Abstract
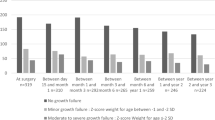
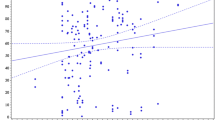
Closure of the large ventricular septal defects (VSD) in infancy can lead to normalization of growth, but data are limited. Our study is done to assess the growth pattern in different age groups of children and lower birth weight babies after shunt closure. This is a prospective observational study that included infants with isolated large VSD operated in infancy. Anthropometric data were collected at baseline and at follow-up, and growth patterns were analyzed. 99 infants were included in the study. The mean age and weight at the time of surgery were 6.97 ± 2.79 months and 5.07 ± 1.16 kg, respectively. The mean follow-up duration was 8.99 ± 2.31 months. The weight for age (W/A) was the most adversely affected parameter preoperatively, and there was significant improvement noted in the mean Z score for W/A after shunt closure (− 3.67 ± 1.18 vs. − 1.76 ± 1.14, p = 0.0012). There was improvement in Z-scores for length for age (L/A) and weight for length (W/L), although it was not statistically significant. The infants from all the age groups had statistically significant growth in the anthropometric parameters. The rate of weight gain was maximum in the infants operated below 8 months of age (2–4 months = 3588 g, 5–6 months = 3592 g, 7–8 months = 3606 g, 9–10 months = 2590 g, 11–12 months = 2250 g). Low birth weight and normal birth weight infants had similar Z-scores at the time of surgery and at follow-up in all 3 anthropometric parameters, and birth weight did not affect pre- as well as post-operative growth parameters. Suboptimal improvement in weight and length was seen in 40 and 20% of babies even after successful surgical repair, respectively. Growth failure in infants with a large VSD can be multifactorial. Early surgical closure of the shunt can lead to early normalization of growth parameters and faster catch-up growth. Few babies may fail to demonstrate a positive growth response even after timely surgical correction, and may be related to intrauterine and genetic factors or faulty feeding habits.



Similar content being viewed by others
Data Availability
No datasets were generated or analysed during the current study.
Abbreviations
- ACC:
-
Aortic cross clamp
- ASD:
-
Atrial septal defect
- CCF:
-
Congestive cardiac failure
- CHD:
-
Congenital heart defect
- CPB:
-
Cardiopulmonary bypass
- ICU:
-
Intensive care unit
- L/A:
-
Length for age
- LBW:
-
Low birth weight
- LRTI:
-
Lower respiratory tract infection
- PDA:
-
Patent ductus arteriosus
- VSD:
-
Ventricular septal defect
- W/A:
-
Weight for age
- W/L:
-
Weight for length
References
Wren C, Richmond S, Donaldson L (2000) Temporal variability in birth prevalence of cardiovascular malformations. Heart 83(4):414–419. https://doi.org/10.1136/heart.83.4.414
Cresti A, Giordano R, Koestenberger M et al (2018) Incidence and natural history of neonatal isolated ventricular septal defects: do we know everything? A 6-year single-center Italian experience follow-up. Congenital Heart Dis 13(1):105–112. https://doi.org/10.1111/chd.12528
Levy RJ, Rosenthal A, Fyler DC, Nadas AS (1978) Birthweight of infants with congenital heart disease. Am J Dis Child 132(3):249–254. https://doi.org/10.1001/archpedi.1978.02120280033007
Greenwood RD, Rosenthal A, Parisi L, Fyler DC, Nadas AS (1975) Extracardiac abnormalities in infants with congenital heart disease. Pediatrics 55(4):485–492
Jacobs JP, Mayer JE Jr, Mavroudis C et al (2017) The society of thoracic surgeons congenital heart surgery database: 2017 update on outcomes and quality. Ann Thorac Surg 103(3):699–709. https://doi.org/10.1016/j.athoracsur.2017.01.004
Bhatt M, Roth SJ, Kumar RK et al (2004) Management of infants with large, unrepaired ventricular septal defects and respiratory infection requiring mechanical ventilation. J Thorac Cardiovasc Surg 127(5):1466–1473. https://doi.org/10.1016/j.jtcvs.2003.11.030
Levy RJ, Rosenthal A, Miettinen OS, Nadas AS (1978) Determinants of growth in patients with ventricular septal defect. Circulation 57(4):793–797. https://doi.org/10.1161/01.cir.57.4.793
Vaidyanathan B, Roth SJ, Gauvreau K, Shivaprakasha K, Rao SG, Kumar RK (2006) Somatic growth after ventricular septal defect in malnourished infants. J Pediatr 149(2):205–209. https://doi.org/10.1016/j.jpeds.2006.04.012
Manso PH, Carmona F, Jácomo AD, Bettiol H, Barbieri MA, Carlotti AP (2010) Growth after ventricular septal defect repair: does defect size matter? A 10-year experience. Acta Paediatr 99(9):1356–1360. https://doi.org/10.1111/j.1651-2227.2010.01801.x
Correia Martins L, Lourenço R, Cordeiro S et al (2016) Catch-up growth in term and preterm infants after surgical closure of ventricular septal defect in the first year of life. Eur J Pediatr 175(4):573–579. https://doi.org/10.1007/s00431-015-2676-4
Bloomfield DK (1964) The natural history of ventricular septal defect in patients surviving infancy. Circulation 29:914–955. https://doi.org/10.1161/01.cir.29.6.914
Schuurmans FM, Pulles-Heintzberger CFM, Gerver WJM, Kester ADM, Forget P-P (1998) Long-term growth of children with congenital heart disease: a retrospective study. Acta Paediatr 87:1250–1255. https://doi.org/10.1111/j.1651-2227.1998.tb00947
Menahem S (1972) The clinical growth of infants and children with ventricular septal defects. Aust Paediatr J 8(1):1–15. https://doi.org/10.1111/j.1440-1754.1972.tb01780.x
Collins G, Calder L, Rose V, Kidd L, Keith J (1972) Ventricular septal defect: clinical and hemodynamic changes in the first five years of life. Am Heart J 84(5):695–705. https://doi.org/10.1016/0002-8703(72)90186-x
Saxena A, Relan J, Agarwal R et al (2019) Indian guidelines for indications and timing of intervention for common congenital heart diseases: revised and updated consensus statement of the working group on management of congenital heart diseases. Ann Pediatr Cardiol 12(3):254–286. https://doi.org/10.4103/apc.APC_32_19
Anderson BR, Stevens KN, Nicolson SC et al (2013) Contemporary outcomes of surgical ventricular septal defect closure. J Thorac Cardiovasc Surg 145(3):641–647. https://doi.org/10.1016/j.jtcvs.2012.11.032
Inohara T, Ichihara N, Kohsaka S et al (2019) The effect of body weight in infants undergoing ventricular septal defect closure: a report from the nationwide Japanese congenital surgical database. J Thorac Cardiovasc Surg 157(3):1132-1141.e7. https://doi.org/10.1016/j.jtcvs.2018.11.111
Kogon B, Butler H, Kirshbom P, Kanter K, McConnell M (2008) Closure of symptomatic ventricular septal defects: how early is too early? Pediatr Cardiol 29(1):36–39. https://doi.org/10.1007/s00246-007-9016-z
Bayer LM, Robinson SJ (1969) Growth history of children with congenital heart defects. Size according to sex, age decade, surgical status, and diagnostic category. Am J Dis Child 117(5):564–572. https://doi.org/10.1001/archpedi.1969.02100030566011
Weintraub RG, Menahem S (1991) Early surgical closure of a large ventricular septal defect: influence on long-term growth. J Am Coll Cardiol 18(2):552–558. https://doi.org/10.1016/0735-1097(91)90614-f
Funding
The authors have not disclosed any funding.
Author information
Authors and Affiliations
Contributions
SW prepared the manuscript. DK contributed toward data collection and statistical analysis. AMB, SPR, and KK contributed toward dietary advice and patient follow-up. SK revised and finalized the manuscript.
Corresponding author
Ethics declarations
Conflict interest
The authors have not disclosed any competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wadile, S., Kondgekar, D., Banpurkar, A.M. et al. How do Age at the Surgery and Birth Weight Influence Post-Operative Anthropometric Parameters in Infants with Surgical Closure of Large Ventricular Septal Defects? A Prospective Cohort Study from a Lower-Middle-Income Country. Pediatr Cardiol (2024). https://doi.org/10.1007/s00246-024-03486-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-024-03486-w