Abstract
Background
Gonadal shielding remains common, but current estimates of gonadal radiation risk are lower than estimated risks to colon and stomach. A female gonadal shield may attenuate active automatic exposure control (AEC) sensors, resulting in increased dose to colon and stomach as well as to ovaries outside the shielded area.
Objective
We assess changes in dose–area product (DAP) and absorbed organ dose when female gonadal shielding is used with AEC for pelvis radiography.
Materials and methods
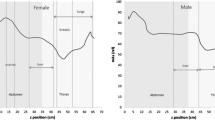
We imaged adult and 5-year-old equivalent dosimetry phantoms using pelvis radiograph technique with AEC in the presence and absence of a female gonadal shield. We recorded DAP and mAs and measured organ absorbed dose at six internal sites using film dosimetry.
Results
Female gonadal shielding with AEC increased DAP 63% for the 5-year-old phantom and 147% for the adult phantom. Absorbed organ dose at unshielded locations of colon, stomach and ovaries increased 21–51% in the 5-year-old phantom and 17–100% in the adult phantom. Absorbed organ dose sampled under the shield decreased 67% in the 5-year-old phantom and 16% in the adult phantom.
Conclusion
Female gonadal shielding combined with AEC during pelvic radiography increases absorbed dose to organs with greater radiation sensitivity and to unshielded ovaries. Difficulty in proper use of gonadal shields has been well described, and use of female gonadal shielding may be inadvisable given the risks of increasing radiation.



Similar content being viewed by others
References
Ardran GM, Crooks HE (1957) Gonad radiation dose from diagnostic procedures. Br J Radiol 30:295–297
Stanford RW, Vance J (1955) The quantity of radiation received by the reproductive organs of patients during routine diagnostic X-ray examinations. Br J Radiol 28:266–273
Abram E, Wilkinson DM, Hodson CJ (1958) Gonadal protection from X radiation for the female. Br J Radiol 31:335–3365
Adran GM, Kemp FH (1957) Protection of the male gonads in diagnostic procedures. Br J Radiol 30:280
Feldman A, Babcock GC, Lanier RR et al (1958) Gonadal exposure dose from diagnostic X-ray procedures. Radiology 71:197–207
International Commission on Radiological Protection (1977) ICRP publication 26: recommendations of the ICRP. Ann ICRP 1
International Commission on Radiological Protection (1991) ICRP publication 60: 1990 recommendations of the ICRP. Ann ICRP 21
International Commission on Radiological Protection (2007) ICRP publication 103: the 2007 recommendations of the International Commission on Radiological Protection. Ann ICRP 37:1–332
Rossi RP, Lin P-JP, Rauch PL et al (1985) AAPM report 14: performance specifications and acceptance testing for X-ray generators and automatic exposure control devices. American Association of Physicists in Medicine, New York
Kaplan SL, Magill D, Felice MA et al (2017) Intussusception reduction: effect of air vs. liquid enema on radiation dose. Pediatr Radiol. https://doi.org/10.1007/s00247-017-3902-1
Wang ZJ, Chen KS, Gould R et al (2011) Positive enteric contrast material for abdominal and pelvic CT with automatic exposure control: what is the effect on patient radiation exposure? Eur J Radiol 79:e58–e62
Paul J, Schell B, Kerl JM et al (2011) Effect of contrast material on image noise and radiation dose in adult chest computed tomography using automatic exposure control: a comparative study between 16-, 64- and 128-slice CT. Eur J Radiol 79:e128–e132
Nguyen KK, Schlaifer AE, Smith DL et al (2012) In automated fluoroscopy settings, does shielding affect radiation exposure to surrounding unshielded tissues? J Endourol 26:1489–1493
Persliden J, Schuwert P, Mortensson W (1996) Comparison of absorbed radiation doses in barium and air enema reduction of intussusception: a phantom study. Pediatr Radiol 26:329–332
Herrmann TL, Fauber TL, Gill J et al (2012) White paper: best practices in digital radiography. American Society of Radiologic Technologists. https://www.asrt.org/docs/default-source/publications/whitepapers/asrt12_bstpracdigradwhp_final.pdf. Accessed 17 Aug 2017
Goske MJ, Charkot E, Herrmann T et al (2011) Image Gently: challenges for radiologic technologists when performing digital radiography in children. Pediatr Radiol 41:611–619
Kenny N, Hill J (1992) Gonad protection in young orthopaedic patients. BMJ 304:1411–1413
Palmer SH, Starritt HC, Paterson M (1998) Radiation protection of the ovaries in young scoliosis patients. Eur Spine J 7:278–281
Wainwright AM (2000) Shielding reproductive organs of orthopaedic patients during pelvic radiography. Ann R Coll Surg Engl 82:318–321
Liakos P, Schoenecker PL, Lyons D et al (2001) Evaluation of the efficacy of pelvic shielding in preadolescent girls. J Pediatr Orthop 21:433–435
McCarty M, Waugh R, McCallum H et al (2001) Paediatric pelvic imaging: improvement in gonad shield placement by multidisciplinary audit. Pediatr Radiol 31:646–649
Sikand M, Stinchcombe S, Livesley PJ (2003) Study on the use of gonadal protection shields during paediatric pelvic X-rays. Ann R Coll Surg Engl 85:422–425
Gul A, Zafar M, Maffulli N (2005) Gonadal shields in pelvic radiographs in pediatric patients. Bull Hosp Jt Dis 63:13–14
Bardo DM, Black M, Schenk K et al (2009) Location of the ovaries in girls from newborn to 18 years of age: reconsidering ovarian shielding. Pediatr Radiol 39:253–259
Fawcett SL, Gomez AC, Barter SJ et al (2012) More harm than good? The anatomy of misguided shielding of the ovaries. Br J Radiol 85:e442–e447
Fawcett SL, Barter SJ (2009) The use of gonad shielding in paediatric hip and pelvis radiographs. Br J Radiol 82:363–370
Frantzen MJ, Robben S, Postma AA et al (2012) Gonad shielding in paediatric pelvic radiography: disadvantages prevail over benefit. Insights Imaging 3:23–32
Lee MC, Lloyd J, Solomito MJ (2017) Poor utility of gonadal shielding for pediatric pelvic radiographs. Orthopedics 40:e623–e627
Karami V, Zabihzadeh M, Shams N, Saki Malehi A (2017) Gonad shielding during pelvic radiography: a systematic review and meta-analysis. Arch Iran Med 20:113–123
Winfeld M, Strubel N, Pinkney L et al (2013) Relative distribution of pertinent findings on portable neonatal abdominal radiographs: can we shield the gonads? Pediatr Radiol 43:1295–1302
American College of Radiology, Society for Pediatric Radiology (2014) ACR-SPR practice parameter for general radiography, amended 2014. Vol RES 30–2013 (Res 39)
Khong PL, Ringertz H, Donoghue V et al (2013) ICRP publication 121: radiological protection in paediatric diagnostic and interventional radiology. Ann ICRP 42:1–63 http://www.icrp.org/publication.asp?id=ICRP%20Publication%20121
Don S (2004) Radiosensitivity of children: potential for overexposure in CR and DR and magnitude of doses in ordinary radiographic examinations. Pediatr Radiol 34:S167–S172
Kaplan SL, Magill D, Felice MA et al (2015) Lead gonad shields: good or bad for patient radiation exposure? Pediatr Radiol 45:S89–S90
Acknowledgements
The authors acknowledge Eatrice Hinton, RT, and Colleen Flowers, RT, for technical assistance and manuscript review.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Appendix 1 Calibration curve
Appendix 1 Calibration curve

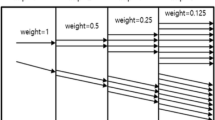
This calibration curve was used to determine absorbed dose from film dosimeters implanted in the phantoms. To make the curve, we exposed film samples (Gafchromic, Ashland) together with a solid state radiation detector (Black Piranha with an external T20 dose probe; RTI Group AB, Sweden) to multiple known amounts of radiation between 2.17 and 124.4 mGy. The solid state detector is calibrated on a 2-year cycle by the manufacturer’s accredited calibration laboratory (ISO/IEC 17025). During calibration the detector is compared to a reference ion chamber, which is traceable through PTB (Germany) to national or international measurement standards. The standard uncertainty of measurement is in compliance with EAL Publication EA-4/02 and is ±1.4% at standard reference condition. The uncertainty increases to ±2.7% when the T20 probe is used with a calibrated Piranha for radiation dose measurements. We measured film green values from these exposures and fit the calibration green values to a three-parameter hyperbolic decay curve as above, where y = film darkening, or mean green value, and x= absorbed dose in mGy. The film was scanned using a commercially available flatbed optical scanner (Mustek Systems Inc., Taiwan). The resultant images were evaluated with ImageJ 1.48v software (National Institutes of Health, Bethesda, MD), and the curve fit for the data was analyzed using Sigma Plot 13 (Systat Software Inc., San Jose, CA). The coefficient of determination R2=0.996, indicated that the exponential decay function fit the calibration data well. We calculated absorbed dose in our experiments by locating the mean green values of our exposed films along this calibration curve.
Rights and permissions
About this article
Cite this article
Kaplan, S.L., Magill, D., Felice, M.A. et al. Female gonadal shielding with automatic exposure control increases radiation risks. Pediatr Radiol 48, 227–234 (2018). https://doi.org/10.1007/s00247-017-3996-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-017-3996-5