Abstract
Background
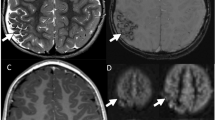
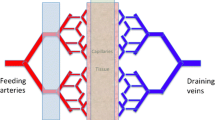
Leigh disease is a metabolic disorder of the mitochondrial respiratory chain culminating in symmetrical necrotizing lesions in the deep gray nuclei or brainstem. Apart from classic gliotic/necrotic lesions, small-vessel proliferation is also characteristic on histopathology. We have observed lesional hyperperfusion on arterial spin-labeling (ASL) sequence in children with Leigh disease.
Objective
In this cross-sectional analysis, we evaluated lesional ASL perfusion characteristics in children with Leigh syndrome.
Materials and methods
We searched the imaging database from an academic children’s hospital for “arterial spin labeling, perfusion, necrosis, lactate, and Leigh” to build a cohort of children for retrospective analysis. We reviewed each child’s medical record to confirm a diagnosis of Leigh disease, excluding exams with artifact, technical limitations, and without ASL images. We evaluated the degree and extent of cerebral blood flow and relationship to brain lesions. Images were compared to normal exams from an aged-matche cohort.
Results
The database search yielded 45 exams; 30 were excluded. We evaluated 15 exams from 8 children with Leigh disease and 15 age-matched normal exams. In general, Leigh brain perfusion ranged from hyperintense (n=10) to hypointense (n=5). Necrotic lesions appeared hypointense/hypoperfused. Active lesions with associated restricted diffusion demonstrated hyperperfusion. ASL perfusion patterns differed significantly from those on age-matched normal studies (P=<.0001). Disease activity positively correlated with cerebral deep gray nuclei hyperperfusion (P=0.0037) and lesion grade (P=0.0256).
Conclusion
Children with Leigh disease have abnormal perfusion of brain lesions. Hyperperfusion can be found in active brain lesions, possibly associated with small-vessel proliferation characteristic of the disease.





Similar content being viewed by others
References
Ruhoy IS, Saneto RP (2014) The genetics of Leigh syndrome and its implications for clinical practice and risk management. Appl Clin Genet 7:221–234
Rahman S, Blok RD, Dahl HH et al (1996) Leigh syndrome: clinical features and biochemical and DNA abnormalities. Ann Neurol 39:343–351
Parikh S, Goldstein A, Koenig MK et al (2015) Diagnosis and management of mitochondrial disease: a consensus statement from the Mitochondrial Medicine Society. Genet Med 17:689–701
Arii J, Tanabe Y (2000) Leigh syndrome: serial MR imaging and clinical follow-up. AJNR Am J Neuroradiol 21:1502–1509
Leigh D (1951) Subacute necrotizing encephalomyelopathy in an infant. J Neurol Neurosurg Psychiatry 14:216–221
Lake NJ, Bird MJ, Isohanni P, Paetau A (2015) Leigh syndrome: neuropathology and pathogenesis 74:482–492
Alsop DC, Detre JA, Golay X et al (2015) Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: a consensus of the ISMRM perfusion study group and the European consortium for ASL dementia. Magn Reson Med 73:102–116
Wintermark M, Lepori D, Cotting J et al (2004) Brain perfusion in children: evolution with age assessed by quantitative perfusion computed tomography. Pediatrics 113:1642–1652
Gropman AL (2013) Mitochondrial mechanisms and neurological disorders. Neurotherapeutics 10:185
Gropman AL (2013) Neuroimaging in mitochondrial disorders. Neurotherapeutics 10:273–285
Takahashi S, Oki J, Miyamoto A et al (1999) Proton magnetic resonance spectroscopy to study the metabolic changes in the brain of a patient with Leigh syndrome. Brain Dev 21:200–204
Krageloh-Mann I, Grodd W, Schoning M et al (1993) Proton spectroscopy in five patients with Leigh’s disease and mitochondrial enzyme deficiency. Dev Med Child Neurol 35:769–776
Jurkiewicz E, Chelstowska S, Pakula-Kosciesza I et al (2011) Proton MR spectroscopy in patients with Leigh syndrome. Neuroradiol J 24:424–428
Barkovich AJ, Patay Z (2012) Metabolic, toxic, and inflammatory brain disorders. In: Barkovich AJ, Raybaud C (eds) Pediatric neuroimaging, 5th edn. Lippincott Williams & Wilkins, Philadelphia, pp 178–182
Delonlay P, Rotig A, Sarnat HB (2013) Respiratory chain deficiencies. Handb Clin Neurol 113:1651–1666
Whitehead MT, Fricke S, Gropman A (2015) Structural brain defects. Clin Perinatol 242:337–361
Hegde AN, Mohan S, Lath N et al (2011) Differential diagnosis for bilateral abnormalities of the basal ganglia and thalamus. Radiographics 31:5–30
Deibler AD, Pollock JM, Kraft RA et al (2008) Arterial spin-labeling in routine clinical practice, part 1: techniques and artifacts. AJNR Am J Neuroradiol 29:1228–1234
Deibler AR, Pollock JM, Kraft RA et al (2008) Arterial spin-labeling in routine clinical practice, part 2: hypoperfusion patterns. AJNR Am J Neuroradiol 29:1235–1241
Deibler AR, Pollock JM, Kraft RA et al (2008) Arterial spin-labeling in routine clinical practice, part 3: hyperperfusion patterns. AJNR Am J Neuroradiol 29:1428–1435
László A, Ambrus E, Vörös E et al (2009) 99-mTc-HMPAO single photon emission computed tomography examinations in genetically determined neurometabolic disorders. Ideggyogy Sz 62:168–177
Yen TC, Yeh SH (1995) 99mTc-HMPAO brain single photon emission computerized tomography in mitochondrial encephalomyopathies. Zhongua Yi Xue Za Zhi 56:287–291
Chen Z, Li J, Lou X et al (2012) Sequential evaluation of brain lesions using functional magnetic resonance imaging in patients with Leigh syndrome. Nan Fang Yi Ke Da Xue Xue Bao 32:1474–1477
Chi CS, Lee HF, Tsai CR et al (2011) Lactate peak on brain MRS in children with syndromic mitochondrial diseases. J Chin Med Assoc 74:305–359
Sijens PE, Smit GP, Rodiger LA et al (2008) MR spectroscopy of the brain in Leigh syndrome. Brain Dev 30:579–583
Detre JA, Wang ZY, Bogdan AR et al (1991) Regional variation in brain lactate in Leigh syndrome by localized 1H magnetic resonance spectroscopy. Ann Neurol 29:218–221
Avula S, Parikh S, Demarest S et al (2014) Treatment of mitochondrial disorders. Curr Treat Options Neurol 16:292
Todd MM, Weeks J (1996) Comparative effects of propofol, pentobarbital, and isoflurane on cerebral blood flow and blood volume. J Neurosurg Anesthesiol 8:296–303
Wang J, Licht DJ, Jahng GH et al (2003) Pediatric perfusion imaging using pulsed arterial spin labeling. J Magn Reson Imaging 18:404–413
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None
Rights and permissions
About this article
Cite this article
Whitehead, M.T., Lee, B. & Gropman, A. Lesional perfusion abnormalities in Leigh disease demonstrated by arterial spin labeling correlate with disease activity. Pediatr Radiol 46, 1309–1316 (2016). https://doi.org/10.1007/s00247-016-3616-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00247-016-3616-9