Abstract
Background
Localized craniofacial scleroderma is a rare pediatric disease that involves a spectrum of discoloration, fibrosis and hemiatrophy of the face and scalp. Children with localized craniofacial scleroderma may have neurological symptoms, and in this context often undergo diagnostic imaging of the brain.
Objective
To catalogue neuroimaging abnormalities in patients with localized craniofacial scleroderma treated at our institution, review their clinical courses and compare this data with prior studies.
Materials and methods
Following Institutional Review Board approval, an imaging database search identified 10 patients with localized craniofacial scleroderma and neuroimaging abnormalities treated at our institution. Neuroimaging exams and the electronic medical record were reviewed for each case.
Results
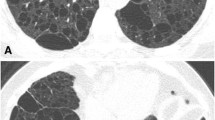
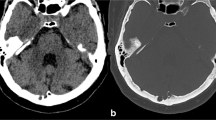
The most common indications for neuroimaging were headache or seizure (80% of cases). The most common neuroimaging abnormalities were T2-hyperintense, subcortical white matter lesions ipsilateral to the cutaneous lesion (90% of cases) on magnetic resonance imaging (MRI). Calcifications or blood products (50%), cysts (40%) and abnormal enhancement (20%) were also observed. A positron emission tomography (PET) scan obtained for a single case demonstrated diminished 18F-fluorodeoxyglucose (FDG) avidity corresponding to the dominant focus of signal abnormality on MRI. Progressive neuroimaging abnormalities were present in 30% of cases. There was no consistent relationship between changes in neurological symptoms following treatment and neuroimaging findings.
Conclusion
Our results are similar to previously published data. In the absence of new or worsening neurological symptoms, the role of neuroimaging for follow-up of localized craniofacial scleroderma is unclear. Knowledge of intracranial neuroimaging abnormalities that are commonly associated with localized craniofacial scleroderma helps to distinguish these lesions from others that have similar appearance.






Similar content being viewed by others
References
Holland KE, Steffes B, Nocton JJ et al (2006) Linear scleroderma en coup de sabre with associated neurologic abnormalities. Pediatrics 117:e132–e136
Holl-Wieden A, Klink T, Klink J et al (2006) Linear scleroderma 'en coup de sabre' associated with cerebral and ocular vasculitis. Scand J Rheumatol 35:402–404
Kister I, Inglese M, Laxer RM et al (2008) Neurologic manifestations of localized scleroderma: a case report and literature review. Neurology 71:1538–1545
Appenzeller S, Montenegro MA, Dertkigil SS et al (2004) Neuroimaging findings in scleroderma en coup de sabre. Neurology 62:1585–1589
Zannin ME, Martini G, Athreya BH et al (2007) Ocular involvement in children with localised scleroderma: a multi-centre study. Br J Ophthalmol 91:1311–1314
Takehara K, Sato S (2005) Localized scleroderma is an autoimmune disorder. Rheumatology (Oxford) 44:274–279
Fett N, Werth VP (2011) Update on morphea: part I. Epidemiology, clinical presentation, and pathogenesis. J Am Acad Dermatol 64:217–228
Fett N, Werth VP (2011) Update on morphea: part II. Outcome measures and treatment. J Am Acad Dermatol 64:231–242
Herrick AL, Ennis H, Bhushan M et al (2010) Incidence of childhood linear scleroderma and systemic sclerosis in the UK and Ireland. Arthritis Care Res (Hoboken) 62:213–218
Zulian F, Athreya BH, Laxer R et al (2006) Juvenile localized scleroderma: clinical and epidemiological features in 750 children. An international study. Rheumatology (Oxford) 45:614–620
Peterson LS, Nelson AM, Su WP (1995) Classification of morphea (localized scleroderma). Mayo Clin Proc 70:1068–1076
Blaszczyk M, Krolicki L, Krasu M et al (2003) Progressive facial hemiatrophy: central nervous system involvement and relationship with scleroderma en coup de sabre. J Rheumatol 30:1997–2004
Lehman TJ (1992) The parry Romberg syndrome of progressive facial hemiatrophy and linear scleroderma en coup de sabre. Mistaken diagnosis or overlapping conditions? J Rheumatol 19:844–845
Tolkachjov SN, Patel NG, Tollefson MM (2015) Progressive hemifacial atrophy: a review. Orphanet J Rare Dis 10:39
Tollefson MM, Witman PM (2007) En coup de sabre morphea and parry-Romberg syndrome: a retrospective review of 54 patients. J Am Acad Dermatol 56:257–263
Chiu YE, Vora S, Kwon EK et al (2012) A significant proportion of children with morphea en coup de sabre and parry-Romberg syndrome have neuroimaging findings. Pediatr Dermatol 29:738–748
Peterson LS, Nelson AM, Su WP (1997) The epidemiology of morphea (localized scleroderma) in Olmsted County 1960–1993. J Rheumatol 24:73–80
Jablonska S, Blaszczyk M (2005) Long-lasting follow-up favours a close relationship between progressive facial hemiatrophy and scleroderma en coup de sabre. J Eur Acad Dermatol Venereol 19:403–404
Duymaz A, Karabekmez FE, Keskin M et al (2009) Parry-Romberg syndrome: facial atrophy and its relationship with other regions of the body. Ann Plast Surg 63:457–461
Orozco-Covarrubias L, Guzman-Meza A, Ridaura-Sanz C et al (2002) Scleroderma 'en coup de sabre' and progressive facial hemiatrophy. Is it possible to differentiate them? J Eur Acad Dermatol Venereol 16:361–366
Kraus V, Lawson EF, von Scheven E et al (2014) Atypical cases of scleroderma en coup de sabre. J Child Neurol 29:698–703
Lis-Swiety A, Brzezinska-Wcislo L, Arasiewicz H (2017) Neurological abnormalities in localized scleroderma of the face and head: a case series study for evaluation of imaging findings and clinical course. Int J Neurosci 127:835–839
Amaral TN, Peres FA, Lapa AT et al (2013) Neurologic involvement in scleroderma: a systematic review. Semin Arthritis Rheum 43:335–347
Bucher F, Fricke J, Neugebauer A et al (2016) Ophthalmological manifestations of Parry-Romberg syndrome. Surv Ophthalmol 61:693–701
Careta MF, Leite Cda C, Cresta F et al (2013) Prospective study to evaluate the clinical and radiological outcome of patients with scleroderma of the face. Autoimmun Rev 12:1064–1069
Stone J, Franks AJ, Guthrie JA et al (2001) Scleroderma "en coup de sabre": pathological evidence of intracerebral inflammation. J Neurol Neurosurg Psychiatry 70:382–385
Goldberg-Stern H, deGrauw T, Passo M et al (1997) Parry-Romberg syndrome: follow-up imaging during suppressive therapy. Neuroradiology 39:873–876
Luer W, Jockel D, Henze T et al (1990) Progressive inflammatory lesions of the brain parenchyma in localized scleroderma of the head. J Neurol 237:379–381
Paprocka J, Jamroz E, Adamek D et al (2006) Difficulties in differentiation of Parry-Romberg syndrome, unilateral facial sclerodermia, and Rasmussen syndrome. Childs Nerv Syst 22:409–415
Sathornsumetee S, Schanberg L, Rabinovich E et al (2005) Parry-Romberg syndrome with fatal brain stem involvement. J Pediatr 146:429–431
Unterberger I, Trinka E, Engelhardt K et al (2003) Linear scleroderma "en coup de sabre" coexisting with plaque-morphea: neuroradiological manifestation and response to corticosteroids. J Neurol Neurosurg Psychiatry 74:661–664
Fain ET, Mannion M, Pope E et al (2011) Brain cavernomas associated with en coup de sabre linear scleroderma: two case reports. Pediatr Rheumatol Online J 9(18)
Longo D, Paonessa A, Specchio N et al (2011) Parry-Romberg syndrome and Rasmussen encephalitis: possible association. Clinical and neuroimaging features. J Neuroimaging 21:188–193
Menascu S, Padeh S, Hoffman C et al (2009) Parry-Romberg syndrome presenting as status migrainosus. Pediatr Neurol 40:321–323
Sakai M, Aoki S, al IY (2008) Silent white matter lesion in linear scleroderma en coup de sabre. J Comput Assist Tomogr 32:822–824
Terstegge K, Kunath B, Felber S et al (1994) MR of brain involvement in progressive facial hemiatrophy (Romberg disease): reconsideration of a syndrome. AJNR Am J Neuroradiol 15:145–150
Bergler-Czop B, Lis-Swiety A, Brzezinska-Wcislo L (2009) Scleroderma linearis: hemiatrophia faciei progressiva (Parry-Romberg syndrom) without any changes in CNS and linear scleroderma "en coup de sabre" with CNS tumor. BMC Neurol 9:39
Asher SW, Berg BO (1982) Progressive hemifacial atrophy: report of three cases, including one observed over 43 years, and computed tomographic findings. Arch Neurol 39:44–46
Cory RC, Clayman DA, Faillace WJ et al (1997) Clinical and radiologic findings in progressive facial hemiatrophy (Parry-Romberg syndrome). AJNR Am J Neuroradiol 18:751–757
David J, Wilson J, Woo P (1991) Scleroderma 'en coup de sabre'. Ann Rheum Dis 50:260–262
Derex L, Isnard H, Revol M (1995) Progressive facial hemiatrophy with multiple benign tumors and hamartomas. Neuropediatrics 26:306–309
Fry JA, Alvarellos A, Fink CW et al (1992) Intracranial findings in progressive facial hemiatrophy. J Rheumatol 19:956–958
Higashi Y, Kanekura T, Fukumaru K et al (2000) Scleroderma en coup de sabre with central nervous system involvement. J Dermatol 27:486–488
Liu P, Uziel Y, Chuang S et al (1994) Localized scleroderma: imaging features. Pediatr Radiol 24:207–209
Menni S, Marzano AV, Passoni E (1997) Neurologic abnormalities in two patients with facial hemiatrophy and sclerosis coexisting with morphea. Pediatr Dermatol 14:113–116
Schievink WI, Mellinger JF, Atkinson JL (1996) Progressive intracranial aneurysmal disease in a child with progressive hemifacial atrophy (Parry-Romberg disease): case report. Neurosurgery 38:1237–1241
Taylor HM, Robinson R, Cox T (1997) Progressive facial hemiatrophy: MRI appearances. Dev Med Child Neurol 39:484–486
Aynaci FM, Sen Y, Erdol H et al (2001) Parry-Romberg syndrome associated with Adie's pupil and radiologic findings. Pediatr Neurol 25:416–418
Carreno M, Donaire A, Barcelo MI et al (2007) Parry Romberg syndrome and linear scleroderma in coup de sabre mimicking Rasmussen encephalitis. Neurology 68:1308–1310
Finley TA, Siatkowski RM (2004) Progressive visual loss in a child with Parry-Romberg syndrome. Semin Ophthalmol 19:91–94
Hulzebos CV, de Vries TW, Armbrust W et al (2004) Progressive facial hemiatrophy: a complex disorder not only affecting the face. A report in a monozygotic male twin pair. Acta Paediatr 93:1665–1669
Moko SB, Mistry Y, Blandin de Chalain TM (2003) Parry-Romberg syndrome: intracranial MRI appearances. J Craniomaxillofac Surg 31:321–324
Okumura A, Ikuta T, Tsuji T et al (2006) Parry-Romberg syndrome with a clinically silent white matter lesion. AJNR Am J Neuroradiol 27:1729–1731
Sandhu K, Handa S (2004) Subdural hygroma in a patient with Parry-Romberg syndrome. Pediatr Dermatol 21:48–50
Shah JR, Juhasz C, Kupsky WJ et al (2003) Rasmussen encephalitis associated with Parry-Romberg syndrome. Neurology 61:395–397
Sommer A, Gambichler T, all B-BM e (2006) Clinical and serological characteristics of progressive facial hemiatrophy: a case series of 12 patients. J Am Acad Dermatol 54:227–233
Verhelst HE, Beele H, Joos R et al (2008) Hippocampal atrophy and developmental regression as first sign of linear scleroderma "en coup de sabre". Eur J Paediatr Neurol 12:508–511
Yano T, Sawaishi Y, Toyono M et al (2000) Progressive facial hemiatrophy after epileptic seizures. Pediatr Neurol 23:164–166
Chiang KL, Chang KP, Wong TT et al (2009) Linear scleroderma "en coup de sabre": initial presentation as intractable partial seizures in a child. Pediatr Neonatol 50:294–298
Qureshi UA, Wani NA, Altaf U (2010) Parry-Romberg syndrome associated with unusual intracranial vascular malformations and phthisis bulbi. J Neurol Sci 291:107–109
Sartori S, Martini G, Calderone M et al (2009) Severe epilepsy preceding by four months the onset of scleroderma en coup de sabre. Clin Exp Rheumatol 27(3 Suppl 54):64–67
Takenouchi T, Solomon GE (2010) Alien hand syndrome in Parry-Romberg syndrome. Pediatr Neurol 42:280–282
Doolittle DA, Lehman VT, Schwartz KM et al (2015) CNS imaging findings associated with Parry-Romberg syndrome and en coup de sabre: correlation to dermatologic and neurologic abnormalities. Neuroradiology 57:21–34
Abdel Razek AA, Alvarez H, Bagg S (2014) Imaging spectrum of CNS vasculitis. Radiographics 34:873–894
Chung MH, Sum J, Morrell MJ et al (1995) Intracerebral involvement in scleroderma en coup de sabre: report of a case with neuropathologic findings. Ann Neurol 37:679–681
Danve A, O'Dell J (2015) The role of 18F fluorodeoxyglucose positron emission tomography scanning in the diagnosis and management of systemic vasculitis. Int J Rheum Dis 18:714–724
Zerizer I, Tan K, Khan S et al (2010) Role of FDG-PET and PET/CT in the diagnosis and management of vasculitis. Eur J Radiol 73:504–509
Sarikaya I (2015) PET studies in epilepsy. Am J Nucl Med Mol Imaging 5:416–430
Ding K, Gupta PK, Diaz-Arrastia R (2016) Epilepsy after traumatic brain injury. In: Laskowitz D, Grant G (eds). Translational research in traumatic brain injury. Front Neurosci, Boca Raton
Rostasy K, Bajer-Kornek B, Venkateswaran S et al (2016) Differential diagnosis and evaluation in pediatric inflammatory demyelinating disorders. Neurology 87(9 Suppl 2):S28–S37
Acknowledgements
Dr. Maloney is supported, in part, through a National Institutes of Health, National Research Service Award training grant held by the University of Washington Gastroenterology Division (grant number 5 T32 DK0072). The authors would like to thank Catherine Amlie-Lefond, M.D., and Heather Brandling-Bennett, M.D., who were instrumental in the early formulations of this project.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Maloney, E., Menashe, S.J., Iyer, R.S. et al. The central nervous system manifestations of localized craniofacial scleroderma: a study of 10 cases and literature review. Pediatr Radiol 48, 1642–1654 (2018). https://doi.org/10.1007/s00247-018-4177-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-018-4177-x