Abstract
Prenatal diagnosis (preDx) of critical congenital heart disease (CCHD) decreases neonatal morbidity and mortality. Obstetrical fetal cardiac imaging guidelines in 2013 aimed to increase preDx. The objectives of this study were to determine the contemporary preDx rate of CCHD and identify maternal–fetal factors and variations in prenatal care that may be potential barriers. This retrospective single center study evaluated maternal demographics and characteristics of infants with CCHD (requiring cardiac catheterization or surgical intervention before 6 months-old) between 2016 and 2019. 58% of the 339 infants with CCHD had preDx. Infants with preDx were more likely to have mothers ≥ 35 years-old (p = 0.028), family history of CHD (p = 0.017), health insurance (p = 0.002), or anatomic scan with perinatology (p < 0.001). Hispanic infants were less likely to have preDx (45.6%, p = 0.005). PreDx rates were higher in infants with extracardiac/genetic anomalies (p < 0.001) and significantly different between CCHD subtypes (76% for single ventricle, 51% for biventricular/four-chamber view, 59% for proximal outflow tract anomalies, and 48% for distal great artery anomalies; p = 0.024). In infants without preDx, 25% of their mothers had indication for, but did not undergo, fetal echocardiography. PreDx rates of CCHD remains inadequate across subtypes detectable by standard fetal cardiac screening views, particularly in uninsured and Hispanic communities.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Congenital heart disease (CHD) is the most common congenital anomaly affecting approximately 1% of live births [1]. Critical congenital heart disease (CCHD) is a subset of CHD consisting of lesions that require early surgical or transcatheter intervention during infancy to allow for survival. Infants with critical congenital heart disease are at risk for increased rates of morbidity and mortality if not medically supported in a timely manner after birth [2]. Prenatal diagnosis of CCHD allows for multidisciplinary coordination of care, counseling, parental decision making, genetic testing, and psychosocial support. Risk stratification of prenatally diagnosed patients determines appropriate levels of care, with decisions about timing and mode of delivery, and if needed, allows immediate postnatal access to specialists, such as neonatologists, pediatric cardiologists, and pediatric cardiovascular surgeons [3]. Prenatally diagnosed fetuses with CCHD that are transferred for delivery at or near higher level pediatric cardiac centers have improved outcomes with decreased morbidity [4,5,6,7] and lower overall healthcare costs [8].
Prenatal diagnosis of CHD relies on detection by obstetric ultrasound and confirmation by fetal echocardiography. A fetal echocardiogram is recommended in pregnancies at risk for CHD based on maternal and/or fetal indications [9]. However, the majority of CHD occurs in low risk pregnancies, [10, 11] and thus prenatal diagnosis requires suspicion for fetal cardiac anomaly on screening obstetric ultrasounds. The detection of or suspicion for CHD requires careful evaluation of standard fetal cardiac views. Certain anomalies, such as hypoplastic left heart syndrome, are detectable in a standard four-chamber view. Other anomalies such as tetralogy of Fallot, transposition of the great arteries, and coarctation of the aorta may have normal appearing four-chamber views and require additional views involving the cardiac outflow tracts and/or great arteries. CCHD, in the vast majority of conditions, involves anomalies of the outflow tracts. In 2013, the American Institute of Ultrasound Medicine, American College of Obstetrics and Gynecology, American College of Radiology and Society of Radiologists in Ultrasound released new guidelines for routine obstetric anatomic ultrasounds to include views of the right and left cardiac outflow tracts in addition to the previously recommended four-chamber view of the fetal heart [12]. These updated guidelines were released based on previous studies showing low detection rates of CCHD in the United States with routine obstetrical ultrasounds, ranging from 12 to 53% [5]. Since the new guidelines were released, studies have shown no significant improvement in prenatal detection rates of critical outflow tract anomalies [13]. A prior retrospective analysis of patients seen at Rady Children’s Hospital compared pre- 2013-guideline and post-guideline detection rates of critical outflow tract anomalies, demonstrated that the prenatal detection rate increased only from 52 to 61%, and hypothesized that the low increase in detection rates was due to suboptimal obstetrical implementation and training on the updated guidelines [13]. If a mother is appropriately referred for a fetal echocardiogram, a detailed fetal echocardiogram performed by a specialized fetal cardiac sonographer or cardiologist and reviewed by a pediatric cardiologist with specialized training in advanced imaging results in highly accurate diagnosis of CHD [14, 15] and appropriate prenatal multidisciplinary care. This study seeks to determine the contemporary rate of prenatal diagnosis in infants with CCHD and identify maternal–fetal factors and variations in prenatal care that may be potential barriers to prenatal diagnosis.
Methods
Study Design/Subject Selection
This retrospective single center study evaluated maternal demographics and characteristics of infants with CCHD (defined as requiring cardiac catheterization or surgical intervention before 6 months-old) seen at Rady Children’s Hospital (RCHSD)/University of California, San Diego (UCSD) from October 2016 to December 2019. Eligible mother/infant pairs were identified through the RCHSD Heart Institute cardiac catheterization, cardiovascular surgery, and echocardiogram databases in addition to electronic medical record queries. Data collection was performed through retrospective chart review of the infant and mother’s medical records at RCHSD/UCSD. Prospective telephone surveys ascertained prenatal care information from mothers of neonates who underwent or died prior to intervention within the first 31 days of life. All cardiac defects were included with the exception of infants with isolated ventricular septal defect (VSD), vascular ring, or branch pulmonary artery anomalies, who were excluded. CCHD diagnoses were categorized according to subtypes and the fetal cardiac view required for detection and whether the infant had a single ventricle or two ventricle lesion (Table 1). Diagnoses such as total anomalous pulmonary venous connection and atrioventricular canal defects are considered biventricular/four-chamber view (4CV) lesions that require the four-chamber view for diagnosis. Diagnoses such as hypoplastic left heart syndrome and tricuspid atresia are categorized as single ventricle lesions that require the four-chamber view for diagnosis. Tetralogy of Fallot and d-transposition of the great arteries are examples of proximal outflow tract diagnoses requiring outflow tract views. Interrupted aortic arch and coarctation of the aorta are diagnoses categorized as distal outflow tract anomalies requiring the three vessel view. Maternal demographic information and prenatal care factors, such as maternal age at delivery, maternal BMI, highest level of prenatal care, estimated gestational age at start of prenatal care, whether or not an anatomy scan was performed in the second trimester, maternal medical problems, insurance status and type of insurance, annual household income during pregnancy and delivery location were collected from the medical record and phone survey. Area Deprivation Index (ADI), a validated measure of neighborhood socioeconomic disadvantage, was assigned according to maternal zip code [16]. The study was approved by the RCHSD/UCSD Institutional Review Board.
Data Analysis
Continuous variable clinical demographic data was compared using the Wilcoxon Rank Sum Test. Categorical data was compared using Fisher’s exact tests. A p-value of less than 0.05 was used to define statistical significance. Univariable and multivariate regression analysis were performed to evaluate each predictor’s effect on the outcome of prenatal diagnosis. All statistical analyses were performed using R Core Team (2020. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. (https://www.R-project.org/). Analyses were performed for the entire study cohort and for those requiring intervention in the first 31 days of life.
Results
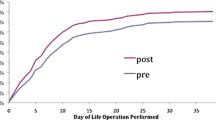
Overall, 58% (197/339) of infants with CCHD had prenatal diagnosis. The most common CCHD lesions were coarctation of the aorta (47% diagnosed prenatally), tetralogy of Fallot variants (63% diagnosed prenatally), and d-transposition of the great arteries (63% diagnosed prenatally) (Table 1). Infants with prenatal diagnosis were more likely to have mothers who were 35 or older (p = 0.028), had family history of CHD (p = 0.017), had health insurance (p = 0.002), or saw a perinatologist for their anatomic scan (p < 0.001) (Table 2). Hispanic infants were less likely to have prenatal diagnosis (57/125, 45.6%) compared to African American (19/26, 73%), Asian (21/33, 63.6%), or Caucasian/Non-Hispanic (77/121, 63.6%) infants (p = 0.005) (Fig. 1). Hispanic mothers were also more likely to have public health insurance (62%) compared to African American (48%), Asian (31%), or Caucasian/Non-Hispanic (18%) mothers (p < 0.001). In all infants who had prenatal diagnosis versus those who did not, there was no significant difference between maternal primary language, BMI, annual household income, socioeconomic status (based on ADI), health insurance type, or distance from a fetal cardiologist. Prenatal diagnosis rates were higher in infants with prenatal diagnosis of extracardiac/genetic anomalies (p < 0.001) and significantly different between subtypes of CCHD (76% in infants with single ventricle anomalies, 51% in infants with biventricular/4CV anomalies, 59% in infants with proximal outflow tract anomalies, and 48% in infants with anomalies of the distal great arteries; p = 0.024) (Table 3, Fig. 2).
Prenatal diagnosis rates based on type of congenital heart disease. The single ventricle group includes diagnoses such as hypoplastic left heart syndrome that require the four-chamber view for diagnosis. The two ventricle group includes biventricular/4CV lesions that require the four-chamber view for diagnosis such as total anomalous pulmonary venous return. Tetralogy of Fallot and D-Transposition of the Great Arteries are examples of diagnoses requiring outflow tract views. Interrupted aortic arch and coarctation of the aorta were diagnoses categorized as requiring the three vessel trachea view
In the infants without prenatal diagnosis, 73% should have been detected on screening cardiac views on anatomy ultrasound: 31/142 (21%) had CCHD detectable by fetal four-chamber view and 77/142 (54%) had CCHD detectable by adequate outflow tract imaging (Fig. 3). 25% (36/142) of mothers of infants without prenatal diagnosis had indication for, but were not referred for or did not undergo, fetal echocardiography; of these mothers, 47% (17/36) had diabetes (at least 6 with pre-gestational diabetes; 11 mothers had insufficient recall/data to determine type/severity of diabetes), 14% (5/36) were carrying monochorionic twin pregnancies, and 36% (13/36) had a fetus with an extracardiac (5 renal, 2 cleft lip/palate, 1 brain, 1 gastrointestinal) or genetic (Trisomy 21) anomaly, 2/36 had incomplete screening fetal cardiac views, and 1 had an IVF pregnancy.
Of the neonatal subgroup that required/underwent intervention within the first 31 days of life, 58% (124/215) were prenatally diagnosed. Within this subgroup, the statistical analysis yielded the same statistically significant factors as those in the whole study group with three exceptions. Mothers with public health insurance (p = 0.03) or a lower socioeconomic status as determined by the ADI (p = 0.028) were less likely to have an infant with prenatal diagnosis. Mother’s age at delivery did not reach statistical significance. Within the neonatal subgroup, infants of mothers who had prenatal care (p = 0.012), had insurance (p = 0.005), saw a perinatologist as the highest level of care (p < 0.001), had an anatomy scan done in the second trimester (p = 0.028), had a fetal echocardiogram (p < 0.001) were also more likely to be diagnosed prenatally.
In all infants who had prenatal diagnosis versus those who did not, there was no significant difference between maternal primary language, gestational age at start of prenatal care, presence of maternal medical problems, socioeconomic status, or miles from a fetal cardiologist.
In the univariate analysis (Table 4), Hispanic infants were less likely to be diagnosed prenatally (OR 0.48, p = 0.005 for the entire study population, OR 0.39, p = 0.004 for the neonatal subgroup). Mothers older than 35 years were more likely to have an infant with prenatal diagnosis (OR 1.83, p = 0.028). Although there was no statistically significant difference between insurance types when analyzing the entire study population, those with private insurance were more likely to be prenatally diagnosed in the neonatal intervention subgroup (OR 1.9, p = 0.04). Mothers with an obstetrician, midwife or family practice practitioner as their highest level of prenatal care were less likely to have an infant with prenatal diagnosis (OR 0.06, p < 0.001 for the entire study population; OR 0.03, p < 0.001 for the neonatal subgroup) compared to those who had a perinatologist as the highest level of care. Those with their anatomic scan at a perinatology office were more likely to be prenatally diagnosed as compared to those with their scan at an obstetric office (OR 3.35, p < 0.001 for the entire study population; OR 3.2, p = 0.003 for the neonatal subgroup).
Infants with single ventricle CHD were more likely to be prenatally diagnosed compared with biventricular/4CV CHD (OR 3.05, p = 0.02). In the neonatal intervention subgroup, those with single ventricle lesions (OR 8.55, p = 0.002), proximal outflow tract abnormalities (OR 5.2, p = 0.006), and distal outflow tract abnormalities (OR 4.76, p = 0.013) were more likely to be prenatally diagnosed as compared to biventricular/4CV lesions. Proximal outflow tract abnormalities included pulmonary stenosis, aortic stenosis, d-transposition of the great arteries, truncus arteriosus and tetralogy of Fallot. Distal outflow tract abnormalities included coarctation of the aorta and interrupted aortic arch. Those with extracardiac/genetic anomalies were more likely to be prenatally diagnosed for both the entire study population (OR 3.3, p < 0.001) and the neonatal subgroup (OR 2.7, p = 0.008).
The multivariate analysis (Table 5) included infant race/ethnicity, highest level of maternal prenatal care, location of anatomic scan, extracardiac/genetic abnormalities, views required for diagnosis, and single ventricular lesions versus biventricular/4CV lesions. Several variables were excluded from the multivariate analysis due to small subgroups. The multivariate analysis confirmed that Hispanic infants were less likely to be prenatally diagnosed (OR 0.42, p = 0.048). Those who had an obstetrician, midwife or family practice physician as their highest level of prenatal care were less likely to be prenatally diagnosed (OR 0.08, p < 0.001) compared to those who saw a perinatologist. Those who had their anatomic scan at a perinatology office were more likely to be prenatally diagnosed (OR 2.89, p = 0.01). The subtype of CCHD (single ventricle vs biventricular/4CV CCHD vs outflow tract anomalies vs distal great artery anomalies) and present of fetal extracardiac/genetic abnormality diagnosed were not statistically significant in the multivariate analysis.
Discussion
Overall, only 58% of infants with CCHD were diagnosed prenatally. This study found important demographic factors associated with a lower likelihood of prenatal diagnosis. Hispanic patients, those with lower socioeconomic status, and those without insurance were less likely to have prenatal diagnosis. Hispanic infants in our study were less likely to be prenatally diagnosed, with an odds ratio of 0.42 in a multivariate analysis after accounting for highest level of obstetrical care, location of anatomic scan, presence of extracardiac/genetic anomalies, and subtype of CHD. Although there was no statistically significant difference in level of prenatal care and lack of health insurance in Hispanic mothers, there may be other factors that are more difficult to define such as cultural differences that are not accounted for in our analysis. Infants who required neonatal intervention were less likely to be prenatally diagnosed if they had lower socioeconomic status. Socioeconomic status as measured by ADI was not statistically significant when analyzing the entire study population. We also found no statistically significant difference in household income between the prenatal versus postnatal diagnosis groups, but our dataset was limited by the retrospective nature of this study.
The findings in our study are consistent with multiple single and multicenter studies in the US and Canada linking lower socioeconomic status with decreased rates of prenatal diagnosis. A large multicenter Fetal Heart Society collaborative which demonstrated that Hispanic ethnicity, lower socioeconomic status, and rural residence were associated with decreased prenatal diagnosis in infants with TGA and lower socioeconomic status was associated with decreased prenatal diagnosis in infants with HLHS in the United States and Canada [17]. Another single center study in Wisconsin found that those living in impoverished or rural communities had lower rates of prenatal diagnosis.[18] A single center study in the United States found that patients with public health insurance and lower socioeconomic status were less likely to have prenatal diagnosis as compared to patients with private insurance and higher socioeconomic status [19]. A recent study from Alberta, Canada found that distance from a tertiary care center and lower socioeconomic status were associated with lower likelihood of prenatal diagnosis [20]. Even in places with universal health insurance, such as Canada, those of lower socioeconomic status were less likely to be prenatally diagnosed, suggesting that lower socioeconomic status has a role to play that is independent of insurance status. In our study, mothers without health insurance were less likely to have infants with prenatal diagnosis. Infants with CCHD who required neonatal intervention in our study were more likely to be prenatally diagnosed if they had private health insurance. However, we found no statistically significant different in type of insurance between those with or without prenatally diagnosis when analyzing the entire study population. A single center study at Northwestern University found that women with public health insurance were less likely to undergo diagnosis testing after positive screening for aneuploidy [21], suggesting that mothers without health insurance or with public health insurance may have additional challenges with understanding and navigating a complex multidisciplinary prenatal care system. Mothers without health insurance or with public health insurance may have limited resources to access advanced medical evaluation with a perinatologist and/or fetal echocardiography.
The overall 58% prenatal diagnosis rate of CCHD in San Diego County remains inadequate despite the 2013 societal guidelines intended to increase prenatal detection rates of CHD, with inclusion of views of the cardiac outflow tracts in addition to the four-chamber view of the fetal heart during routine obstetric anatomic ultrasounds [12]. The four-chamber view is the most standard and familiar fetal cardiac view to obstetric providers, and yet prenatal diagnosis rate of CCHD diagnosable by even this view remained a suboptimal 64% in this contemporary study. In CCHD requiring outflow tract imaging for diagnosis, the prenatal diagnosis rate was even lower at 59% in this study.
Worldwide prenatal diagnosis rates of CCHD are variable, with some regions in the world having prenatal diagnosis rates as high as 87% [22, 23]. Prior to 2013, a study analyzing the Society of Thoracic Surgeons database between 2006 and 2012 across 91 U.S. centers found a prenatal diagnosis rate of 34% for all CHD requiring surgical intervention at age less than or equal to six months; the detection rate was highest at 67% for hypoplastic left heart syndrome and lowest at 9% for total anomalous pulmonary venous return [5]. Similarly, a single center study in the United States found lower rates of prenatal diagnosis in CHD that required additional views other than four-chamber view, with a prenatal diagnosis rate of 48% for CHD diagnosable by 4 chamber view and 36% for CHD requiring outflow tract views [18]. A regional study in the Netherlands from 2002 to 2012 noted significantly higher prenatal detection rates (93%) in single ventricle lesions, with an overall CHD prenatal detection rate of 59% [24]. In Alberta, Canada between 2008 and 2018, 58% of major CHD was diagnosed prenatally with higher detection rates of 82% for lesions requiring the four-chamber view versus those 66% of those requiring the outflow tract view [25]. More recent studies done after the 2013 modified guidelines [12] in the United States and internationally have continued to show variable and wide ranges of prenatal diagnosis rates, with CHD diagnosable by the standard four-chamber view more often diagnosed prenatally (Table 6) [5, 22, 26, 27]. In San Diego between 2015 and 2016, prenatal detection rates of critical outflow tract anomalies was 61% [13]. In Japan between 2013 and 2017, 41% of infants with CCHD were diagnosed prenatally [28]. In Sweden between 2013 and 2017, 56% of infants with CCHD were diagnosed prenatally, with the prenatal detection rate for single ventricle lesions being 100% compared to 9% for TGA, an outflow tract anomaly [23]. In Copenhagen between 2015 and 2018, 89% of infants with CCHD were identified prenatally (although the study excluded those with pulmonary or aortic stenosis and total anomalous pulmonary venous return); 100% of single ventricle and HLHS infants had prenatal diagnosis compared to 82% of TGA infants [29].
In our study, a significant percentage (25%) of mothers of infants without prenatal diagnosis did not undergo fetal echocardiography although they had an indication for one. Common missed indications were maternal diabetes, fetal extracardiac defects or genetic anomaly, or a monochorionic twin pregnancy. Our study noted certain factors associated with increased likelihood of prenatal diagnosis, such as family history of congenital heart disease and presence of an extracardiac/genetic fetal anomaly, that are recommended indications for referral for a fetal echocardiogram [9]. We propose that increasing awareness in obstetrical providers of these maternal–fetal indications for referral for fetal echocardiography would increase rates of prenatal diagnosis. If a mother is appropriately referred for and undergoes fetal echocardiography, there is a very high likelihood of an accurate prenatal CHD diagnosis, as a comprehensive fetal echocardiogram has been previously shown to result in highly accurate diagnosis of CHD [14, 15]. Our study demonstrated a strong association between having a perinatologist as the highest level obstetrical provider and prenatal diagnosis of CHD. Several factors noted to be associated with a higher likelihood of prenatal diagnosis, such as advanced maternal age and extracardiac anomalies, would also be indications for referral to a perinatologist. Evaluation of fetal cardiac anatomy by perinatology is likely to be more comprehensive, with increased sonographer and physician expertise and comfort in detecting abnormality.
Limitations
This study is a single center study and findings may not be generalizable to larger populations. There is a significantly larger Hispanic population and smaller white, non-Hispanic population in San Diego County and our study population when compared to the United States as a whole [30]. Study data was obtained via retrospective chart review and cannot assess causality. Some data was obtained via telephone surveys of mothers of infants with CCHD and that data may be inaccurate due to recall bias, memory failure or other reasons. Telephone surveys for the entire study population were not obtained due lack of personnel time and resources; the survey was therefore limited to focus on those patients who required early intervention.
Due to the multiple referring obstetrical/perinatology practices outside of our institution’s accessible medical records and retrospective nature of the study, the study authors had limited data to certain aspect of prenatal care. This study did not include the total number of pregnancies diagnosed with CHD that terminated, as the information was not accurately attainable, and thus the true prenatal detection rate may be higher. Actual ultrasound images from the obstetric anatomic ultrasound scan were not available or acquired to review to determine whether the correct cardiac screening views were obtained and whether they were abnormal or normal. Reviewing obstetric ultrasound scan images in future studies may be helpful in addressing limitations in image technique and/or interpretation by providers obtaining anatomic ultrasound scans. Indications for referral to perinatology for anatomic scan (potentially resulting in increased detection of CHD) was not available. Despite these limitations, this study identified certain important factors strongly associated with lower likelihood of prenatal diagnosis that should be addressed in future outreach and policy making.
Conclusion
Prenatal diagnosis rates of CCHD remains inadequate, particularly across subtypes detectable by the standard fetal cardiac screening views. Certain maternal factors, such as lack of health insurance, suboptimal prenatal care, and Hispanic ethnicity, are associated with a lower likelihood of prenatal diagnosis and addressing these factors should be prioritized. Outreach to primary obstetrical providers and education regarding fetal cardiac imaging and indications for fetal echocardiogram, particularly in uninsured and Hispanic communities, should be prioritized to increase rates of prenatal diagnosis of CCHD. Additional multidisciplinary investments should aim to bring fetal echocardiography services to lower socioeconomic communities and reduce the gap in accessing higher levels of advanced prenatal care.
References
Hoffman JI, Kaplan S (2002) The incidence of congenital heart disease. J Am Coll Cardiol 39(12):1890–1900
Cloete E, Bloomfield FH, Sadler L et al (2019) Antenatal detection of treatable critical congenital heart disease is associated with lower morbidity and mortality. J Pediatr 204:66–70
Donofrio MT, Levy RJ, Schuette JJ et al (2013) Specialized delivery room planning for fetuses with critical congenital heart disease. Am J Cardiol 111(5):737–747
Allen JLM, Vernon M (2013) The financial impact of geography in pre- and postnatal detection of critical congenital heart disease in a broad referral area. J Am Coll Cardiol 61(10):E451
Quartermain MD, Pasquali SK, Hill KD et al (2015) Variation in prenatal diagnosis of congenital heart disease in infants. Pediatrics 136(2):e378–e385
Holland BJ, Myers JA, Woods CR Jr (2015) Prenatal diagnosis of critical congenital heart disease reduces risk of death from cardiovascular compromise prior to planned neonatal cardiac surgery: a meta-analysis. Ultrasound Obstet Gynecol 45(6):631–638
Chakraborty A, Gorla SR, Swaminathan S (2018) Impact of prenatal diagnosis of complex congenital heart disease on neonatal and infant morbidity and mortality. Prenat Diagn 38(12):958–963
Jegatheeswaran A, Oliveira C, Batsos C et al (2011) Costs of prenatal detection of congenital heart disease. Am J Cardiol 108(12):1808–1814
Donofrio MT, Moon-Grady AJ, Hornberger LK et al (2014) Diagnosis and treatment of fetal cardiac disease: a scientific statement from the American Heart Association. Circulation 129(21):2183–2242
Stumpflen I, Stumpflen A, Wimmer M et al (1996) Effect of detailed fetal echocardiography as part of routine prenatal ultrasonographic screening on detection of congenital heart disease. Lancet 348(9031):854–857
Simpson LL (2004) Indications for fetal echocardiography from a tertiary-care obstetric sonography practice. J Clin Ultrasound 32(3):123–128
AIUM practice guideline for the performance of obstetric ultrasound examinations. J Ultrasound Med. 2013;32(6):1083–101.
Sun HY, Proudfoot JA, McCandless RT (2018) Prenatal detection of critical cardiac outflow tract anomalies remains suboptimal despite revised obstetrical imaging guidelines. Congenit Heart Dis 13(5):748–756
Lytzen R, Vejlstrup N, Bjerre J et al (2020) The accuracy of prenatal diagnosis of major congenital heart disease is increasing. J Obstet Gynaecol 40(3):308–315
Haberer K, He R, McBrien A et al (2022) Accuracy of fetal echocardiography in defining anatomic details: a single-institution experience over a 12-year period. J Am Soc Echocardiogr 35(7):762–772
Hu J, Kind AJH, Nerenz D (2018) Area deprivation index predicts readmission risk at an urban teaching hospital. Am J Med Qual 33(5):493–501
Krishnan A, Jacobs MB, Morris SA et al (2021) Impact of socioeconomic status, race and ethnicity, and geography on prenatal detection of hypoplastic left heart syndrome and transposition of the great arteries. Circulation 143(21):2049–2060
Hill GD, Block JR, Tanem JB et al (2015) Disparities in the prenatal detection of critical congenital heart disease. Prenat Diagn 35(9):859–863
Peiris V, Singh TP, Tworetzky W et al (2009) Association of socioeconomic position and medical insurance with fetal diagnosis of critical congenital heart disease. Circ Cardiovasc Qual Outcomes 2(4):354–360
Kaur A, Hornberger LK, Fruitman D et al (2022) Impact of rural residence and low socioeconomic status on rate and timing of prenatal detection of major congenital heart disease in a jurisdiction of universal health coverage. Ultrasound Obstet Gynecol 60(3):359–366
Wong AE, Dungan J, Feinglass J et al (2015) Socioeconomic disparities in diagnostic testing after positive aneuploidy screening. Am J Perinatol 30(2):205–210
Bakker MK, Bergman JEH, Krikov S et al (2019) Prenatal diagnosis and prevalence of critical congenital heart defects: an international retrospective cohort study. BMJ Open 9(7):e028139
Waern M, Mellander M, Berg A et al (2021) Prenatal detection of congenital heart disease—results of a Swedish screening program 2013–2017. BMC Pregnancy Childbirth 21(1):579
van Velzen CL, Clur SA, Rijlaarsdam ME et al (2016) Prenatal detection of congenital heart disease–results of a national screening programme. BJOG 123(3):400–407
Kaur A, Hornberger LK, Fruitman D et al (2022) Trends in the prenatal detection of major congenital heart disease in Alberta from 2008 to 2018. J Obstet Gynaecol Can 44(8):895–900
Campbell MJ, Lorch S, Rychik J et al (2021) Socioeconomic barriers to prenatal diagnosis of critical congenital heart disease. Prenat Diagn 41(3):341–346
Evans WN, Acherman RJ, Ciccolo ML et al (2019) Detecting critical congenital heart disease in nevada. World J Pediatr Congenit Heart Surg 10(6):702–706
Matsui H, Hirata Y, Inuzuka R et al (2021) Initial national investigation of the prenatal diagnosis of congenital heart malformations in Japan-Regional Detection Rate and Emergency Transfer from 2013 to 2017. J Cardiol 78(6):480–486
Vedel C, Tabor A, Jorgensen FS et al (2021) Prenatal detection rate of major congenital heart defects in Copenhagen from 2015 to 2018. Ultrasound Obstet Gynecol 58(2):324–325
U.S. Census Bureau QuickFacts: United States; San Diego City, California. https://wwwcensusgov/quickfacts/fact/table/sandiegocountycalifornia,US/PST045221. Accessed March 6, 2023.
Evans WN, Acherman RJ, Restrepo H (2021) Prenatal diagnosis of significant congenital heart disease and elective termination of pregnancy in Nevada. J Matern Fetal Neonatal Med 35:8761
Acknowledgements
The authors would like to thank Hyeri You and Lin Liu for their assistance with the statistical analysis and Xiaoyang Yu for assistance with data collection. The project described was partially supported by the National Institutes of Health, Grant UL1TR001442 of CTSA funding. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Author information
Authors and Affiliations
Contributions
HYS, AD, IFG and HO contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no disclosures.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Davtyan, A., Ostler, H., Golding, I.F. et al. Prenatal Diagnosis Rate of Critical Congenital Heart Disease Remains Inadequate with Significant Racial/Ethnic and Socioeconomic Disparities and Technical Barriers. Pediatr Cardiol (2023). https://doi.org/10.1007/s00246-023-03262-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00246-023-03262-2