Abstract
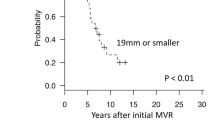
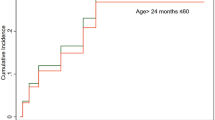
Evolving reconstructive techniques have progressively become the preferred approach for treatment of pediatric mitral valve regurgitation. We present our experience in a cohort of patients undergoing surgical correction for severe mitral regurgitation. Fifty-five patients (age 1 month–18 years; median 5 years) were included in the present analysis. Different surgical techniques were used (posterior leaflet augmentation in 25, isolated cleft closure in 12, Alfieri-type procedure in 10, annuloplasty in 5, with artificial chordae in 2, and quadrangular resection with chordal transposition in 1). Follow-up time ranged from 1 to 192 months (median 38[IQR 12–54] months). Operative and follow-up mortality was 0%. Reintervention in the whole population occurred in 31% of patients. However, when first surgery was performed under 2 years of age (no = 17), reintervention reached nearly 50%. The degree of residual mitral regurgitation at follow-up remained stable after surgery, while a significant increase in mean transmitral gradient was observed over time (paired t test = 0.03). In multivariable Cox-regression analysis, post-surgical transmitral gradient was the only independent predictor for reintervention (p = 0.017; HR 2.4; 95%CI 1.2–5.1), after correcting for differences in age at surgery, type of reintervention, mitral annulus dimension, and BSA at the first surgery. ROC curve demonstrated that a post-surgical transmitral mean gradient value > 5 mmHg, was predictive for reintervention (AUC = 0.89; Youden index = 0.44). Our study suggests that the use of conservative technique strategy achieves satisfactory functional results in infants and children with severe MR, although the rate of reoperation in younger patients remains substantial. Post-operative moderate mitral stenosis was the strongest predictor for reoperation.




Similar content being viewed by others
Abbreviations
- PLA:
-
Posterior leaflet augmentation
- OST:
-
Other surgical techniques
- MV:
-
Mitral valve
- MR:
-
Mitral regurgitation
- ePTFE:
-
Expanded polytetrafluoroethylene
- BSA:
-
Body surface area
References
Carpentier A, Branchini B, Cour JC, Asfaou E, Villani M, Deloche A, Relland J, DAllaines C, Blondeau P, Piwnica A, Parenzan L, Brom G (1976) Congenital malformations of the mitral valve in children. Pathology and surgical treatment. J Thorac Cardiovasc Surg 72(6):854–866
Chauvaud S, Fuzellier JF, Houel R, Berrebi A, Mihaileanu S, Carpentier A (1998) Reconstructive surgery in congenital mitral valve insufficiency (Carpentier’s techniques): long-term results. J Thorac Cardiovasc Surg 115(1):84–93
Caldarone CA, Raghuveer G, Hills CB, Atkins DL, Burns TL, Behrendt DM, Moller JH (2001) Long-term survival after mitral valve replacement in children < 5 years: a multi-institutional study. Circulation 104(12 Suppl 1):I143-7
Baird CW, Myers PO, Marx G, Del Nido PJ (2012) Mitral valve operations at a high volume pediatric heart center: evolving techniques and improved survival with mitral valve repair versus replacement. Ann Pediatr Cardiol 5(1):13–20
Oppido G, Davies B, McMullan DM, Cochrane AD, Cheung MMH, d’Udekem Y, Brizard CP (2008) Surgical treatment of congenital mitral valve disease: midterm results of a repair-oriented policy. J Thorac Cardiovasc Surg 135(6):1313–1321
Kalfa D, Vergnat M, Ly M, Stos B, Lambert V, Baruteau A, Belli E (2014) A standardized repair-oriented strategy for mitral insufficiency in infants and children: midterm functional outcomes and predictors of adverse events. J Thorac Cardiovasc Surg 148(4):1459–1466
Chauvaud S, Jebara V, Chachques JC, el Asmar B, Mihaileanu S, Perier P et al (1991) Valve extension with glutaraldehyde-preserved autologous pericardium. Results in mitral valve repair. J Thorac Cardiovasc Surg 102:171–178
Dion RA, Gutermann H, Van Kerrebroeck C, Verhaert D (2012) Augmentation of the posterior leaflet of the mitral valve. Multimed Man Cardiothorac Surg 2012:mms015. https://doi.org/10.1093/mmcts/mms015
Trezzi M, Cetrano E, Albano A, Carotti A (2015) Extending the limits for mitral valve replacement in low-weight infants using a stented bovine jugular vein graft. J Thorac Cardiovasc Surg 150(3):729–730
Uva MS, Galletti L, Gayet FL, Piot D, Serraf A, Bruniaux J et al (1995) Surgery for congenital mitral valve disease in the first year of life. J Thorac Cardiovasc Surg 109(1):164–176
Stellin G, Padalino MA, Vida VL, Bozzucco G, Orrù E, Biffanti R et al (2010) Surgical repair of congenital mitral valve malformations in infancy and childhood: a single-center 36-year experience. J Thorac Cardiovasc Surg 140(6):1238–1244
Wood AE, Healy DG, Nolke L, Duff D, Oslizlok P, Walsh K (2005) Mitral valve reconstruction in a pediatric population: late clinical results and predictors of long-term outcome. J Thorac Cardiovasc Surg 130(1):66–73
Aharon AS, Laks H, Drinkwater DC, Chugh R, Gates RN, Grant PW et al (1994) Early and late results of mitral valve repair in children. J Thorac Cardiovasc Surg 107(5):1262–1270
Krishnan US, Gersony WM, Berman-Rosenzweig E, Apfel HD (1997) Late left ventricular function after surgery for children with chronic symptomatic mitral regurgitation. Circulation 96:4280–4285
Murakami T, Nakazawa M, Nakanishi T, Momma K (1999) Prediction of postoperative left ventricular pump function in congenital mitral regurgitation. Pediatr Cardiol 20:418–421
Minami K, Kado H, Sai S, Tatewaki H, Shiokawa Y, Nakashima A, Fukae K, Hirose H (2005) Midterm results of mitral valve repair with artificial chordae in children. J Thorac Cardiovasc Surg 129(2):336–342
Boon R, Hazekamp M, Hoohenkerk G, Rijlaarsdam M, Schoof P, Koolbergen D, Heredia L, Dion R (2007) Artificial chordae for pediatric mitral and tricuspid valve repair. Eur J Cardiothorac Surg 32(1):143–148. Epub 2007 May 2
Alghamdi AA, Yanagawa B, Singh S, Horton A, Al-Radi OO, Caldarone CA (2011) Balancing stenosis and regurgitation during valve surgery in pediatric patients. Ann Thorac Surg 92:680–684
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brancaccio, G., Chinali, M., Trezzi, M. et al. Outcome for Conservative Surgery for the Correction of Severe Mitral Valve Regurgitation in Children: A Single-Center Experience. Pediatr Cardiol 40, 1663–1669 (2019). https://doi.org/10.1007/s00246-019-02201-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-019-02201-4