Abstract
The best strategy for lead management in children is a matter of debate, and our experiences are limited. This is a retrospective single-center study comparing difficulties and outcomes of transvenous lead extraction (TLE) implanted ich childhood and at age < 19 years (childhood-implanted-childhood-extracted, CICE) and at age < 19 (childhood-implanted-adulthood-extracted, CIAE). CICE patients—71 children (mean age 15.1 years) as compared to CIAE patients (114 adults (mean age 28.61 years) were more likely to have VVI than DDD pacemakers. Differences in implant duration (7.96 vs 14.08 years) appeared to be most important, but procedure complexity and outcomes also differed between the groups. Young adults with cardiac implantable electronic device implanted in childhood had more risk factors for major complications and underwent more complex procedures compared to children. Implant duration was significantly longer in CIAE patients than in children, being the most important factor that had an impact on patient safety and procedure complexity. CIAE patients were more likely to have prolonged operative duration and more complex procedures due to technical problems, and they were 2–3 times more likely to require second-line or advanced tools compared to children, but the rates of clinical and procedural success were comparable in both groups. The difference between the incidence of major complications between CICE and CIAE patients is very clear (MC 2.9 vs 7.0%, hemopericardium 1.4 vs 5.3% etc.), although statistically insignificant. Delay of lead extraction to adulthood seems to be a riskier option than planned TLE in children before growing up.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The number of new cardiac implantable electronic device (CIED) implantations in children is not rising. However, due to advances in cardiovascular techniques, the number of young adults with repaired congenital heart as well as children with implanted cardiac devices can be expected to have increased longevity into adulthood (negligible mortality).
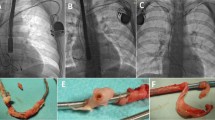
Although reports show long-term durability of leads pacemakers (PM) 20 years, implantable cardioverter-defibrillator (ICD) 10 years [1, 2] these values are usually lower in children [3,4,5,6,7]. In children, mechanical damage and other types of lead dysfunction resulting from body growth, faster scarring and calcification, lead insulation breaches and a more active lifestyle limit the durability of intracardiac leads [3,4,5,6,7] (Fig. 1).
The strain of the leads caused by the growth of the body. The strain of the leads caused by the growth of the body, which is one of the causes of lead dysfunction (increase of the stimulation threshold, decrease of resistance due to damage to external insulation). Pictures typical of young adolescents with leads implanted in childhood (A–D). Abandoned epicardial leads implanted earlier in early childhood are common (B and C). In children and youth, single-chamber systems (A, C and D) predominate
Lead replacement as the optimal lead management strategy for children with lead dysfunction is recommended both in previous and recent guidelines [8,9,10], but execution of the strategy in pediatric electrocardiology departments may differ. Differences in transvenous lead extraction (TLE) and procedure difficulty between children and adolescents have been discussed in several reports [11,12,13,14,15,16,17] and multicentre studies [7, 18]. Most pediatric cardiologists prefer a passive approach, that is lead removal for class 1 and 2a indications and extraction postponement in patients with class 2b indications [5, 18,19,20]. Considering the optimal time for lead extraction some investigators advocate waiting until children stop growing than extracting non-functional leads during physical growth, suggesting that TLE in young adults is safer [18,19,20].
As a result, most children, once they turn 18, are referred to adult electrophysiologists for potential lead replacement or system upgrade. Finally, most young adults become candidates for TLE at adult centers.
No previous study has investigated the effects of postponing TLE to an undefined time as long as the leads meet the criteria of functionality (without analysis of their age and their radiological image, often suggesting impending dysfunction). Furthermore, there have been no studies that compare the effectiveness and safety of TLE in adolescents with leads implanted in childhood and TLE in children. This knowledge gap prompted us to conduct this study.
The aim of the study was to compare the complexity, effectiveness, and outcomes after TLE in children (below the age of 19 years) from pediatric wards and TLE in young adults (with leads implanted in childhood) performed at a high-volume center for adult patients. We sought to determine which strategy is better for children with borderline functional leads: to delay lead replacement as long as possible or to perform TLE in childhood even for class 2b indications.
Methods
Study Population
This post hoc analysis used clinical data of 3741 patients who underwent transvenous lead extraction between 2006 and 2022. The first group consisted of 71 children from 5 to 19 (mean age 15.10 ± 2.95 years) who were < 19 at first CIED implantation and transvenous lead extraction (childhood-implanted-childhood-extracted patients, CICE). The second group consisted of 114 young adults from 19 to 57 (mean age 28.61 ± 9.36 years) who were < 19 at first CIED implantation but > 19 during TLE (childhood-implanted-adulthood-extracted patients, CIAE). No other exclusion criteria were used.
Lead Extraction Procedure
The procedures of TLE were defined according to the HRS 2009 and 2017 and EHRA 2018 guidelines [8,9,10] on management of lead-related complications. TLE procedures were performed in a stepwise manner using mechanical systems such as polypropylene Byrd dilator sheaths (Cook® Medical, Leechburg, PA, USA), mainly via the lead implant vein. If technical difficulties arose, alternative venous approaches and/or additional tools such as Evolution (Cook® Medical, USA), TightRail (Phillips®, USA), lassos, basket catheters were used. Laser cutting sheaths were not used. In both study groups lead extractions were performed by the same experienced a team. Indications for TLE and type of periprocedural complications were defined according to the HRS Expert Consensus Statement on lead extraction [8, 9].
Definitions
Clinical success, procedural success, partial radiographic success, as well as major and minor complications of TLE were defined in accordance with recommendations for lead management [8,9,10]. The occurrence of permanent bodily injury, significant damage to the tricuspid valve or, for example, stroke, procedure-related death despite optimal treatment, have precluded clinical or procedural success [8,9,10].
The risk of major complications (MC) related to TLE (points, percentage) was assessed using the SAFeTY TLE score, an online tool available at http://alamay2.linuxpl.info/kalkulator/ [21]. The EROS score was used for prediction of significant procedural complications that required emergent surgical intervention (1–3 scale) [22]. Assessment of procedure complexity was based on the MB score showing the need for use of advanced tools to achieve TLE success (0–5 points) [23], LED index referring to lead extraction difficulty based on fluoroscopy times (0–50 points) [24], and Advanced TLE Techniques (Mazzone) score to predict the necessity of using advanced extraction techniques (0–4 points) [25].
Procedure complexity was expressed as procedure time, i.e., time for extraction of all leads (sheath-to-sheath time) and average time of single lead extraction (sheath-to sheath/number of extracted leads). The occurrence of unexpected procedural difficulties referred to as technical problems, i.e., the circumstances that made the procedure more difficult but without complications was another indicator of procedural complexity. Most commonly it was the need to use venous approach other than the access vein, lead-on-lead scarring, fracture of the targeted lead, Byrd dilator collapse/torsion and occlusion of the access vein [26,27,28].
Lead Failure
Mechanical Lead Damage (Electric Failure)
Sudden increase in impedance > 1500 Ohm or high-voltage impedance > 100 Ohm; > 300 nonphysiological short interventricular-intervals (“crackles”).
Non-damaged Lead Dysfunction
Lead failure without mechanical damage: exit/entry block (linear increase in impedance > 1500 Ohm or high-voltage impedance > 100 Ohm or a linear decrease in sensing or increase of pacing threshold to an inacceptable level level), tip dislodgement or extracardiac pacing).
Abnormal Lead Route
Strain of the Leads
Is a radiological image of an electrode that has become too short over time, which may hide a properly functioning electrode or any of the above-mentioned abnormalities. Strain of the leads indicates increased difficulty in removing the lead (close contact of the lead with the venous system and cardiac structures) and indicates an increased risk of future damage to the strained lead.
Abnormal Lead Loop in the Heart
A radiological image in which a lead that is too long (at the time of implantation) creates an intentional or unintentional loop in the heart, atrium or ventricle, or the loop crosses the tricuspid valve. The presence of loops increases the contact of the lead with cardiac structures and scarring at the contact sites, hinders lead dilatation and increases the risk of damage to cardiac structures (including the tricuspid valve).
Extracted Lead Designs
In our material, all implanted PM leads had a conventional design, most of them with active fixation and steroid-eluting. The ICD leads were single-coil. Active leads were most often used, also due to their isodiametric nature. VDD leads were not used in children due to their design (distance between tip and atrial ring electrodes). The studied groups did not include Medtronic 3830 lm-less leads.
Statistical Analysis
Depending on whether the data is normally distributed continuous variables are summarized with a mean ± standard deviation (SD) or median and interquartile range (IQR). Categorical variables are summarized using counts and percentages. The significance of differences between groups was determined using the Chi2 test with Yates correction or Student’s t-test or Mann–Whitney U test, as appropriate. Statistical analysis was performed with Statistica 13.3 (TIBCO Software Inc.).
All patients gave their informed written consent to undergo TLE and use anonymous data from their medical records, approved by the Bioethics Committee.
Results
Comparison of patient characteristics (Table 1) shows that age difference on the day of TLE was 13.51 years (15.10 vs 28.61 years), and age difference on the day of lead implantation 6.25 years (7.13 vs 13.38 years) and this resulted from the assumptions of the study. There was a smaller proportion of women in the CICE group than in the CIAE group (28.17 vs 44.74%). The most common indication for TLE in both groups was mechanical lead damage (electrical failure), more frequent in children (67.61 vs 43.86%).
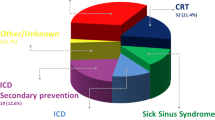
CICE patients more frequently received simple single-chamber PM (67.61 vs 30.70%), whereas CIAE patients were more likely to receive dual-chamber PM (61.40 vs 19.72%). Furthermore, CIAE patients had more leads in the heart (1.91 vs 1.34), more frequently abandoned leads (17.54 vs 7.04%), leads on both sides of the chest (8.77 vs 2.82%) and abnormally long lead loops in the heart before TLE (Fig. 2).
Planned lead loops to prevent progressive lead length deficit as the child grows. Planned lead loops to prevent progressive lead length deficit as the child grows (A–D). Long-term observations showed the ineffectiveness of this technique because the loops grew attached to the walls of the heart, which made it impossible to straighten them and sometimes did not prevent the dysfunction (A), and significantly hinders their transvenous extraction. The technique is abandoned today, however, the phenomenon is often encountered in young patients
A huge difference in dwell time of the oldest lead per patient before TLE (169.0 vs 95.52 months) and global implant duration (25.00 vs 9.50 years) appeared to be the most important factors influencing procedure difficulty, complexity and safety (Table 2).
Several factors allow us to predict procedural risk and difficulty, whereas retrospective analysis may shed some light on the development of major complications and procedure complexity (Table 3).
The CIAE group was characterized by more extracted leads per patient (1.75 vs 1.16), extraction of multiple leads (three or more) (7.90 vs 1.41%), need to use other than lead vein approach (9.65 vs 2.82%), extraction of leads with too long loops in the heart (26.32 vs 0.00%), and extraction of abandoned lead(s) (16.67 vs 4.23%). Some differences were not significant, but there was a noticeable tendency (Fig. 2).
Dwell time of the oldest extracted lead (169.0 vs 86.52) and cumulative dwell time of extracted leads, i.e., the sum of extracted lead dwell times (20.67 vs 8.58 years) provide the most important information.
The bottom row of the Table 3 summarizes the usefulness of the most popular calculators, scales, and scores for assessment of procedure safety and difficulty (complexity).
The SAFeTY TLE score assessing the risk of major complications [21] showed 4.13 times higher risk of MC, the EROS 3 score [22] showed 9.13 times higher of risk of significant procedural complications that required urgent surgical intervention, the MB score 4 and 5 [23] showed 18.35 times higher need for advanced tools to achieve TLE success, the LED index exceeding 14 points [24] indicated 6.64 times higher risk of difficult TLE based on fluoroscopy time, Advanced TLE Techniques (Mazzone) [25] score 3 and 4 predicted 3.59 times higher need for advanced extraction techniques in CIAE patients as compared to CICE patients. All calculators, scales, and scores predicted a higher risk of MC and procedure difficulty (complexity) in CIAE patients.
The venue of TLE in CIAE patients has evolved with years from an EP-LAB via a cardiac surgical operating theater to a hybrid room. Lead extractions in CICE patients were performed in children’s hospital, first in the cardiac surgical operating room or later in the hybrid room. Most TLEs were done in patients under general anesthesia. Continuous TEE monitoring was introduced 7 years ago in adult departments and 4 years ago in children’s departments (Table 4).
Procedure duration expressed as a median of sheath-to-sheath time (19.00 vs 9.00 min) was longer in CIAE patients, which was a result of a larger number of extracted leads; the median of single lead extraction time (sheath-to-sheath/number of extracted leads) was not significantly different from that in CICE patients (11.50 vs 9.00; P = 0.247).
Non-functional superfluous leads were more commonly extracted in CIAE patients (16.67 vs 4.23%). It is also worth underlining that young adults were 4 times more likely to undergo extraction of abandoned leads (which is a risk factor for major complications of TLE) compared to children.
Extraction procedures can be prolonged or complicated by occlusion of the access vein (subclavian region), Byrd dilator collapse/torsion/“fracture,” lead break during extraction, lead-on-lead scarring, need to use alternative venous approach, loss of free lead portion, need to extract non-targeted leads. The problems must be solved, thus prolonging the procedure (they are not major or minor complications of TLE). As Table 4 shows, unexpected technical problems occurred twice (or more) as frequently in CIAE patients. It should be highlighted that multiple (in the same patient) unexpected difficulties were nearly 3 times more common in CIAE patients. In CIAE patients the second-line tools (Evolution, TightRail, metal sheaths, lasso catheters / snares) were used 1.5 (or more) times more often than in children.
Major complications were more often in CIAE than CICE patients (7.02 vs 2.87%), i.e., hemopericardium (5.26 vs 1.41%), need for urgent cardiac repair (5.26 vs 1.41%). (Table 5).
TLE effectiveness expressed as lack of partial radiographic success (16.67 vs 12.68%), clinical (95.61 vs 97.18%) and procedural (84.21 vs 84.51%) was lower in CIAE patients. Summing up, in young patients with leads implanted in childhood (CIAE) all complications occurred more frequently than in children: major complications (any)—2.5 times, hemopericardium—3.73 times, significant or severe tricuspid valve damage—1.2 times more frequently (Table 5).
Discussion
This study attempts to answer the question which is better: to extract leads in childhood (for class 2b indications) during physical growth or to wait for lead replacement until children stop growing or perhaps to postpone it as far into the future as possible. Our analysis showed that in young adults with leads implanted in childhood (CIAE) implant duration was 1.8 times longer than in children (CICE). As a consequence, CIAE patients underwent more complex procedures due to the occurrence of various unexpected technical problems, and they were 2–3 times more likely to require second-line or advanced tools compared to children.
Moreover, all complications occurred more frequently in CIAE than in CICE patients: major complications (any)—1.6 times, hemopericardium—2.6 times, significant and severe tricuspid valve damage—3.3 times more frequently. Finally, we demonstrated that TLE was more difficult and associated with higher risk in young adults than in children.
The PACELEAD survey on lead extraction in children and adults [18] demonstrated that > 70% of responders favored lead abandonment for class 2b indications. The survey showed a tendency toward lead abandonment over lead extraction, especially in complex cases. Lead abandonment is still an accepted strategy in many hospitals [5, 14, 18,19,20, 29].
Although the risk associated with TLE can be slightly higher in children [7, 11,12,13,14,15,16,17,18], there are several tools (calculators, scores, scales) that allow us to predict the real risk of TLE in individual patients [21,22,23,24,25]. The risk of major complications can be assessed using the SAFeTY TLE score [21] and EROS score [22], whereas procedure complexity can be predicted using the MB score, LED score, Advanced LE score [23,24,25]. We showed that all the calculators, scales, and scores indicated much more difficult and riskier TLE in young people with leads implanted in childhood (CIAE) than in children (CICE).
As mentioned in the Introduction section, transitioning from childhood to adulthood with old or very old leads, if still officially “functional,” poses an additional challenge. Correct or only “acceptable” values of pacing/sensing/impedance do not indicate long-term lead durability because of body growth [1, 3,4,5,6, 12, 18]. Such functional leads can be strained or coiled [30, 31], strongly adherent to the heart [11,12,13,14,15,16]. They are usually covered with a thick film of calcified scar tissue, which damages external lead insulation [32]. Limited lead durability, especially in children and young patients [3,4,5,6,7, 14, 18] creates the need for lead replacement or new lead implantation with abandonment of non-functional leads [18]. Only a few reports described the problems related to abandoned leads in children and young adults [6, 13, 19, 20, 29]. Our experience shows that lead abandonment approach in children, juveniles, and young adults may create much more serious problems 10–20 years later. Silvetti et al. in their study reported that two of 18 patients with abandoned leads developed lead endocarditis at 5 and 10 years after lead abandonment (11.1%) [20].
We selected eight reports on TLE in children and juveniles [7, 11,12,13,14,15,16,17,18] comparing mean patient age, implant duration, major complications, and occurrence of procedure-related death. (Table 6) There are 5 reports (151 children) in which mean patients age was < 18 years (about 12.4 years) and 2 reports (1023 children, juveniles, and young adults) in which mean patients age was > 18 years (about 19.3 years). There is no report on TLE in a specific group of adult patients with leads implanted in childhood. The Table 6 shows that mean age of children and young adults in the literature is 18.1 years and average dwell time of extracted leads is 38.8 months. The respective values in our groups were 15.10 years and 94.9 months for children (CICE), and 28.5 years and 173.7 months for adults (CIAE) (for uniformity, age of leads was expressed as a mean). This indicates that adults with leads implanted in childhood (CIAE) are very specific candidates for TLE. The rate of major complications reported in the literature was 3.8% in total, whereas in our study the rate of major complications was 2.8% in children (CICE group) and as high as 7.0% in adults (CIAE group).
The conclusion from this Table 6 is that a passive approach to lead management and delay of lead replacement until adulthood, or occurrence of serious complications in children creates a group of patients in whom lead extraction is most difficult and risky.
Our results further support the attitudes of Cecchin et al. who clearly explained that “Our approach has been to embrace the logic that most individuals with expected longevity > 20 years should have nonfunctioning leads removed to leave room for the future and avoid a more difficult procedure down the line” [15].
“Prophylactic extraction” of functional but old or very old leads is still a matter of debate. Evidence collected over the last 3 decades shows that the risk associated with lead extraction doubles every 3 years and lead lifetime is limited [1,2,3,4,5,6,7, 14, 18, 29]. An important issue which remains to be solved is to decide which is better: prophylactic lead replacement in children who stopped growing or waiting for dysfunction of gradually older leads. Our experience shows that symptomatic patients with unexpected lead failure are at risk of being admitted to a provincial hospital where they receive an additional lead without even considering lead replacement. It is the most common reason for lead abandonment which translated into more complex lead extraction at a later time (demonstrated in our study and previous studies in adults) [33, 34]. A general conclusion is that a passive approach to lead management and delay of lead replacement far into the future and the occurrence of serious complications in children and in juveniles creates a group of patients in whom lead extraction is most difficult and risky.
This paper provides some clues to the electrophysiologists performing TLE in adults, and gentle suggestions for future revision of the guidelines on lead management strategy in patients with leads implanted in childhood.
Although the PACES recommendations recommend adapting the implanted system optimally to the disease and type of cardiac arrhythmia, the selection of the CIED system is often determined by factors such as the expected height of the child and the expected deficit in lead length, faster lead wear and tear than in adults and the expected need to replace the lead after 10–12 years—cause the some children to receive a single-chamber system. This is not a generally accepted strategy, but it seems at least acceptable [35].
The main limitation of this study is that it involved only patients undergoing transvenous lead extraction, whereas there was no possibility of assessing patients with system upgrade without TLE procedures. The organizational model of TLE procedures evolved over time (procedures in adults 03, 2006–08, 2022, procedures in children 01, 2007–08, 2022). A mechanical-only approach to lead extraction was used throughout the study (no laser energy). Finally, all procedures in this study were performed by the same very experienced extractor and his team (co-operator, heart surgeon, nurses), therefore it may not give an overview of TLE safety and efficacy in children and young adults.
Our Most Important Finds
Young adults with leads implanted in childhood were more likely to undergo complex procedures with major complications compared to children. Implant duration was significantly longer in young adults than in children, which appeared to be the most important factor influencing procedure safety and complexity. Compared to children, young adults had longer and more complex extraction procedures, and they were 2–3 times more likely to require second-line tools. All technical complications were also more common, but the rates of complete radiographic, clinical and procedural success were comparable.
Conclusion
Delay of lead extraction to adulthood seems to be a riskier option than planned TLE in children before growing up.
References
Mori H, Kato R, Ikeda Y, Tsutsui K, Hoya H, Tanaka S, Iwanaga S, Nakano S, Muramatsu T, Sumitomo N, Matsumoto K (2021) Transvenous lead performance of implantable cardioverter-defibrillators and pacemakers. Pacing Clin Electrophysiol 44:481–489
Sterns LD (2019) Pacemaker lead surveillance and failure: is there a signal in the noise? Heart Rhythm 16:579–580
Janson CM, Patel AR, Bonney WJ, Smoots K, Shah MJ (2014) Implantable cardioverter-defibrillator lead failure in children and young adults: a matter of lead diameter or lead design? J Am Coll Cardiol 63:133–140
Rausch CM, Hughes BH, Runciman M, Law IH, Bradley DJ, Sujeev M, Duke A, Schaffer M, Collins KK (2010) Axillary versus infraclavicular placement for endocardial heart rhythm devices in patients with pediatric and congenital heart disease. Am J Cardiol 106:1646–1651
Silvetti MS, Drago F, Marcora S, Rav L (2007) Outcome of single-chamber, ventricular pacemakers with transvenous leads implanted in children. Europace 9:894–899
Fortescue EB, Berul CI, Cecchin F, Walsh EP, Triedman JK, Alexander ME (2004) Patient, procedural, and hardware factors associated with pacemaker lead failures in pediatrics and congenital heart disease. Heart Rhythm 1:150–159
Atallah J, Erickson CC, Cecchin F, Dubin AM, Law IH, Cohen MI, Lapage MJ, Cannon BC, Chun TU, Freedenberg V, Gierdalski M (2013) Pediatric and congenital electrophysiology society (PACES). Multi-institutional study of implantable defibrillator lead performance in children and young adults: results of the pediatric lead extractability and survival evaluation (PLEASE) study. Circulation 12:2393–2402
Wilkoff BL, Love CJ, Byrd CL, Bongiorni MG, Carrillo RG, Crossley GH 3rd, Epstein LM, Friedman RA, Kennergren CE, Mitkowski P, Schaerf RH, Wazni OM (2009) Heart Rhythm Society; American Heart Association. Transvenous lead extraction: heart Rhythm Society expert consensus on facilities, training, indications, and patient management: this document was endorsed by the American Heart Association (AHA). Heart Rhythm 6:1085–1104
Kusumoto FM, Schoenfeld MH, Wilkoff B, Berul CI, Birgersdotter-Green UM, Carrillo R, Cha YM, Clancy J, Deharo JC, Ellenbogen KA, Exner D, Hussein AA, Kennergren C, Krahn A, Lee R, Love CJ, Madden RA, Mazzetti HA, Moore JC, Parsonnet J, Patton KK, Rozner MA, Selzman KA, Shoda M, Srivathsan K, Strathmore NF, Swerdlow CD, Tompkins C, Wazni O (2017) 2017 HRS expert consensus statement on cardiovascular implantable electronic device lead management and extraction. Heart Rhythm 14:e503–e551
Bongiorni MG, Burri H, Deharo JC, Starck C, Kennergren C, Saghy L, Rao A, Tascini C, Lever N, Kutarski A, Fernandez Lozano I, Strathmore N, Costa R, Epstein L, Love C, Blomstrom-Lundqvist C, ESC Scientific Document Group (2018) 2018 EHRA expert consensus statement on lead extraction: recommendations on definitions, endpoints, research trial design, and data collection requirements for clinical scientific studies and registries: endorsed by APHRS/HRS/LAHRS. Europace 20:1217
Friedman RA, Van Zandt H, Collins E, LeGras M, Perry J (1996) Lead extraction in young patients with and without congenital heart disease using the subclavian approach. Pacing Clin Electrophysiol 19:778–783
Cooper JM, Stephenson EA, Berul CI, Walsh EP, Epstein LM (2003) Implantable cardioverter defibrillator lead complications and laser extraction in children and young adults with congenital heart disease: implications for implantation and management. J Cardiovasc Electrophysiol 14:344–349
Moak JP, Freedenberg V, Ramwell C, Skeete A (2006) Effectiveness of excimer laser-assisted pacing and ICD lead extraction in children and young adults. Pacing Clin Electrophysiol 29:461–466
Dilber E, Karagöz T, Celiker A (2009) Lead extraction in children and young adults using different techniques. Med Princ Pract 18:356–359
Cecchin F, Atallah J, Walsh EP, Triedman JK, Alexander ME, Berul CI (2010) Lead extraction in pediatric and congenital heart disease patients. Circ Arrhythm Electrophysiol 3:437–444
Zartner PA, Wiebe W, Toussaint-Goetz N, Schneider MB (2010) Lead removal in young patients in view of lifelong pacing. Europace 12:714–718
McCanta AC, Tanel RE, Gralla J, Runciman DM, Collins KK (2014) The fate of nontargeted endocardial leads during the extraction of one or more targeted leads in pediatrics and congenital heart disease. Pacing Clin Electrophysiol 37:104–108
McCanta AC, Schaffer MS, Collins KK (2011) Pediatric and adult congenital endocardial lead extraction or abandonment decision (PACELEAD) survey of lead management. Pacing Clin Electrophysiol 34:1621–1627
Suga C, Hayes DL, Hyberger LK, Lloyd MA (2000) Is there an adverse outcome from abandoned pacing leads? J Interv Card Electrophysiol 4:493–499
Silvetti MS, Drago F (2008) Outcome of young patients with abandoned, nonfunctional endocardial leads. Pacing Clin Electrophysiol 31:473–479
Jacheć W, Polewczyk A, Polewczyk M, Tomasik A, Kutarski A (2020) Transvenous lead extraction SAFeTY score for risk stratification and proper patient selection for removal procedures using mechanical tools. J Clin Med 9:361
Sidhu BS, Ayis S, Gould J, Elliott MK, Mehta V, Kennergren C, Butter C, Deharo JC, Kutarski A, Maggioni AP, Auricchio A, Kuck KH, Blomström-Lundqvist C, Bongiorni MG, Rinaldi CA, ELECTRa Investigators Group (2021) Risk stratification of patients undergoing transvenous lead extraction with the ELECTRa Registry Outcome Score (EROS): an ESC EHRA EORP European lead extraction ConTRolled ELECTRa registry analysis. Europace 23:1462–1471
Bontempi L, Curnis A, Della Bella P, Cerini M, Radinovic A, Inama L, Melillo F, Salghetti F, Marzi A, Gargaro A, Giacopelli D, Mazzone P (2020) The MB score: a new risk stratification index to predict the need for advanced tools in lead extraction procedures. Europace 22:613–621
Bontempi L, Vassanelli F, Cerini M, Inama L, Salghetti F, Giacopelli D, Gargaro A, Raweh A, Curnis A (2017) Predicting the difficulty of a transvenous lead extraction procedure: validation of the LED index. J Cardiovasc Electrophysiol 28:811–818
Mazzone P, Tsiachris D, Marzi A, Ciconte G, Paglino G, Sora N, Sala S, Vergara P, Gulletta S, Della BP (2013) Predictors of advanced lead extraction based on a systematic stepwise approach: results from a high-volume center. Pacing Clin Electrophysiol 36:837–844
Kutarski A, Czajkowski M, Pietura R, Obszanski B, Polewczyk A, Jachec W, Polewczyk M, Mlynarczyk K, Grabowski M, Opolski G (2018) Effectiveness, safety, and long-term outcomes of non-powered mechanical sheaths for transvenous lead extraction. Europace 20:1324–1333
Kutarski A, Polewczyk M, Polewczyk AM, Polewczyk A (2017) A relevant Byrd dilator sheath damage during transvenous lead extraction – the rare phenomenon with potentially serious consequences. Heart Beat 2:1–8
Kutarski A, Jacheć W, Tułecki Ł, Czajkowski M, Nowosielecka D, Stefańczyk P, Tomków K, Polewczyk A (2022) Disparities in transvenous lead extraction in young adults. Sci Rep 12:9601
Berul CI, Van Hare GF, Kertesz NJ, Dubin AM, Cecchin F, Collins KK, Cannon BC, Alexander ME, Triedman JK, Walsh EP, Friedman RA (2008) Results of a multicenter retrospective implantable cardioverterdefibrillator registry of pediatric and congenital heart disease patients. J Am Coll Cardiol 51:1685–1691
Gabbarini F, Golzio PG, Bordese R, Agnoletti G (2014) Reforming of intracardiac lead loops in pediatric patients. Int J Cardiol 171:e86–e87
Stojanov P, Velimirović D, Hrnjak V, Pavlović SU, Zivković M, Djordjević Z (1998) Absorbable suture technique: solution to the growth problem in pediatric pacing with endocardial leads. Pacing Clin Electrophysiol 21:65–68
Kołodzińska A, Kutarski A, Koperski Ł, Grabowski M, Małecka B, Opolski G (2012) Differences in encapsulating lead tissue in patients who underwent transvenous lead removal. Europace 14:994–1001
Jacheć W, Polewczyk A, Segreti L, Bongiorni MG, Kutarski A (2019) To abandon or not to abandon: late consequences of pacing and ICD lead abandonment. Pacing Clin Electrophysiol 42:1006–1017
Segreti L, Rinaldi CA, Claridge S, Svendsen JH, Blomstrom-Lundqvist C, Auricchio A, Butter C, Dagres N, Deharo JC, Maggioni AP, Kutarski A, Kennergren C, Laroche C, Kempa M, Magnani A, Casteigt B, Bongiorni MG, ELECTRa Investigators (2019) Procedural outcomes associated with transvenous lead extraction in patients with abandoned leads: an ESC-EHRA ELECTRa (European Lead Extraction ConTRolled) Registry Sub-Analysis. Europace 21:645–654
Writing Committee Members, Shah MJ, Silka MJ, Silva JNA, Balaji S, Beach CM, Benjamin MN, Berul CI, Cannon B, Cecchin F, Cohen MI, Dalal AS, Dechert BE, Foster A, Gebauer R, Gonzalez Corcia MC, Kannankeril PJ, Karpawich PP, Kim JJ, Krishna MR, Kubuš P, LaPage MJ, Mah DY, Malloy-Walton L, Miyazaki A, Motonaga KS, Niu MC, Olen M, Paul T, Rosenthal E, Saarel EV, Silvetti MS, Stephenson EA, Tan RB, Triedman J, Bergen NHV, Wackel PL (2021) 2021 PACES expert consensus statement on the indications and management of cardiovascular implantable electronic devices in pediatric patients. Heart Rhythm 18:1888–1924
Acknowledgements
We would like to thank all doctors participating in TLE procedures.
Author information
Authors and Affiliations
Contributions
AK supervision, original draft editing, first operator MM-K supervision, writing-review MB investigation, data curation MB. investigation, data curation, co-operator WL investigation, data curation, co-operator WJ methodology, statistical study, draft preparation BZ investigation, data curation AP supervision, writing-review ŁT investigation, data curation, co-operator MC investigation, data curation, co-operator DN investigation, data curation, corresponding author, KB supervision, writing-review All authors reviewed the manuscript
Corresponding author
Ethics declarations
Conflict of interest
The author’s declared that they have no conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kutarski, A., Miszczak-Knecht, M., Brzezinska, M. et al. Lead Extraction in Children and Young Adults: When is the Best Time for Lead/System Replacement?. Pediatr Cardiol (2023). https://doi.org/10.1007/s00246-023-03320-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-023-03320-9