Abstract
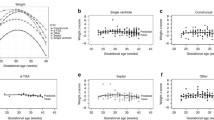
We evaluated differences in growth between fetuses with and without congenital heart disease (CHD) and tested associations between growth and early childhood neurodevelopment (ND). In this prospective cohort study, fetuses with hypoplastic left heart syndrome (HLHS), transposition of the great arteries (TGA), and tetralogy of Fallot (TOF) and controls had biparietal diameter (BPD), head (HC) and abdominal circumference (AC), femur length (FL), and estimated fetal weight (EFW) recorded serially during pregnancy at 18–26 weeks GA (F1), at 27–33 weeks GA (F2), and at 34–40 weeks GA (F3). CHD subjects underwent Bayley Scales of Infant Development-III ND testing at 18 months. Differences between CHD fetuses and controls were assessed using t tests and generalized linear modeling. Correlations between biometry and ND informed regression modeling. We enrolled 41 controls and 68 fetuses with CHD (N = 24 HLHS, N = 21 TGA, N = 23 TOF), 46 of whom had ND scores available. At 18–26 weeks, CHD fetuses were smaller than controls in all biometric parameters. Differences in growth rates were observed for HC, BPD, and AC, but not for FL or EFW. Cognitive score correlated with HC/AC at F2 (r = −0.33, P = 0.04) and mean HC/AC across gestation (r = −0.35, P = 0.03). Language correlated with FL/BPD at F2 (r = 0.34, P = 0.04). In stepwise linear regression, mean HC/AC predicted Cognition (B = −102, P = 0.026, R 2 = 0.13) and FL/BPD at F2 predicted Language score (B = 127, P = 0.03, R 2 = 0.12). Differences in growth between CHD fetuses and controls can be measured early in pregnancy. In CHD fetuses, larger abdominal relative to head circumference is associated with better 18-month neurodevelopment.


Similar content being viewed by others
References
De Onis M (2006) WHO Multicenter Growth Reference Study Group. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr 450(Suppl):76–85
Donofrio MT, Bremer YA, Schieken RM, Gennings C, Morton LD, Eidem BW, Cetta F, Falkensammer CB, Huhta JC, Kleinman CS (2003) Autoregulation of cerebral blood flow in fetuses with congenital heart disease: the brain sparing effect. Pediatr Cardiol 24(5):436–443
Dudley NJ (2005) A systematic review of the ultrasound estimation of fetal weight. Ultrasound Obstet Gynecol 25(1):80–89
Duncan KR, Issa B, Moore R, Baker PN, Johnson IR, Gowland PA (2005) A comparison of fetal organ measurements by echo-planar magnetic resonance imaging and ultrasound. BJOG 112(1):43–49
Hadlock FP, Deter RL, Harrist RB, Park SK (1984) Estimating fetal age: computer-assisted analysis of multiple fetal growth parameters. Radiology 152:497–5011
Hadlock FP, Harrist RB, Sharman RS, Deter RL, Park SK (1985) Estimation of fetal weight with the use of head, body, and femur measurements—a prospective study. Am J Obstet Gynecol 151(3):333–337
Khalil A, Suff N, Thilaganathan B, Hurrell A, Cooper D, Carvalho JS (2014) Brain abnormalities and neurodevelopmental delay in congenital heart disease: systematic review and meta-analysis. Ultrasound Obstet Gynecol 43(1):14–24
Khoury MJ, Erickson JD, Cordero JF, McCarthy BJ (1988) Congenital malformations and intrauterine growth retardation: a population study. Pediatrics 82(1):83–90
Levy RJ, Rosenthal A, Fyler DC, Nadas AS (1978) Birthweight of infants with congenital heart disease. Am J Dis Child 132(3):249–254
Limperopoulos C, Tworetzky W, McElhinney DB, Newburger JW, Brown DW, Robertson RL Jr, Guizard N, McGrath E, Geva J, Annese D, Dunbar-Masterson C, Trainor B, Laussen PC, du Plessis AJ (2010) Brain volume and metabolism in fetuses with congenital heart disease: evaluation with quantitative magnetic resonance imaging and spectroscopy. Circulation 121(1):26–33
Masoller N, Martínez JM, Gómez O, Bennasar M, Crispi F, Sanz M, Egaña-Ugrinovic G, Bartrons J, Puerto B, Gratacós E (2014) Evidence of second trimester changes in head biometry and brain perfusion in fetuses with congenital heart disease. Ultrasound Obstet Gynecol 44(2):182–187
Matos SM, Sarmento S, Moreira S, Pereira MM, Quintas J, Peixoto B, Areias JC, Areias ME (2014) Impact of fetal development on neurocognitive performance of adolescents with cyanotic and acyanotic congenital heart disease. Congenit Heart Dis 9(5):373–381
Newburger JW, Sleeper LA, Bellinger DC, Goldberg CS, Tabbutt S, Lu M, Mussatto KA, Williams IA, Gustafson KE, Mital S, Pike N, Sood E, Mahle WT, Cooper DS, Dunbar-Masterson C, Krawczeski CD, Lewis A, Menon SC, Pemberton VL, Ravishankar C, Atz TW, Ohye RG, Gaynor JW (2012) Pediatric Heart Network Investigators. Early developmental outcome in children with hypoplastic left heart syndrome and related anomalies: the single ventricle reconstruction trial. Circulation 125(17):2081–2091
Owen M, Shevell M, Donofrio M, Majnemer A, McCarter R, Vezina G, Bouyssi-Kobar M, Evangelou I, Freeman D, Weisenfeld N, Limperopoulos C (2014) Brain volume and neurobehavior in newborns with complex congenital heart defects. J Pediatr 164(5):1121–1127
Ravishankar C, Zak V, Williams IA, Bellinger DC, Gaynor JW, Ghanayem NS, Krawczeski CD, Licht DJ, Mahony L, Newburger JW, Pemberton VL, Williams RV, Sananes R, Cook AL, Atz T, Khaikin S, Hsu DT (2013) Pediatric Heart Network Investigators. Association of impaired linear growth and worse neurodevelopmental outcome in infants with single ventricle physiology: a report from the pediatric heart network infant single ventricle trial. J Pediatr 162(2):250–256
van Batenburg-Eddes T, de Groot L, Steegers EA, Hofman A, Jaddoe VW, Verhulst FC, Tiemeier H (2010) Fetal programming of infant neuromotor development: the generation R study. Pediatr Res 67(2):132–137
Williams IA, Tarullo AR, Grieve PG, Wilpers A, Vignola EF, Myers MM, Fifer WP (2012) Fetal cerebrovascular resistance and neonatal EEG predict 18-month neurodevelopmental outcome in infants with congenital heart disease. Ultrasound Obstet Gynecol 40(3):304–309
Williams IA, Fifer C, Jaeggi E, Levine JC, Michelfelder EC, Szwast AL (2013) The association of fetal cerebrovascular resistance with early neurodevelopment in single ventricle congenital heart disease. Am Heart J 165(4):544–550
Acknowledgments
I.A. Williams received support from Grant No. 1K23HD061601 from the National Institute of Child Health & Human Development of the National Institutes of Health and from the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant Number UL1 TR000040. The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Child Health & Human Development.
Conflict of interest
The authors declare that they have no conflicts of interest or relationships to disclose beyond those listed above.
Ethical standard
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Williams, I.A., Fifer, W.P. & Andrews, H. Fetal Growth and Neurodevelopmental Outcome in Congenital Heart Disease. Pediatr Cardiol 36, 1135–1144 (2015). https://doi.org/10.1007/s00246-015-1132-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-015-1132-6