Abstract
Background
Surgical repair of muscle lacerations is the standard of care to restore function. Compared to non-surgically repaired lacerations, surgical repairs have been shown to heal faster and have higher strength return and lower incidence of hematomas. Multiple techniques have been reported to repair muscle lacerations. There are many factors to consider in choosing a technique for muscle belly repair including scar tissue formation, length of immobilization, strength of repair, and suture pullout. An ideal repair method has not yet been clearly identified; therefore, the purpose of this review is to evaluate the existing literature on various repair methods and the methods used to test them.
Methods
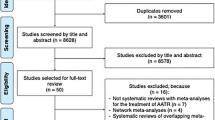
Using the PRISMA-ScR framework, a scoping review was performed to identify biomechanical studies that examined the strength and efficacy of muscle belly repair techniques. PubMed, Web of Science, and Scopus were searched to locate relevant studies.
Results
Nine original studies which met inclusion criteria were selected for final review. Six studies evaluated specific suture techniques, while the remaining three studies evaluated, inclusion of epimysium in the repair, repair of the epimysium versus perimysium, and porcine versus bovine skeletal muscle biomechanical properties. While the six studies evaluating suture techniques tested overlapping suture types, they varied in preload and peak load values and the type of suture used, yielding heterogenous data. The compiled data did not support one method being the optimal repair choice.
Conclusions
Existing literature evaluating the mechanics of muscle repair is limited by a lack of standardization. The included studies suggest that using sutures which incorporate the epimysium or using a combination of sutures that anchor the core of the muscle belly and encompass the perimeter may yield more robust repairs than other techniques. However, further research using comparable experimental conditions is necessary to identify an ideal muscle belly repair technique.
Level of evidence: Not gradable.



Similar content being viewed by others
Data Availability
The authors declare that the data supporting the findings of this review are included in the paper itself and in the articles referenced therein.
References
Oliva F, Via AG, Kiritsi O, Foti C, Maffulli N (2013) Surgical repair of muscle laceration: biomechanical properties at 6 years follow-up. Muscles Ligaments Tendons J 3(4):313–317
Castillo AC, Kaltwasser K, Morris R et al (2021) Comparing 3 suture techniques after muscle laceration repair. HAND 16(1):67–72. https://doi.org/10.1177/1558944719837021
Menetrey J, Kasemkijwattana C, Fu FH, Moreland MS, Huard J (1999) Suturing versus immobilization of a muscle laceration. Am J Sports Med 27(2):222–229. https://doi.org/10.1177/03635465990270021801
Tricco AC, Lillie E, Zarin W et al (2018) PRISMA Extension for Scoping Reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med 169(7):467–473. https://doi.org/10.7326/M18-0850
Kragh JF, Svoboda SJ, Wenke JC, Ward JA, Walters TJ (2005) Epimysium and perimysium in suturing in skeletal muscle lacerations. J Trauma 59(1):209–212. https://doi.org/10.1097/01.ta.0000171530.11588.70
Kragh JF, Svoboda SJ, Wenke JC, Brooks DE, Bice TG, Walters TJ (2005) The role of epimysium in suturing skeletal muscle lacerations. J Am Coll Surg 200(1):38–44. https://doi.org/10.1016/j.jamcollsurg.2004.09.009
Kragh JF, Svoboda SJ, Wenke JC, Ward JA, Walters TJ (2005) Passive biomechanical properties of sutured mammalian muscle lacerations. J Invest Surg 18(1):19–23. https://doi.org/10.1080/08941930590905170
He M, Sebastin SJ, Gan AWT, Lim AYT, Chong AKS (2014) Biomechanical comparison of different suturing techniques in rabbit medial gastrocnemius muscle laceration repair. Ann Plast Surg 73(3):333–335. https://doi.org/10.1097/SAP.0b013e31827ae9b0
Goyal KS, Speeckaert AL, Goitz RJ, Tavana ML (2019) A comparison of barbed suture versus traditional techniques for muscle belly repair. Hand N Y N 14(1):91–94. https://doi.org/10.1177/1558944718798853
Chance JR, Krgh JK, Agrawal CM, Basamania CJ (2005) Pullout forces of sutures in muscle lacerations. Orthopedics 28(10):1187–1190. https://doi.org/10.3928/0147-7447-20051001-16
Kragh JF, Svoboda SJ, Wenke JC, Ward JA, Walters TJ. Suturing of lacerations of skeletal muscle. J Bone Joint Surg Br. 2005;87-B(9):1303–1305. doi:https://doi.org/10.1302/0301-620X.87B9.15728
Lionello G, Fognani R, Baleani M, Sudanese A, Toni A (2015) Suturing the myotendinous junction in total hip arthroplasty: a biomechanical comparison of different stitching techniques. Clin Biomech 30(10):1077–1082. https://doi.org/10.1016/j.clinbiomech.2015.09.003
Julien TP, Mudgal CS (2011) Anchor suture technique for muscle belly repair. Tech Hand Up Extrem Surg 15(4):257–259. https://doi.org/10.1097/BTH.0b013e318220e75a
Green CJ, Wang A, Henderson J, Ebert J, Edwards P (2020) Successful surgical repair of a full-thickness intramuscular muscle belly rupture of pectoralis major. JSES Int 4(1):91–94. https://doi.org/10.1016/j.jses.2019.10.006
Järvinen MJ, Lehto MUK (1993) The effects of early mobilisation and immobilisation on the healing process following muscle injuries. Sports Med 15(2):78–89. https://doi.org/10.2165/00007256-199315020-00002
Kannus P (2000) Immobilization or early mobilization after an acute soft-tissue injury? Phys Sportsmed 28(3):55–63. https://doi.org/10.3810/psm.2000.03.775
Almekinders LC (1991) Results of surgical repair versus splinting of experimentally transected muscle. J Orthop Trauma 5(2):173–176. https://doi.org/10.1097/00005131-199105020-00009
Maddox GE, Ludwig J, Craig ER et al (2015) Flexor tendon repair with a knotless, bidirectional barbed suture: an in vivo biomechanical analysis. J Hand Surg 40(5):963–968. https://doi.org/10.1016/j.jhsa.2015.01.013
Çolak Ö, Kankaya Y, Sungur N et al (2019) Barbed sutures versus conventional tenorrhaphy in flexor tendon repair: an ex vivo biomechanical analysis. Arch Plast Surg 46(03):228–234. https://doi.org/10.5999/aps.2018.00962
Shah A, Rowlands M, Au A (2015) Barbed sutures and tendon repair—a review. HAND 10(1):6–15. https://doi.org/10.1007/s11552-014-9669-z
Shin JY, Kim JS, Roh SG, Lee NH, Yang KM (2016) Biomechanical analysis of barbed suture in flexor tendon repair versus conventional method: systematic review and meta-analysis. Plast Reconstr Surg 138(4):666e–674e. https://doi.org/10.1097/PRS.0000000000002573
Huang Y, Cadet ER, King MW, Cole JH (2022) Comparison of the mechanical properties and anchoring performance of polyvinylidene fluoride and polypropylene barbed sutures for tendon repair. J Biomed Mater Res B Appl Biomater 110(10):2258–2265. https://doi.org/10.1002/jbm.b.35074
Miller B, Dodds SD, deMars A, Zagoreas N, Waitayawinyu T, Trumble TE (2007) Flexor tendon repairs: the impact of fiberwire on grasping and locking core sutures. J Hand Surg 32(5):591–596. https://doi.org/10.1016/j.jhsa.2007.03.003
Kim HM, Nelson G, Thomopoulos S, Silva MJ, Das R, Gelberman RH (2010) Technical and biological modifications for enhanced flexor tendon repair. J Hand Surg 35(6):1031–1037. https://doi.org/10.1016/j.jhsa.2009.12.044
Rawson S, Cartmell S, Wong J (2013) Suture techniques for tendon repair; a comparative review. Muscles Ligaments Tendons J 3(3):220–228
Gelberman RH, Boyer MI, Brodt MD, Winters SC, Silva MJ. The effect of gap formation at the repair site on the strength and excursion of Intrasynovial flexor tendons. An experimental study on the early stages of tendon-healing in dogs*: J Bone Jt Surg. 1999;81(7):975–982. doi:https://doi.org/10.2106/00004623-199907000-00010
Terada, Shinichiro Takayama, Harumo N. Muscle repair after a transsection injury with development of a gap: an experimental study in rats. Scand J Plast Reconstr Surg Hand Surg. 2001;35(3):233–238. doi:https://doi.org/10.1080/028443101750523131
Gardner T, Kenter K, Li Y (2020) Fibrosis following acute skeletal muscle injury: mitigation and reversal potential in the clinic. J Sports Med 2020:1–7. https://doi.org/10.1155/2020/7059057
Maquirriain J (2011) Achilles tendon rupture: avoiding tendon lengthening during surgical repair and rehabilitation. Yale J Biol Med 84(3):289–300
Fischer B, Kurz S, Höch A, Schleifenbaum S (2020) The influence of different sample preparation on mechanical properties of human iliotibial tract. Sci Rep 10(1):14836. https://doi.org/10.1038/s41598-020-71790-5
Lansdown DA, Riff AJ, Meadows M, Yanke AB, Bach BR (2017) What factors influence the biomechanical properties of allograft tissue for ACL reconstruction? A systematic review Clin Orthop 475(10):2412–2426. https://doi.org/10.1007/s11999-017-5330-9
Hammer N, Lingslebe U, Aust G, Milani TL, Hädrich C, Steinke H (2012) Ultimate stress and age-dependent deformation characteristics of the iliotibial tract. J Mech Behav Biomed Mater 16:81–86. https://doi.org/10.1016/j.jmbbm.2012.04.025
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLOS Med 18(3):e1003583. https://doi.org/10.1371/journal.pmed.1003583
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
Ethical approval was not required for this study.
Consent to participate
Consent to participate was not required for this study.
Consent for publication
Consent to publish was not required for this study.
Competing interests
Avril Stulginski, Medha Vallurupalli, Mikhail Pakvasa, Cathy J. Tang, Eric D. Wang, and Amber R. Leis declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix 1. PubMed search
Query | (muscle belly repair OR muscle laceration repair) AND technique AND (biomechanical testing OR tensile) NOT shoulder |
|---|---|
Details | ((((“muscle s”[All Fields] OR “muscles”[MeSH Terms] OR “muscles”[All Fields] OR “muscle”[All Fields]) AND (“bellies”[All Fields] OR “belly”[All Fields]) AND (“repairability”[All Fields] OR “repairable”[All Fields] OR “repaire”[All Fields] OR “repaired”[All Fields] OR “repairment”[All Fields] OR “wound healing”[MeSH Terms] OR (“wound”[All Fields] AND “healing”[All Fields]) OR “wound healing”[All Fields] OR “repair”[All Fields] OR “repairing”[All Fields] OR “repairs”[All Fields])) OR ((“muscle s”[All Fields] OR “muscles”[MeSH Terms] OR “muscles”[All Fields] OR “muscle”[All Fields]) AND (“lacerations”[MeSH Terms] OR “lacerations”[All Fields] OR “lacerate”[All Fields] OR “lacerated”[All Fields] OR “lacerating”[All Fields] OR “laceration”[All Fields]) AND (“repairability”[All Fields] OR “repairable”[All Fields] OR “repaire”[All Fields] OR “repaired”[All Fields] OR “repairment”[All Fields] OR “wound healing”[MeSH Terms] OR (“wound”[All Fields] AND “healing”[All Fields]) OR “wound healing”[All Fields] OR “repair”[All Fields] OR “repairing”[All Fields] OR “repairs”[All Fields]))) AND (“methods”[MeSH Terms] OR “methods”[All Fields] OR “technique”[All Fields] OR “methods”[MeSH Subheading] OR “techniques”[All Fields] OR “technique s”[All Fields]) AND (((“biomechanical phenomena”[MeSH Terms] OR (“biomechanical”[All Fields] AND “phenomena”[All Fields]) OR “biomechanical phenomena”[All Fields] OR “biomechanic”[All Fields] OR “biomechanics”[All Fields] OR “biomechanical”[All Fields] OR “biomechanically”[All Fields]) AND (“test s”[All Fields] OR “tested”[All Fields] OR “testing”[All Fields] OR “testings”[All Fields] OR “tests”[All Fields])) OR (“tensil”[All Fields] OR “tensile”[All Fields]))) NOT (“shoulder”[MeSH Terms] OR “shoulder”[All Fields] OR “shoulders”[All Fields] OR “shoulder s”[All Fields]) |
Translation | muscle: “muscle’s”[All Fields] OR “muscles”[MeSH Terms] OR “muscles”[All Fields] OR “muscle”[All Fields] belly: “bellies”[All Fields] OR “belly”[All Fields] repair: “repairability”[All Fields] OR “repairable”[All Fields] OR “repaire”[All Fields] OR “repaired”[All Fields] OR “repairment”[All Fields] OR “wound healing”[MeSH Terms] OR (“wound”[All Fields] AND “healing”[All Fields]) OR “wound healing”[All Fields] OR “repair”[All Fields] OR “repairing”[All Fields] OR “repairs”[All Fields] muscle: “muscle’s”[All Fields] OR “muscles”[MeSH Terms] OR “muscles”[All Fields] OR “muscle”[All Fields] laceration: “lacerations”[MeSH Terms] OR “lacerations”[All Fields] OR “lacerate”[All Fields] OR “lacerated”[All Fields] OR “lacerating”[All Fields] OR “laceration”[All Fields] repair: “repairability”[All Fields] OR “repairable”[All Fields] OR “repaire”[All Fields] OR “repaired”[All Fields] OR “repairment”[All Fields] OR “wound healing”[MeSH Terms] OR (“wound”[All Fields] AND “healing”[All Fields]) OR “wound healing”[All Fields] OR “repair”[All Fields] OR “repairing”[All Fields] OR “repairs”[All Fields] technique: “methods”[MeSH Terms] OR “methods”[All Fields] OR “technique”[All Fields] OR “methods”[Subheading] OR “techniques”[All Fields] OR “technique’s”[All Fields] biomechanical: “biomechanical phenomena”[MeSH Terms] OR (“biomechanical”[All Fields] AND “phenomena”[All Fields]) OR “biomechanical phenomena”[All Fields] OR “biomechanic”[All Fields] OR “biomechanics”[All Fields] OR “biomechanical”[All Fields] OR “biomechanically”[All Fields] testing: “test’s”[All Fields] OR “tested”[All Fields] OR “testing”[All Fields] OR “testings”[All Fields] OR “tests”[All Fields] tensile: “tensil”[All Fields] OR “tensile”[All Fields] shoulder: “shoulder”[MeSH Terms] OR “shoulder”[All Fields] OR “shoulders”[All Fields] OR “shoulder’s”[All Fields] |
Results | 25 |
Appendix 2. Summary outcomes of suture techniques
Study | Suture technique | Suture type | Preload | Loading | Maximum load | Mean strain | Stiffness | Displacement | Failure mode |
|---|---|---|---|---|---|---|---|---|---|
Kragh et al | Kessler | Size 2, braided polyester | 5–8 N | 25 mm/min | 35.1 N (SD 9.4) | 7.9 (SD 2.9) | - | - | Tear out (n = 5/5) |
He et al | Kessler | Size 5 and 6, polypropylene | 2 N | 60 mm/min | 15.5 N | - | 1 N/mm | - | - |
Chance et al | Kessler | Size 2, braided polyester | - | - | 16.18 N (SD 6.08) | - | - | - | Pullout (n = 12/13) Avulsion (n = 1/13) |
Castillo et al | Mason-Allen | Size 3, polyglactin | - | - | 45.39 N (SD 13.86) | - | 1.76 N/mm (SD 0.68) | 28.45 mm (SD 9.37) at maximum load | - |
Goyal et al | Mason-Allen | Size 1 and 2, Ethibond barbed PDS | 1 N | 60 mm/min | 12.73 N (SD 2.40) | - | - | 1.84 mm (SD 0.39) at 10N | - |
Chance et al | Mason-Allen | Size 2, braided polyester | - | - | 36.58 N (SD 11.28) | - | - | - | Avulsion (n = 13/13) |
Chance et al | Mattress | Size 2, braided polyester | - | - | 18.14 N (SD 5.10) | - | - | - | Avulsion (n = 31/31) |
He et al | Mattress | Size 5 and 6 polypropylene | 2 N | 60 mm/min | 4.4 N | - | 0.3 N/mm | - | - |
Castillo et al | Perimeter | Size 3, polyglactin | 3–5 N | 25 mm/min | 64.29 N (SD 19.30) | - | 3.24 N/mm (SD 0.73) | 64.29 mm (SD 19.30) at maximum load | - |
Chance et al | Perimeter | Size 2, braided polyester | - | - | 43.35 (SD 11.28) | - | - | - | Avulsion (n = 12/13) Pullout (n = 1/13) |
Kragh et al | MAP | Size 2, braided polyester | 5–8 N | 25 mm/min | 74 N (SD 11.3) | 12.2 (SD 3.7 | - | - | No failure |
Chance et al | MAP | Size 2, braided polyester | - | - | 62.76 N (SD 13.73) | - | - | - | Avulsion (n = 13/13) |
He et al | MAP | Size 5 and 6, polypropylene | 2 N | 60 mm/min | 13.2 N | - | 0.6 N/mm | - | - |
Castillo et al | Figure-of-8 | Size 3, polyglactin | 3–5 N | 25 mm/min | 54.18 N (SD 21.47) | - | 2.52 N/mm (SD 0.99) | 27.22 mm (SD 6.64) at maximum load | - |
Goyal et al | Figure-of-8 | Size 1 and 2, Ethibond barbed PDS | 1 N | 60 mm/min | 8.96 N (SD 4.24) | - | - | - | - |
Lionello et al | Figure-of-8 | Size 2, polyglactin | 10 N | 0.1 N/s | 59 N | - | 5 N/mm | - | - |
Chance et al | Figure-of-8 | Size 2, braided polyester | - | - | 17.36 N (SD 4.31) | - | - | - | Pullout (n = 13/13) |
Goyal et al | Modified Kessler | Size 1 and 2, Ethibond barbed PDS | 1 N | 60 mm/min | 7.71 N (SD 3.78) | - | - | - | - |
Lionello et al | Simple | Size 2, polyglactin | 10 N | 0.1 N/s | 61 N | - | - | - | - |
Goyal et al. (Barbed) | Custom/novel | Size 1 and 2 Ethibond barbed PDS | 1 N | 60 mm/min | 17.86 N (SD 2.26) | - | - | 1.57 mm (SD 0.39) at 10 N | - |
Goyal et al. (Ethibond) | Custom/novel | Size 1 and 2 Ethibond barbed PDS | 1 N | 60 mm/min | 13.16 N (SD 1.57) | - | - | 3.55 mm (SD 0.78) at 10 N | - |
Lionello et al | Custom/novel | Size 2, polyglactin | 10 N | 0.1 N/s | 85 N | - | 5.4 N/mm | - | - |
Rights and permissions
About this article
Cite this article
Stulginski, A., Vallurupalli, M., Pakvasa, M. et al. Evaluating suturing methods for surgical repair of muscle belly lacerations: a scoping review of biomechanical studies. Eur J Plast Surg 47, 23 (2024). https://doi.org/10.1007/s00238-024-02161-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00238-024-02161-w