Abstract
Background
The most significant complication of free flap reconstruction is flap failure, which can be a result of numerous factors but ultimately affecting the vascularity of the flap tissues. In cases of doubtful flap viability re-exploration in the early postoperative period has a better salvage rate than the late postoperative period in free flaps. We aim to analize the salvage rate of free flaps undergoing re-exploration in different time periods in the postoperative phase.
Methods
This is a retrospective analysis of charts of 376 patients who underwent free tissue transfer during 4 consecutive years from August 2013 to July 2017 for the reconstruction of post-oncological resection defects among which 43 patients underwent re-exploration. Indications for re-exploration were vascular compromise indicated by absent or very delayed bleeding, brisk dark bleeding, suspected haematoma, chyle collection, etc.
Results
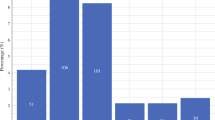
Among 43 patients who underwent re-exploration, 3 patients were re-explored on the operative day itself, 23 on the 1st postoperative day, 6 on the 2nd day, 4 on the 3rd day, 5 on the 4th day and 2 on the 5th day with salvage rates of 100%, 48%, 50%, 20%, 20% and 0% respectively. Findings on re-exploration included arterial/venous thrombosis, haematoma, chyle collection, external compression on pedicle/perforator by nerve, etc.
Conclusions
Analysing the data collected from this series of patients who underwent re-exploration, it has been observed that the re-explorations performed in the early postoperative period have a better chance of salvaging the flap. Although it is intuitive that a high index of suspicion followed by early re-exploration will improve the salvage rate, this paper attends to back this up with evidence.
Level of evidence: Level III, risk/prognostic study.










Similar content being viewed by others
References
Tamai S (2009) History of microsurgery. Plast Reconstr Surg. 124(6S):e282–e294
O’Neill JP, Shine N, Eadie PA, Beausang E, Timon C (2010) Free tissue transfer versus pedicled flap reconstruction of head and neck malignancy defects. Ir J Med Sci. 179(3):337–343
Rosenthal EL, Dixon SF (2003) Free flap complications: when is enough, enough? Curr Opin Otolaryngol Head Neck Surg. 11(4):236–239
Abemayor E, Blackwell KE (2000) Reconstruction of soft tissue defects in the oral cavity and oropharynx. Arch Otolaryngol Head Neck Surg. 126(7):909–912
Bui DT, Cordeiro PG, Hu QY, Disa JJ, Pusic A, Mehrara BJ (2007) Free flap reexploration: indications, treatment, and outcomes in 1193 free flaps. Plast Reconstr Surg. 119(7):2092–2100
Valentini V, Cassoni A, Marianetti TM, Mitro V, Gennaro P, Ialongo C, Iannetti G (2008) Diabetes as main risk factor in head and neck reconstructive surgery with free flaps. J Craniofac Surg. 19(4):1080–1084
Joo YH, Sun DI, Park JO, Cho KJ, Kim MS (2010) Risk factors of free flap compromise in 247 cases of microvascular head and neck reconstruction: a single surgeon’s experience. Eur Arch Otorhinolaryngol. 267(10):1629–1633
Schusterman MA, Miller MJ, Reece GP, Kroll SS, Marchi M, Goepfert H (1994) A single center’s experience with 308 free flaps for repair of head and neck cancer defects. Plast Reconstr Surg. 93(3):472–478
Duncan MJ, Manktelow RT, Zuker RM, Rosen IB (1985) Mandibular reconstruction in the radiated patient: the role of osteocutaneous free tissue transfers. Plast Reconstr Surg. 76(6):829–840
Maruccia M, Fallico N, Cigna E, Ciudad P, Nicoli F, Trignano E, Nacchiero E, Giudice G, Ribuffo D, Chen HC (2017) Suprafascial versus traditional harvesting technique for free antero lateral thigh flap: a case-control study to assess the best functional and aesthetic result in extremity reconstruction. Microsurgery. 37:851–857
Schwarzer C, Mücke T, Wolff KD, Loeffelbein DJ, Rau A (2016) Donor site morbidity and flap perfusion of subfascial and suprafascial radial forearm flaps: a randomized prospective clinical comparison trial. J Cranio Maxill Surg. 44(9):1299–1304
Kroll SS, Schusterman MA, Reece GP, Miller MJ, Evans GRD, Robb GL, Baldwin BJ (1996) Timing of pedicle thrombosis and flap loss after free-tissue transfer. Plast Reconstr Surg. 98(7):1230–1233
Chen KT, Mardini S, Wei FC et al (2007) Timing of presentation of the first signs of vascular compromise dictates the salvage outcome of free flap transfers. Plast Reconstr Surg 120(1):187–195
Brown JS, Devine JC, Magennis P, Sillifant P, Rogers SN, Vaughan ED (2003) Factors that influence the outcome of salvage in free tissue transfer. Br J Oral Maxillofac Surg. 41(1):16–20
Smit JM, Acosta R, Zeebregts CJ, Liss AG, Anniko M, Hartman EH (2007) Early reintervention of compromised free flaps improves success rate. Microsurgery. 27(7):612–616
Novakovic D, Patel RS, Goldstein DP, Gullane PJ (2009) Salvage of failed free flaps used in head and neck reconstruction. Head Neck Oncol. 1(1):33
Hyodo I, Nakayama B, Kato H, Hasegawa Y, Ogawa T, Terada A, Torii S (2007) Analysis of salvage operation in head and neck microsurgical reconstruction. Laryngoscope. 117(2):357–360
Yu P, Chang DW, Miller MJ, Reece G, Robb GL (2009) Analysis of 49 cases of flap compromise in 1310 free flaps for head and neck reconstruction. Head Neck. 31(1):45–51
Siemionow M, Arslan E (2004) Ischemia/reperfusion injury: a review in relation to free tissue transfers. Microsurgery. 24(6):468–475
Acknowledgements
The authors would like to thank Dr. Vivek Koushik and Mr. Balasubramaniam Ramakrishnan.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection and analysis were performed by Dr. Jijo Joseph. The first draft of the manuscript was written by Dr. Jijo Joseph and Dr. Shivaram Bharathwaj. All other authors edited, proofread and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Jijo Joseph, Antony Arvind, Shivaram Bharadwaj, G. B. Rajan and Hari Krishna M. declare no conflict of interest.
Ethics approval
The local research ethics committee has confirmed that no ethical approval is required for retrospective studies.
Informed consent to participate
Informed consent was obtained from all the participants included in the study.
Patient consent
Patients signed consent regarding publishing their data and photographs.
Code availability
Not applicable.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Joseph, J., Bharathwaj, S., Arvind, A. et al. Re-exploration in the early postoperative period has a better salvage rate in free flaps. Eur J Plast Surg 44, 219–230 (2021). https://doi.org/10.1007/s00238-020-01744-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-020-01744-7