Abstract
Background
Surgical complications following breast reconstruction remain a significant concern. This study aimed to investigate if incisional negative pressure wound therapy (iNPWT) using Prevena™ provides superior wound treatment for patients undergoing immediate breast reconstruction (IBR) compared to conventional postoperative dressing. Additionally, we investigated whether intraoperative indocyanine green angiography (ICG-A) could predict and prevent postoperative complications.
Methods
A randomized controlled study (RCT) comprising 39 patients was conducted. The primary outcome was time until surgical drain removal. ICG-A was applied to evaluate tissue perfusion and compared to rate of postoperative complications. Patients were followed for one year, including postoperative complications, quality of life (QoL), scar evaluation, incidence of lymphedema and timely administration of adjuvant therapy.
Results
No significant differences were observed in time to surgical drain removal, hospitalization or incidence of postoperative complications between the two groups. Analysis revealed no significant association between ICG-A results and postoperative complications. After one year, both groups exhibited similar QoL and satisfaction with scars. One patient developed lymphedema during follow-up, and adjuvant treatment was timely administered in 82%.
Conclusions
This RCT investigated iNPWT by Prevena™ compared to conventional postoperative dressing in IBR using implants or tissue expanders. ICG-A was applied to assess tissue perfusion and compared to postoperative complications. We did not find any significant differences in recovery time, hospitalization duration, postoperative complication rates, QoL, or scar satisfaction between the two groups within a one-year follow-up. Additionally, there were no significant association between ICG-A and postoperative complications. Larger randomized studies incorporating intraoperative ICG-A are needed to obtain higher quality data.
Level of Evidence: Level I, Risk/Prognostic
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Breast cancer is the leading cancer in women worldwide affecting 1 in every 9 women [1, 2].
Though many patients are treated by breast conserving therapy [3], some patients will require mastectomy possibly combined with a breast reconstruction which may be performed as an immediate procedure [4].
Implant-based immediate breast reconstruction (IBR) requires a healthy well-vascularized flap accomplished by careful planning and close collaboration with breast surgeons. However, the overall risk of complications can be as high as 60% [4,5,6] with rates of surgical site infections and flap necrosis of 20–30% [7].
Prevention of surgical site complications in oncological patients is crucial, not only to avoid a negative effect on patients’ quality of life (QoL), but also risk of postponing adjuvant treatment.
affecting both recurrence risk and overall survival—constituting a significant burden for society [8,9,10].
Negative pressure wound therapy (NPWT), known as vacuum assisted closure (VAC), has been widely used treating different types of wounds by generating negative pressure leading to removal of excess fluid, reduction of edema, increased dermal perfusion, stimulating the formation of granulation tissue and reducing bacterial colonization [10]. Studies have reported NPWT to be associated with a reduced risk of complications, improved scar quality and enhanced recovery [11,12,13]. In breast surgery, use of NPWT is reported to lower the risk of infections, wound dehiscence, necrosis and seroma and cost-efficient [8,9,10, 14, 15].
Incisional negative pressure wound therapy (iNPWT), is a newer approach for surgical site closure based on the principles behind NPWT. Recently, Prevena™ has been approved as an iNPWT-system applied at completion of the breast reconstructive procedure.
Prevena™ consists of a sponge foam with a bactericidal silver linning, dressed with an adherent film, connected to a vacuum device [16]. The Prevena™ foam and dressing is placed over the suture line and kept in situ for 7 days (https://www.3m.com/3M/en_US/p/d/b5005265118/).
Indocyanine green angiography (ICG-A) is an intraoperative imaging modality developed to assist in quantification of tissue perfusion and perforators in breast reconstructive procedures. Use of ICG-A is associated with a lower risk of per- and postoperative complications within breast reconstructive procedures [17,18,19,20].
We hypothesize that iNPWT, administrated by Prevena™ can potentially reduce the postoperative complications in patients undergoing IBR, compared to conventional postoperative dressing (3 M™ Micropore™ tape).
Furthermore, that intraoperative results of ICG-A are associated with mastectomy skin flap necrosis and postoperative outcomes.
The aim of this study is to evaluate whether iNPWT provides superior wound treatment for patients undergoing an IBR, compared to treatment with conventional postoperative dressing. Furthermore, to investigate if intraoperative use of ICG-A can predict and prevent postoperative complications.
Secondly, to evaluate scars, QoL, timing of adjuvant therapy and incidence of postoperative lymphedema of the affected limb/limbs after IBR.
Accordingly, we conducted a randomized controlled study (RCT) applying iNPWT in IBR using implants or tissue expanders (TE). Intraoperative ICG-A was applied in all procedures.
We present this paper in accordance with the CONsolidated Standards Of Reporting Trials (Consort) guidelines.
Methods
Patients
Forty-one patients undergoing IBR using implants or TE were included.
Patients were enrolled consecutively at the Department of Plastic Surgery and Burns Treatment, Copenhagen University hospital, Rigshospitalet, Denmark between February and December 2020.
The inclusion criteria were: Patients older than 18 years of age deemed suitable for IBR by the consultant plastic- and breast surgeon. Patients who were pregnant, breastfeeding or not able to understand enough Danish to comprehend the given information and to complete the study questionnaires were excluded. Patients allergic to iodine were also excluded [21].
Data collection
Authors adhered to the Consort guidelines. The study was approved by The Capital Denmark Region Committees on Health Research Ethics (H-19074545, 70,429).
Ethical considerations.
The study was approved and registered by the Capital Region of Denmark joint application for the Danish Data Protection Agency, the Scientific Ethical Committee of the Capital Region of Denmark, and the research project was carried out in accordance with the Helsinki Declaration II.
Randomization
The included patients were randomized to one of two arms: Prevena™ iNPWT treatment for 7 days (intervention group) or conventional postoperative dressing (control group), in an allocation ratio of 1:1, using a block randomization according to the SNOSE principles [22]. Regardless of which type of post-operative dressing the patient was randomized to receive, the surgical procedure was performed in the same way (standard of care). The study was not blinded, since the Prevena™ device makes a sound, when generating negative pressure, and the dressing looks a lot different compared to the conventional post-operative dressing.
Intraoperative ICG-A application and perfusion assessment
Twenty-five milligrams of ICG were diluted in 10 mL sterile water, an intravenous bolus administration of ICG (Verdye® 5 mg/mL, Diagnostic Green GmbH Feldkirchener Str. 7c 85,551 Kirchheim b. Munich, Germany) of 2.5 mg/mL is followed by a 10 mL flush with normal saline (2.5 mL of ICG solution for each administration)[23].
Peroperative tissue perfusion is visualized within 20 s using the SPY-Elite Fluorescence Imaging system® (Stryker AB, Malmö, Sweden, www.stryker.com) (Video 1). Perfusion was scored and quantified 45 s after injection, and recording concluded after 60 s [24]. The relative perfusion values were quantified using a cut-off value of 33% [25]. Each ICG injection was performed with a minimum of 20 min, and the same investigator conducted the angiographies and quantification of perfusion [26]. Tissue perfusion was consecutively assessed by the ICG-A and compared to the surgeons’ clinical assessment (capillary refill and bleeding from skin edges).
After mastectomy, skin flaps were assessed clinically to identify areas in risk of hypoperfusion. A sizer of appropriate size was inserted, and the dermis temporarily sutured. The first ICG-A was then performed assessing mastectomy skin flaps, with healthy skin outside the surgical field (usually the skin covering the area over the xiphoied process) serving as reference point (100%).
If the angiography was sufficient, breast reconstruction proceeded with either a prepectoral implant wrapped in acellular matrix (Tutomesh®), or a subpectoral (i.e., dual plane) implant/TE with similar matrix.
If the angiography showed values < 33%, the procedure was re-evaluated clinical assessment and a repeated ICG-A. Perfusion < 33% on the second angiography resulted in excision of the hypoperfused area (if located near incision area), a smaller implant or reconstruction with subpectoral placement of a TE. Upon completing the breast reconstruction, ICG-A was performed again to confirm and ensure sufficient perfusion. Two drains were used for each patient, and removed when producing less than 30 ml. for 2 consecutive days.
Complications
Complications were reported and analyzed both per patient and per breast including minor- and major complications, as well as loss of reconstruction.
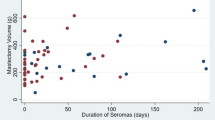
Major complications were defined as complications requiring surgery/debridement in local- or general anesthesia. Minor complications were defined as complications treated conservatively: seroma, infections treated by antibiotics, small hematoma etc. Loss of reconstruction was defined as implant removal without replacement with TE.
Follow-up and postoperative clinical evaluation
Clinical evaluations were conducted 4 times during the trial: before surgery and at 4 weeks, 4–6 months, and 12 months postoperatively. Outpatient visits included assessment of patient well-being and a clinical examination, involving inspecting the surgical fields for signs of infection, necrosis, seroma, hematoma etc. Scars were assessed using the POSAS, and BREAST-Q questionnaires to evaluate QoL. Lymphedema measurements were also performed.
Patient reported satisfaction and aesthetic outcome (BREAST-Q)
Before surgery (at baseline), patients completed the Danish version of the BREAST-Q 1.0 pre-reconstruction module. At each clinical follow-up, the post-reconstruction module of BREAST-Q 1.0 was used to assess patients' QoL using the BREAST-Q score [27].
Patient and Observer Scar Assessment Score (POSAS 2.0)
Scars were assessed using the POSAS (Patient and Observer Scar Assessment Scale) at each post-operative clinical visit [28].
Assessment of postoperative lymphedema
To assess the incidence of postoperative lymphedema measurements of the affected limb/limbs were performed before surgery (baseline) and at each postoperative visit [29]. A specialized physiotherapist performed circumferential measurements (figure-of-eight), and bioimpedance spectroscopy (BIS) using the SOZO system (https://www.impedimed.com/products/sozo/). Presence of lymphedema was categorized based on the International Society of Lymphology staging system [30].
Endpoints
Our primary endpoint was the postoperative time to removal of the surgical drains, as we hypothesize that Prevena™ leads to faster and better regeneration, with fewer complications, thus leading to lover formation of seroma and thereby shorter drain time. Drains were removed when producing less than 30 ml. for 2 consecutive days.
Secondly, proportion of flaps where the ICG-A assessment showed sufficient/insufficient perfusion, and proportion where the intraoperative results of the ICG-A changed surgical decision making. Furthermore, analysis of the association between intraoperative ICG-A and postoperative complications: infection, hematoma, necrosis, epidermolysis and partial- or full flap loss was evaluated [31]. Development of lymphedema, changes in QoL and differences in POSAS were all considered as secondary endpoints, as well as timely initiation of adjuvant treatment. Timely initiation was defined as the date set by the oncologists at the first postoperative multidisciplinary conference.
Statistical analysis
Statistical analysis was performed using R for Mac OS X GUI R 4.2.2 GUI 1.79 High Sierra build (8160). R: Copyright © 2004–2021. The R Foundation for Statistical Computing. http://www.R-project.org.
Continuous variables were analyzed using Wilcox-signed rank test assuming non-distributed data.
Categorical variables were analyzed using Fisher’s exact test due to small sample size.
Analysis of the POSAS were made using Wilcox-signed rank test assuming non-distributed data.
The BREAST-Q was analyzed comparing pre- and postoperative scores within and between the patients allocated to either Prevena™ or conventional postoperative dressing. Two-way repeated measures ANOVA tests were used to analyze repetitive measurements comparing the 2 patient groups based on the assumption of normative data [24]. Statistical significance was set by p-values < 0.05.
The minimal clinically relevant difference the study was looking for, was a decrease of 3 days from surgery until removal of drains. The standard deviation for days until drain removal after immediate breast reconstruction was found by Kim et al. to be 3.66 days [26].
To achieve a statistical significance level of 5% and a study power of 80%, a minimum of 24 patients were required in each group. To raise the power to 88%, we planned to include 30 patients in each group.
Results
Of 41 included patients, 2 dropped out leaving 39 patients for inclusion. Twenty-two patients received unilateral procedures and 17 bilateral, comprising a total of 56 breasts with 30 breasts receiving Prevena™ and 26 standard dressing. Of the 39 patients, 25 received a prepectoral implant-based IBR and 14 were subpectoral.
Mean age was 46.1 years (range 31–65) and mean body mass index (BMI) 23.3 kg/m2 (range 18.7–32.5). Baseline demographics are depicted in Table 1.
Patients were randomly allocated according to the randomization protocol, with 21 patients (30 breasts) in the Prevena™ group and 18 patients (26 breasts) treated with conventional post-operative dressing (Fig. 1).
Statistical analysis on smoking status, alcohol consumption, indication for surgery and adjuvant treatment showed no difference in baseline characteristics between the 2 groups. Furthermore, there were no significant difference in baseline characteristics or complication rates between patients receiving a pre- or subpectoral IBR.
Time to removal of the surgical drains: Prevena™ or conventional dressing
Mean time from breast reconstruction to removal of surgical drains was 10.2 days in the Prevena™ group and 9.3 days in the group treated with conventional postoperative dressing. Analysis showed no significant difference (p = 0.30, W = 202) Table 2.
Hospitalization: Prevena™ or conventional dressing
Mean hospitalization time did not differ in the groups (p = 0.28, W = 151) Table 2. Patients receiving conventional postoperative dressing had a mean hospitalization time of 4.9 days and 4.3 days in the Prevena™ group.
Postoperative dressing and complications: Prevena™ or conventional dressing
Complications including epidermolysis, necrosis, infection, seroma and hematoma were analyzed both per breast and per patient according to the randomization arm: Prevena™ or conventional dressing Tables 2 and 3. Also, complications were grouped in minor, major and loss of reconstruction according to postoperative dressing. Analysis showed no significant differences in incidence of postoperative complications Tables 2 and 3.
Peroperative ICG-A results and postoperative complications
Intraoperative ICG-A found sufficient perfusion in 30/39 patients (77%) Table 4.
Overall, 9/30 patients (23%) demonstrated insufficient perfusion by the ICG-A, whereof 8 of the 9 (88.9%) affected/influenced the intraoperative surgical decision making. Of these 8 patients, 7 (87.5%) experienced postoperative complications consisting of 4 minor complications, 3 major complications and 1 loss of reconstruction. In total, 33.3% with insufficient ICG-A developed major complications.
In 1 patient where the ICG-A showed insufficient perfusion, the surgeons chose to wait and see. This patient healed without complications.
Of the 30 patients where the ICG-A assessed the perfusion to be sufficient, 12 (40%) developed postoperative complications. Of these 12, 10 had minor complications, 2 major complications and 1 loss of reconstruction. Of the patients with sufficient perfusion on the ICG-A 6.67% developed major complications.
Analysis showed no significant association between ICG-A-result and incidence of overall postoperative complications. Also, there were no significant association between ICG-A result and major complications Table 5.
Postoperative follow-up, BREAST-Q and POSAS
BREAST-Q was completed by > 95% at each follow-up Table 1.
Analysis of the BREAST-Q showed a significant improvement in psychosocial- (p = 0.023) and physical well-being (p < 0.001) from the 4-weeks to 12 months follow-up Table 6.
Analyzing the 2 treatment groups, patients receiving the conventional postoperative dressing showed significant better physical- (p = 0.023) and sexual well-being (p = 0.017) after 12 months compared to the Prevena™ group. The were no significant difference between the 2 groups in satisfaction with outcome Table 6.
The POSAS 4-weeks assessment were completed > 85% at each follow-up Table 1.
For both groups, there were no significant difference between the patients’ and observers’ scars scoring after 12 months Table 6, Fig. 2 + 3.
Assessment of postoperative lymphedema and administration of adjuvant therapy
Four patients had preoperatively been diagnosed with lymphedema of the upper extremity Table 1. All 4 had previously undergone axillary lymph node dissection (ALND) and underwent a delayed breast reconstructive procedure. One had been treated with neo-adjuvant chemotherapy (NACT), 2 had undergone adjuvant chemo- and radiation therapy (RT) and 1 had NACT and adjuvant RT.
After 12 months follow-up, 1 additional patient presented with lymphedema of the upper extremity. She had undergone immediate breast reconstruction and ALND in the same procedure and received NACT and adjuvant RT Table 1.
Adjuvant treatment was administered on time in 32 patients (82%). Two patients (5%) experienced delayed adjuvant treatment due to surgical complications, delaying treatment in 7 and 10 days, respectively. Five patients (13%) had their adjuvant treatment delayed due to non-surgical reasons Table 1.
Due to few patients, we did not investigate associations between surgical treatment and lymphoedema. Nor between delayed adjuvant treatment and postoperative complications in relation to postoperative dressings.
Discussion
This single-center RCT investigated if iNPWT administrated by Prevena™ leads to faster recovery and reduces the rate of postoperative complications in patients undergoing IBR. Patients were randomized to receive either Prevena™ or conventional postoperative dressing (3 M™ Micropore™ tape) on the closed incisions.
Time to removal of surgical drains was set as an indicator for faster recovery. Also, we investigated if the use Prevena™ was associated with an increased QoL and satisfaction with scars.
Secondly, intraoperative ICG-A was applied in all procedures analyzing association between ICG-A results and rate of postoperative complications.
Patients were followed for 1 year, including a clinical evaluation before the breast reconstructive procedure and 3 clinical evaluations postoperatively.
Use of iNPWT for closed incisions have been described by several authors, and there is growing evidence that it is associated with reduced complication rates following surgery [8, 10, 11, 15].
A multicenter RCT by Pieszko et al. demonstrated a significant decrease in surgical-site wound complications in patients treated with iNPWT for closed incisions in IBR [14]. iNPWT has also been useful for reduction of complications in mammoplasties and prepectoral breast reconstruction [28, 32], but inconclusive in oncoplastic breast surgery [29, 33].
This study did not find any significant association between the use of iNPWT by Prevena™ and reduced time to removal of drains. Also, there were no significant difference in mean hospitalization time. The rate of postoperative complications was analyzed both per breast and per patient, with no significant differences between the 2 groups in both minor- and major complications, and loss of reconstruction.
The insignificant results may be caused by a substantial lower sample size (39 patients were included) than anticipated when planning the study (a total of 60 patients, with 30 in each group).
Of the total patient population, 48.7% developed postoperative complications with major complications constituting 12.8% and 5.1% experiencing loss of reconstruction. These rates are comparable to previous published studies [14, 34, 35].
Intraoperative change according to the ICG-A was performed in 88.9% with insufficient ICG-A, yet the majority (87.5%) experienced postoperative complications with 33.3% being major complications.
Of the cases with sufficient perfusion by the ICG-A, 40% experienced postoperative complications and 6.7% of these were major complications.
Previous studies have demonstrated ICG-A to be associated with a reduced risk of postoperative complications in breast reconstructive procedures [17, 18, 20, 25, 36,37,38,39,40]. However, we did not find a significant association between ICG-A and postoperative complications,
Though the association between ICG-A and complications was not significant, complication rate was much higher in the group demonstrating insufficient ICG-A. This suggests that an inadequate angiography should result in thorough reevaluation of the surgical procedure, with particular emphasis on enhancing postoperative monitoring and care. This is essential to preempt potential complications.
Administration of adjuvant RT may be the most important risk factor for developing surgical-site complications [41, 42]. Analysis of association between complications and RT was not accomplished due to few patients receiving RT with no difference between groups.
There was no difference in overall postoperative QoL or satisfaction with scars, which is consistent to previous studies [14].
Adjuvant therapy was administered on time in > 80%. The majority of patients receiving delayed adjuvant treatment were caused by non-surgical reasons. During follow-up 1 patient developed lymphedema of the upper extremity which could be related the postoperative adjuvant treatment consisting of RT [43].
Limitations
This study is a RCT with 1 year follow-up. All but 1 patient completed the postoperative follow-up eliminating the risk of missing data.
The study is limited by a relatively small sample size of 39 patients. Unfortunately, due to structural changes, it was not possible to include the number of patients initially planned making the study prone to bias, and conclusions is to be assessed considering this.
Conclusions
This randomized controlled study investigated the use of iNPWT by Prevena™ compared to conventional postoperative dressing in immediate breast reconstructions using implants or tissue expanders. Furthermore, ICG-A was applied to investigate intraoperative tissue perfusion and postoperative complications.
No significant difference in time to recovery and time of hospitalization were found.
The 2 groups did not differ in rate of postoperative complications, QoL and satisfaction with scars within 1 year follow-up.
Though the rate of major complications were higher in the group with insufficient intraoperative ICG-A, there was no significant association between ICG-A and postoperative complications.
Larger randomized studies applying intraoperative ICG-A are needed to obtain higher quality data.
Availability of data and material
All data is obtained and stored anonymously (according to the General Data Protection Regulation (GDPR)) by the corresponding author (EL).
References
World Health Organization (2021) Breast cancer
Laustsen-Kiel CM, Hansen L, Lauritzen E, Damsgaard TE. Breast reconstruction and breast cancer-related lymphedema: insights and perspectives. Plast Aesthet Res. 2024;11:17. Available from: https://www.oaepublish.com/articles/2347-9264.2024.32
Christiansen P, Mele M, Bodilsen A, Rocco N, Zachariae R (2022) Breast-Conserving Surgery or Mastectomy? Annals of Surgery Open 3(4):e205
Matar DY, Wu M, Haug V, Orgill DP, Panayi AC (2022) Surgical complications in immediate and delayed breast reconstruction: A systematic review and meta-analysis. Vol. 75, Journal of Plastic, Reconstructive and Aesthetic Surgery. Churchill Livingstone, pp 4085–95
Hangge PT, Jogerst K, Mohsen A, Kosiorek H, Cronin PA, Stucky CCH et al (2019) Making an informed choice: Which breast reconstruction type has the lowest complication rate? Am J Surg 218(6):1040–1045
Finlay B, Kollias V, Hall KA, Clement Z, Bingham J, Whitfield R et al (2021) Long-term outcomes of breast reconstruction and the need for revision surgery. ANZ J Surg 91(9):1751–1758
Yao A, Greige N, Ricci JA, Draper LB, Weichman KE (2023) Topical Nitroglycerin Ointment Reduces Mastectomy Flap Necrosis in Immediate Autologous Breast Reconstruction. Plast Reconstr Surg 152(4):728–735
Gabriel A, Maxwell GP (2019) Economic Analysis Based on the Use of Closed-Incision Negative-Pressure Therapy after Postoperative Breast Reconstruction. Plast Reconstr Surg 143(1):36S-40S
Song J, Liu X, Wu T (2023) Effectiveness of prophylactic application of negative pressure wound therapy in stopping surgical site wound problems for closed incisions in breast cancer surgery: A meta-analysis. Int Wound J 20(2):241–250
Matusiak D, Wichtowski M, Pieszko K, Kobylarek D, Murawa D (2019) Is negative-pressure wound therapy beneficial in modern-day breast surgery? Vol. 23, Wspolczesna Onkologia. Termedia Publishing House Ltd, pp 69–73
AbdelDayem AM, Nashed GA, Balamoun HA, Mostafa MS (2023) Effectiveness of 3-day prophylactic negative pressure wound therapy on closed abdominal incisions in the prevention of wound complications: a randomized controlled trial. J Gastrointest Surg. 27(8):1702–1709. https://doi.org/10.1007/s11605-023-05752-3
Tran B, Johnson A, Shen C, Lee B, Lee E (2019) Closed-Incision Negative-Pressure Therapy Efficacy in Abdominal Wall Reconstruction in High-Risk Patients: A Meta-analysis. J Surg Res 241:63–71
Tanaydin V, Beugels J, Andriessen A, Sawor JH, van der Hulst RRWJ (2018) Randomized Controlled Study Comparing Disposable Negative-Pressure Wound Therapy with Standard Care in Bilateral Breast Reduction Mammoplasty Evaluating Surgical Site Complications and Scar Quality. Aesthetic Plast Surg 42(4):927–935
Pieszko K, Pieszko K, Wichtowski M, Cieśla S, Ławnicka A, Jamont R et al (2023) A Randomized Study Comparing Closed-Incision Negative-Pressure Wound Therapy with Standard Care in Immediate Breast Reconstruction. Plastic and Reconstructive Surgery. Lippincott Williams and Wilkins, pp 1123–33
Cagney D, Simmons L, O’Leary DP, Corrigan M, Kelly L, O’Sullivan MJ et al (2020) The Efficacy of Prophylactic Negative Pressure Wound Therapy for Closed Incisions in Breast Surgery: A Systematic Review and Meta-Analysis. Vol. 44, World Journal of Surgery. Springer, pp 1526–37
Vidya R, Khosla M, Baek K, Vinayagam R, Thekkinkattil D, Laws S et al (2023) Prophylactic Use of Negative Pressure Wound Therapy in High-risk Patients Undergoing Oncoplastic and Reconstructive Breast Surgery. Plastic and Reconstructive Surgery - Global Open. Lippincott Williams and Wilkins, p E5488
Lauritzen E, Damsgaard TE (2021) Use of indocyanine green angiography decreases the risk of complications in autologous- and implant-based breast reconstruction: a systematic review and meta-analysis. J Plast Reconstr Aesthet Surg 74(8):1703–1717. https://doi.org/10.1016/j.bjps.2021.03.034
Pruimboom T, Schols RM, Van Kuijk SM, Van der Hulst RR, Qiu SS (2020) Indocyanine green angiography for preventing postoperative mastectomy skin flap necrosis in immediate breast reconstruction. Cochrane Database Syst Rev 4(4):CD013280. https://doi.org/10.1002/14651858.CD013280
Park JW, Lee MK, Woo KJ (2022) Influence of vertical location and spacing of perforators on perfusion in deep inferior epigastric artery perforator flap breast reconstruction: quantitative analysis using indocyanine green angiography. Gland Surg. 0(0):0–0
Varela R, Casado-Sanchez C, Zarbakhsh S, Diez J, Hernandez-Godoy J, Landin L (2020) Outcomes of DIEP flap and fluorescent angiography: a randomized controlled clinical trial. Plast Reconstr Surg. 145(1):1–10. https://doi.org/10.1097/PRS.0000000000006393
Chu W, Chennamsetty A, Toroussian R, Lau C (2017) Anaphylactic Shock After Intravenous Administration of Indocyanine Green During Robotic Partial Nephrectomy. Urol Case Rep 1(12):37–38
Sil A, Kumar P, Kumar R, Das NK (2019) Selection of control, randomization, blinding, and allocation concealment. Indian Dermatol Online J 10(5):601–605
Lauritzen E, Bredgaard R, Bonde C, Jensen LT, Damsgaard TE (2022) Indocyanine green angiography in breast reconstruction: a narrative review. Ann Breast Surg 6:6
Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL (2017) Breast cancer and reconstruction: Normative data for interpreting the BREAST-Q. Plast Reconstr Surg 139(5):1046e-e1055
Moyer HR, Losken A (2012) Predicting mastectomy skin flap necrosis with indocyanine green angiography: The gray area defined. Plast Reconstr Surg 129(5):1043–1048
Kim DY, Park SJ, Bang SI, Mun GH, Pyon JK (2016) Does the Use of Incisional Negative-Pressure Wound Therapy Prevent Mastectomy Flap Necrosis in Immediate Expander-Based Breast Reconstruction? Plast Reconstr Surg 138(3):558–566
Willert CB, Gjørup CA, Hölmich LR (2020) Danish translation and linguistic validation of the BREAST-Q. Dan Med J 67(5):A08190445
Ryu JY, Lee JH, Kim JS, Lee JS, Lee JW, Choi KY, Chung HY, Cho BC, Yang JD (2022) Usefulness of incisional negative pressure wound therapy for decreasing wound complication rates and seroma formation following prepectoral breast reconstruction. Aesthetic Plast Surg 46(2):633–641. https://doi.org/10.1007/s00266-020-02115-0
Wareham CM, Karamchandani MM, Ku GDLC, Gaffney K, Sekigami Y, Persing SM et al (2023) Closed Incision Negative Pressure Therapy in Oncoplastic Breast Surgery: A Comparison of Outcomes. Plastic and Reconstructive Surgery - Global Open. Lippincott Williams and Wilkins, p E4936
Kilgore LJ, Korentager SS, Hangge AN, Amin AL, Balanoff CR, Larson KE et al (2018) Reducing Breast Cancer-Related Lymphedema (BCRL) Through Prospective Surveillance Monitoring Using Bioimpedance Spectroscopy (BIS) and Patient Directed Self-Interventions. Ann Surg Oncol 25(10):2948–2952
Lie KH, Barker AS, Ashton MW (2013) A classification system for partial and complete diep flap necrosis based on a review of 17,096 DIEP flaps in 693 articles including analysis of 152 total flap failures. Plast Reconstr Surg 132(6):1401–1408
Tanaydin V, Beugels J, Andriessen A, Sawor JH, van der Hulst RRWJ (2018) Randomized Controlled Study Comparing Disposable Negative-Pressure Wound Therapy with Standard Care in Bilateral Breast Reduction Mammoplasty Evaluating Surgical Site Complications and Scar Quality. Aesthetic Plast Surg 42(4):927–935
Al-Ishaq Z, Rahman E, Salem F, Taj S, Mula-Hussain L, Mylvaganam S, Vidya R, Matey P, Sircar T (2023) Is using closed incision negative pressure therapy in reconstructive and oncoplastic breast surgery helpful in reducing skin necrosis? Cureus 15(4):e38167. https://doi.org/10.7759/cureus.38167
Mirhaidari SJ, Beddell GM, Orlando MV, Parker MG, Pedersen JC, Wagner DS (2018) A Prospective Study of Immediate Breast Reconstruction with Laser-Assisted Indocyanine Green Angiography. Plast Reconstr Surg Glob Open 6(9):e1774
Kim MJ, Mok JH, Lee IJ, Lim H. Mastectomy Skin Flap Stability Prediction Using Indocyanine Green Angiography: A Randomized Prospective Trial. Aesthet Surg J. 2023; Available from: https://academic.oup.com/asj/advance-article/doi/10.1093/asj/sjad226/7223444
Phillips BT, Lanier ST, Conkling N, Wang ED, Dagum AB, Ganz JC et al (2012) Intraoperative perfusion techniques can accurately predict mastectomy skin flap necrosis in breast reconstruction: Results of a prospective trial. Plast Reconstr Surg 129(5):778–788
Munabi NCO, Olorunnipa OB, Goltsman D, Rohde CH, Ascherman JA. The ability of intra-operative perfusion mapping with laser-assisted indocyanine green angiography to predict mastectomy flap necrosis in breast reconstruction: A prospective trial. Journal of Plastic, Reconstructive and Aesthetic Surgery. 2014;67(4):449–55. Available from: https://doi.org/10.1016/j.bjps.2013.12.040
Mattison GL, Lewis PG, Gupta SC, Kim HY (2016) SPY imaging use in postmastectomy breast reconstruction patients: Preventative or overly conservative? Plast Reconstr Surg 138(1):15e–21e
Rinker B (2016) A Comparison of Methods to Assess Mastectomy Flap Viability in Skin-Sparing Mastectomy and Immediate Reconstruction: A Prospective Cohort Study. Plast Reconstr Surg 137(2):395–401
Chirappapha P, Chansoon T, Bureewong S, Phosuwan S, Lertsithichai P, Sukarayothin T, Leesombatpaiboon M, Vassanasiri W (2020) Is it reasonable to use indocyanine green fluorescence imaging to determine the border of pedicled TRAM flap zone IV? Plast Reconstr Surg Glob Open 8(9):e3093. https://doi.org/10.1097/GOX.0000000000003093
AlluéCabañuz M, del ArribasAmo MD, Navarro Barlés A, Guemes Sanchez AT (2019) Influence of radiotherapy on immediate breast reconstruction after skin-sparing mastectomy. Before or after: Does it matter? Cir Esp. 97(3):156–61
Rojas DP, Leonardi MC, Frassoni S, Morra A, Gerardi MA, La Rocca E et al (2021) Implant risk failure in patients undergoing postmastectomy 3-week hypofractionated radiotherapy after immediate reconstruction: Implant failure after breast hypofractionated radiotherapy. Radiother Oncol 1(163):105–113
Hayes SC, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphedema after breast cancer: Incidence, risk factors, and effect on upper body function. J Clin Oncol 26(21):3536–3542
Funding
Open access funding provided by Copenhagen University
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Participants provided informed consent for publication of the images in Fig. 1–3.
Conflict of Interest
Elisabeth Lauritzen, Claes Hannibal Kiilerich, Rikke Bredgaard, Tove Tvedskov, Tine Engberg Damsgaard declare no conflict of interest.
Ethical statement
The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The study was approved by The Central Denmark Region Committees on Health Research Ethics (H-19074545, 70429) and conducted in accordance with the Helsinki declaration (as revised in 2013).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary Material 1: Video 1. Prepectoral implant-based IBR. Intraoperative ICG-A showing sufficient perfusion.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Lauritzen, E., Kiilerich, C.H., Bredgaard, R. et al. Incisional negative pressure wound therapy (PrevenaTM) vs. conventional post-operative dressing after immediate breast reconstruction: a randomized controlled clinical trial. Eur J Plast Surg 47, 79 (2024). https://doi.org/10.1007/s00238-024-02223-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02223-z