MRI) in the diagnosis of leptomeningeal carcinomatosis in melanoma patients. Ann Dermatol Venereol 127:29–32
Agero AL, Benvenuto-Andrade C, Dusza SW et al (2005) Asymptomatic neurocutaneous melanocytosis in patients with large congenital melanocytic nevi: a study of cases from an Internet-based registry. J Am Acad Dermatol 53:959–965
Otsuka T, Takayama H, Sharp R et al (1998) c-Met autocrine activation induces development of malignant melanoma and acquisition of the metastatic phenotype. Cancer Res 58:5157–5167
Wehrle-Haller B (2003) The role of Kit-ligand in melanocyte development and epidermal homeostasis. Pigment Cell Res 16:287–296
Acknowledgements
The authors thank Nevus Outreach Inc. for case collection and permission.
This material was presented as a scientific poster at the 2018 American Society of Neuroradiology meeting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Jakchairoongruang, K., Khakoo, Y., Beckwith, M. et al. New insights into neurocutaneous melanosis. Pediatr Radiol 48, 1786–1796 (2018). https://doi.org/10.1007/s00247-018-4205-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4205-x