Abstract
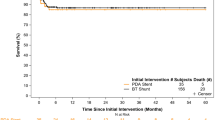
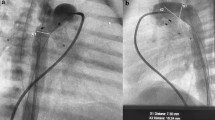
Duct-dependent pulmonary circulation has traditionally been addressed by the Blalock–Taussig–Thomas shunts (BTTS). Recently, catheter-based alternatives such as ductal stenting have emerged as a particularly advantageous option, especially in resource-constrained settings. This article delves into the nuances of ductal stenting within low-resource environments, highlighting its relative ease of application, reduced morbidity, and cost-effectiveness as key factors in its favor. Comparisons in mortality between the two procedures are however likely to be confounded by selection biases. Ductal stenting appears to be particularly beneficial for palliating older infants and children with cyanotic congenital heart disease and diminished pulmonary blood flow who present late. Additionally, it serves as a valuable tool for left ventricular training in late-presenting transposition with an intact ventricular septum. A meticulous pre-procedure echocardiographic assessment of anatomy plays a pivotal role in planning access and hardware, with additional imaging seldom required for this purpose. The adaptation of adult coronary hardware has significantly enhanced the technical feasibility of ductal stenting. However, challenges such as low birth weight and sepsis specifically impact the performance of ductal stenting and patient recovery in low-resource environments. There is potential for systematic application of quality improvement processes to optimize immediate and long-term outcomes of ductal stenting. There is also a need to prospectively examine the application of ductal stenting in low-resource environments through multi-center registries.





Similar content being viewed by others
Data Availability
Data will be maintained for 5 years after publication.
Material Availability
Not applicable.
References
Sasikumar D, Prabhu MA, Kurup R, Francis E, Kumar S, Gangadharan ST, Mahadevan KK, Sivasankaran S, Kumar RK (2023) Outcomes of neonatal critical congenital heart disease: results of a prospective registry-based study from South India. Arch Dis Child. https://doi.org/10.1136/archdischild-2023-325471
Sasikumar N, Hermuzi A, Fan CS, Lee KJ, Chaturvedi R, Hickey E, Honjo O, Van Arsdell GS, Caldarone CA, Agarwal A, Benson L (2017) Outcomes of Blalock–Taussig shunts in current era: a single center experience. Congenital Heart Dis 12(6):808–814. https://doi.org/10.1111/chd.12516
Glatz AC, Petit CJ, Goldstein BH, Kelleman MS, McCracken CE, McDonnell A, Buckey T, Mascio CE, Shashidharan S, Ligon RA, Ao J, Whiteside W, Wallen WJ, Metcalf CM, Aggarwal V, Agrawal H, Qureshi AM (2018) Comparison between patent ductus arteriosus stent and modified Blalock-Taussig shunt as palliation for infants with ductal-dependent pulmonary blood flow: insights from the congenital catheterization research collaborative. Circulation 137:589–601. https://doi.org/10.1161/CIRCULATIONAHA.117.029987
Bentham JR, Zava NK, Harrison WJ, Shauq A, Kalantre A, Derrick G, Chen RH, Dhillon R, Taliotis D, Kang S-L, Crossland D, Adesokan A, Hermuzi A, Kudumula V, Yong S, Noonan P, Hayes N, Stumper O, Thomson JDR (2018) Duct stenting versus modified Blalock–Taussig shunt in neonates with duct-dependent pulmonary blood flow: associations with clinical outcomes in a multicenter national study. Circulation 137:581–588. https://doi.org/10.1161/CIRCULATIONAHA.117.028972
Alsagheir A, Koziarz A, Makhdoum A, Contreras J, Alraddadi H, Abdalla T, Benson L, Chaturvedi RR, Honjo O (2021) Duct stenting versus modified Blalock–Taussig shunt in neonates and infants with duct-dependent pulmonary blood flow: a systematic review and meta-analysis. J Thorac Cardiovasc Surg 161(2):379-390.e8. https://doi.org/10.1016/j.jtcvs.2020.06.008
Alwi M, Choo KK, Latiff HA, Kandavello G, Samion H, Mulyadi MD (2004) Initial results and medium-term follow-up of stent implantation of patent ductus arteriosus in duct-dependent pulmonary circulation. J Am Coll Cardiol 44(2):438–445. https://doi.org/10.1016/j.jacc.2004.03.066
Mahesh K, Kannan BR, Vaidyanathan B, Kamath P, Anil SR, Kumar RK (2005) Stenting the patent arterial duct to increase pulmonary blood flow. Indian Heart J 57(6):704–8
Pezzella T (2002) Worldwide maldistribution of access to cardiac surgery. J Thorac Cardiovasc Surg 123:1016–1017
Saxena A (2018) Congenital heart disease in india: a status report. Indian Pediatr 55(12):1075–1082
Vervoort D, Meuris B, Meyns B, Verbrugghe P (2020) Global cardiac surgery: access to cardiac surgical care around the world. J Thorac Cardiovasc Surg. 159:987-996.e6
Lingaswamy D, Koepcke L, Krishna MR, Kottayil BP, Sunil GS, Moynihan K, Seshadri B, Kumar RK (2020) Catheter-based palliation for infants with tetralogy of Fallot. Cardiol Young 30(10):1469–1472. https://doi.org/10.1017/S1047951120002334
Sasikumar N, Mohanty S, Balaji S, Kumar RK (2022) Rescue right ventricular outflow tract stenting for refractory hypoxic spells. Catheter Cardiovasc Interv. https://doi.org/10.1002/ccd.30522
Brown KL, Crowe S, Franklin R, McLean A, Cunningham D, Barron D, Tsang V, Pagel C, Utley M (2015) Trends in 30-day mortality rate and case mix for paediatric cardiac surgery in the UK between 2000 and 2010. Open Heart 2(1):e000157. https://doi.org/10.1136/openhrt-2014-000157
Dorobantu DM, Pandey R, Sharabiani MT, Mahani AS, Angelini GD, Martin RP, Stoica SC (2016) In- dications and results of systemic to pulmonary shunts: results from a national database. Eur J Cardiothorac Surg 49:1553–1563
Bove T, Vandekerckhove K, Panzer J, De Groote K, De Wolf D, François K (2015) Disease-specific outcome analysis of palliation with the modified Blalock–Taussig shunt. World J Pediatr Cong Heart Surg 6:67–74
Petrucci O, O’Brien SM, Jacobs ML, Jacobs JP, Manning PB, Eghtesady P (2011) Risk factors for mor- tality and morbidity after the neonatal Blalock–Taussig shunt procedure. Ann Thorac Surg 92:642–652
Dorobantu DM, Pandey R, Sharabiani MT, Mahani AS, Angelini GD, Martin RP, Stoica SC (2016) In- dications and results of systemic to pulmonary shunts: results from a national database. Eur J Cardiothorac Surg 49:1553–1563
Tseng SY, Truong VT, Peck D, Kandi S, Brayer S, Jason DP 3rd, Mazur W, Hill GD, Ashfaq A, Goldstein BH, Alsaied T (2022) Patent ductus arteriosus stent versus surgical aortopulmonary shunt for initial palliation of cyanotic congenital heart disease with ductal-dependent pulmonary blood flow: a systematic review and meta-analysis. J Am Heart Assoc 11(13):e024721. https://doi.org/10.1161/JAHA.121.024721
Lingaswamy D, Koepcke L, Krishna MR, Kottayil BP, Sunil GS, Moynihan K, Balaji S, Kumar RK (2020) Catheter-based palliation for infants with tetralogy of Fallot. Cardiol Young. https://doi.org/10.1017/S1047951120002334
Francis E, Kumar S, Kumar RK (2014) Palliative stenting of patent ductus arteriosus in older children and young adults with congenital cyanotic heart disease. Catheter Cardiovasc Interv 83:1109–1111
Kothari SS, Ramakrishnan S, Senguttuvan NB, Gupta SK, Bisoi AK (2011) Ductal recanalization and stenting for late presenters with TGA intact ventricular septum. Ann Pediatr Cardiol 4(2):135–138. https://doi.org/10.4103/0974-2069.84651
Gunasekara CM, Moynihan K, Sudhakar A, Sunil GS, Kotayil BP, Bayya PR, Kumar RK (2020) Neonatal cardiac surgery in low resource settings: implications of birth weight. Arch Dis Child 105(12):1140–1145. https://doi.org/10.1136/archdischild-2020-319161
Gopalakrishnan RM, Nair AR, Sudhakar A, Jayant A, Balachandran R, Neema PK, Kumar RK (2022) Culture-negative sepsis after pediatric cardiac surgery: incidence and outcomes. Ann Pediatr Cardiol. 15(5–6):442–446. https://doi.org/10.4103/apc.apc_37_22
Acknowledgements
We would like to acknowledge the assiatance of Dr Krishna Prasenan, Reserach Assistant, Department of Pediatric Cardiology in typesetting the manuscript.
Author information
Authors and Affiliations
Contributions
Criteria for authorship: Navaneetha Sasikumar: conceptualization, data curation, formal analysis, investigation, methodology, supervision, visualization, writing—original draft preparation , writing—review and editing. Pranoti Toshniwal: data curation, formal analysis, visualization, writing—original draft preparation, writing—review and editing. Abish Sudhakar: data curation, formal analysis, investigation, methodology, writing—review and editing. Praveen Reddy Bayya: data curation, formal analysis, visualization, writing—original draft preparation, writing—review and editing. Raman Krishna Kumar: conceptualization, formal analysis, investigation, methodology, resources, supervision, validation, visualization, writing—original draft preparation , writing—review and editing.
Corresponding author
Ethics declarations
Competing Interests
The authors declare no competing interests.
Ethical Approval
None. No interference with clinical management, no patient identifiers collected.
Informed Consent
Not available.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Sasikumar, N., Toshniwal, P., Bayya, P.R. et al. Ductal Stenting in Low-Resource Environments. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03496-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03496-8