Abstract
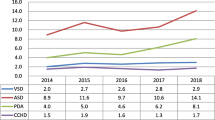
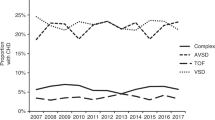
Several studies have suggested an inverse relationship between lower socioeconomic status (SES) and the incidence of congenital heart disease (CHD) among live births. We sought to examine this relationship further in a Canada-wide population study, exploring CHD subtypes, trends, and associated noncardiac abnormalities. Infants born in Canada (less Quebec) from 2008 to 2018 with CHD requiring intervention in the first year were identified using ICD-10 codes through the Canadian Institute for Health Information Discharge Abstract Database. Births of CHD patients were stratified by SES (census-based income quintiles) and compared against national birth proportions using X2 tests. Proportions with extracardiac defects (ED) and nonlethal genetic syndromes (GS) were also explored. From 2008 to 2018, 7711 infants born with CHD were included. The proportions of major CHD distributed across SES quintiles were 27.1%, 20.1%, 19.2%, 18.6%, and 15.0% from lowest to highest, with significant differences relative to national birth proportions (22.0%, 20.0%, 20.6%, 20.7%, and 16.7% from lowest (1) to highest (5)) (p < 0.0001). No temporal trends in the CHD proportions across SES categories were observed over the study period. The distribution across SES quintiles was different only for specific CHD subtypes (double-outlet right ventricle (n = 485, p = 0.03), hypoplastic left heart syndrome (n = 547, p = 0.006), heterotaxy (n = 224, p = 0.03), tetralogy of Fallot (n = 1007, p = 0.008), truncus arteriosus (n = 126, p < 0.0001), and ventricular septal defect (n = 1916, p < 0.0001)), with highest proportions observed in the lowest quintile. The proportion of the total population with ED but not GS was highest in lower SES quintiles (< 0.0001) commensurate with increased proportion of CHD. Our study suggests a negative association between SES and certain CHD lesions and ED.


Similar content being viewed by others
References
Liu Y et al (2019) Global birth prevalence of congenital heart defects 1970–2017: updated systematic review and meta-analysis of 260 studies. Int J Epidemiol 48(2):455–463
Moons P et al (2010) Temporal trends in survival to adulthood among patients born with congenital heart disease from 1970 to 1992 in Belgium. Circulation 122(22):2264–2272
Marelli AJ et al (2014) Lifetime prevalence of congenital heart disease in the general population from 2000 to 2010. Circulation 130(9):749–756
GBD 2017 Congenital Heart Disease Collaborators (2020) Global, regional, and national burden of congenital heart disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Child Adolesc Health 4(3):185–200
Yang BY et al (2021) Maternal exposure to ambient air pollution and congenital heart defects in China. Environ Int 153:106548
Ngwezi D, Hornberger L, Vargas A (2018) Environmental pollution and the development of congenital heart disease: a scoping review. Adv Pediatric Res 5:17
Ngwezi DP et al (2018) Tracking trends in emissions of developmental toxicants and potential associations with congenital heart disease in Alberta, Canada. Challenges 9(2):28
Ngwezi DP et al (2018) Industrial developmental toxicants and congenital heart disease in urban and rural Alberta, Canada. Challenges 9(2):26
Yu D et al (2014) Maternal socioeconomic status and the risk of congenital heart defects in offspring: a meta-analysis of 33 studies. PLoS ONE 9(10):e111056
Miao Q et al (2023) Association between maternal marginalization and infants born with congenital heart disease in Ontario Canada. BMC Public Health 23:790
Peyvandi S et al (2020) Environmental and socioeconomic factors influence the live-born incidence of congenital heart disease: a population-based study in California. J Am Heart Assoc 9(8):e015255
Egbe A et al (2014) Changing prevalence of severe congenital heart disease: a population-based study. Pediatr Cardiol 35(7):1232–1238
Davey B et al (2021) Social determinants of health and outcomes for children and adults with congenital heart disease: a systematic review. Pediatr Res 89(2):275–294
Best KE et al (2019) Socio-economic inequalities in mortality in children with congenital heart disease: a systematic review and meta-analysis. Paediatr Perinat Epidemiol 33(4):291–309
Kuciene R, Dulskiene V (2009) Maternal socioeconomic and lifestyle factors during pregnancy and the risk of congenital heart defects. Medicina (Kaunas) 45(11):904–909
Agha MM et al (2011) Socioeconomic status and prevalence of congenital heart defects: does universal access to health care system eliminate the gap? Birth Defects Res A Clin Mol Teratol 91(12):1011–1018
Carmichael SL, Ma C, Shaw GM (2009) Socioeconomic measures, orofacial clefts, and conotruncal heart defects in California. Birth Defects Res A Clin Mol Teratol 85(10):850–857
Adams MM, Mulinare J, Dooley K (1989) Risk factors for conotruncal cardiac defects in Atlanta. J Am Coll Cardiol 14(2):432–442
Yang J et al (2008) Socioeconomic status in relation to selected birth defects in a large multicentered US case-control study. Am J Epidemiol 167(2):145–154
Long J, Ramadhani T, Mitchell LE (2010) Epidemiology of nonsyndromic conotruncal heart defects in Texas, 1999–2004. Birth Defects Res A Clin Mol Teratol 88(11):971–979
Purkey NJ et al (2019) Birth location of infants with critical congenital heart disease in California. Pediatr Cardiol 40(2):310–318
Correa-Villaseñor A et al (1991) White-black differences in cardiovascular malformations in infancy and socioeconomic factors. The Baltimore-Washington Infant Study Group. Am J Epidemiol 134(4):393–402
Baron AM et al (2001) Congenital heart disease in the Medicaid population of Southern Arizona. Am J Cardiol 88(4):462–465
Kaur A, Hornberger L, Fruitman D, Ngwezi DP, Eckersley L (2022) Impact of location of residence and socioeconomic status on prenatal detection of congenital heart disease in a jurisdiction of universal health coverage. Ultrasound Odstet Gynecol 60:359
Bennett S, Eckersley L, Kaur A, Fruitman D, Hornberger LK (2022) Impact of socioeconomic status and remoteness of residence on fetal outcomes in major CHD. J Am Coll Cardiol 79(9):1971
Krishnan A et al (2021) Impact of socioeconomic status, race and ethnicity, and geography on prenatal detection of hypoplastic left heart syndrome and transposition of the great arteries. Circulation 143(21):2049–2060
Kaur A et al (2022) Trends in the prenatal detection of major congenital heart disease in Alberta from 2008–2018. J Obstet Gynaecol Can 44(8):895–900
Rivera LA, Lebenbaum M, Rosella LC (2015) The influence of socioeconomic status on future risk for developing Type 2 diabetes in the Canadian population between 2011 and 2022: differential associations by sex. Int J Equity Health 14:101
Ospina M et al (2020) Socioeconomic gradients of adverse birth outcomes and related maternal factors in rural and urban Alberta, Canada: a concentration index approach. BMJ Open 10(1):e033296
Persson M et al (2019) Maternal overweight and obesity and risk of congenital heart defects. J Am Coll Cardiol 73(1):44–53
McLaren L (2007) Socioeconomic status and obesity. Epidemiol Rev 29:29–48
Janssen I et al (2006) Influence of individual- and area-level measures of socioeconomic status on obesity, unhealthy eating, and physical inactivity in Canadian adolescents. Am J Clin Nutr 83(1):139–145
Helle E, Priest JR (2020) Maternal obesity and diabetes mellitus as risk factors for congenital heart disease in the offspring. J Am Heart Assoc 9(8):e011541
Chou FS, Chakradhar R, Ghimire LV (2021) Socioeconomic and racial disparities in the prevalence of congenital heart disease in infants of diabetic mothers. J Matern Fetal Neonatal Med 34(24):4167–4170
Siahpush M et al (2006) Socioeconomic variations in nicotine dependence, self-efficacy, and intention to quit across four countries: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control 15(Suppl 3):iii71–iii75
Malik S et al (2008) Maternal smoking and congenital heart defects. Pediatrics 121(4):e810–e816
Carmichael SL et al (2007) Maternal food insecurity is associated with increased risk of certain birth defects. J Nutr 137(9):2087–2092
Qu Y et al (2021) Maternal folic acid supplementation mediates the associations between maternal socioeconomic status and congenital heart diseases in offspring. Prev Med 143:106319
Sotres-Alvarez D et al (2013) Maternal dietary patterns are associated with risk of neural tube and congenital heart defects. Am J Epidemiol 177(11):1279–1288
Ou Y et al (2016) Risk factors of different congenital heart defects in Guangdong. China Pediatr Res 79(4):549–558
Olugbuyi O et al (2022) Impact of socioeconomic status and residence distance on infant heart disease outcomes in Canada. J Am Heart Assoc 11(18):e026627
Luo ZC, Wilkins R, Kramer MS (2006) Effect of neighbourhood income and maternal education on birth outcomes: a population-based study. CMAJ 174(10):1415–1420
McCrindle BW et al (1996) An increased incidence of total anomalous pulmonary venous drainage among aboriginal Canadians. Can J Cardiol 12(1):81–85
Sharma AK et al (2020) Assessing childhood health outcome inequalities with area-based socioeconomic measures: a retrospective cross-sectional study using Manitoba population data. Pediatr Res 88(3):496–502
Funding
The study was funded as part of Dr. Kaul’s Heart and Stroke Foundation Chair. The Foundation had no input into the design, analysis, or interpretation.
Author information
Authors and Affiliations
Contributions
CS (graduate student) and YO (clinical pediatric cardiology trainee) were co first authors who drove all aspects of the research, generating a proposal outlining plans for the research, generating the data from the administrative dataset, performing statistical analyses and generating the manuscript. PK (epidemiologist and research scientist) and LKH (clinical and research pediatric cardiologist) were co-senior supervising faculty who initiated and assisted the first authors in developing the study, overseeing data acquisition, mining, analyses and interpretation and generating the manuscript at every step. LKH is the submitting and corresponding author. DD (senior analyst) and SI (g=postdoctoral student) mined and collected the CIHI data, and assisted both CS and YO data analysis and interpretation. They also reviewed and provided input into the manuscript. DD also generated the final figures and tables with CS and reviewed the statistical analyses for accuracy. AM and LE are pediatric cardiologists who have assisted the development of this project, initially part of the scholarship oversight committee of Dr Olugbuyi, made important contributions to refining the data requested and ultimately collected, reviewed analyses and were important in the interpretation of data, assisted with critical review of the manuscript and input. All authors reviewed, contributed to and approved of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no conflicts of interest relevant to this article to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Smith, C., Olugbuyi, O., Kaul, P. et al. Lower Socioeconomic Status is Associated with an Increased Incidence and Spectrum of Major Congenital Heart Disease and Associated Extracardiac Pathology. Pediatr Cardiol 45, 433–440 (2024). https://doi.org/10.1007/s00246-023-03310-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-023-03310-x