Abstract
Background
Breast reconstruction (BR) has revealed significant benefits on physical and psychological well-being. Satisfaction is currently a key outcome on BR. This study aimed to assess the impact of timing and reconstructive technique on satisfaction, monitoring the influence of patient’s characteristics and complications.
Methods
A single-center study of women undergoing primary BR over a 4.5-year period was conducted. Demographics, clinical features, procedural data, and postoperative complications were assessed. Patient satisfaction was evaluated with the BREAST-Q™. Influence of BR timing (immediate vs. delayed) and surgical technique (autologous vs. implant-based) on satisfaction was analyzed. Univariate and multivariate analyses were performed to identify independent predictors of satisfaction.
Results
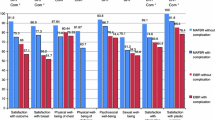
Global response rate to BREAST-Q™ was 76.1% (216 from 284 patients). Responders underwent delayed BR in 67.6%, and autologous BR in 68.5%, with a 30.1% overall complication rate. Timing demonstrated significant impact on satisfaction (p = 0.001), with delayed reconstruction showing a higher mean BREAST-Q™ score. Autologous reconstruction also had a significantly higher BREAST-Q™ (p = 0.002). Transverse rectus abdominis myocutaneous flap presented the highest score, followed by latissimus dorsi with implant, and implant-based showed the lowest satisfaction (p = 0.004). Multivariate regression analysis identified timing, minor complications, and smoking status as independent impact factors of satisfaction (p = 0.001, p = 0.043, and p = 0.011, respectively).
Conclusions
Timing significantly affected satisfaction (delayed reconstruction evidencing positive influence). Technique did not reach significance as independent predictor. Smoking and minor complications showed negative influence. Meaningful satisfaction with delayed reconstruction may encourage BR in the majority of patients, even those with medical or oncologic risks that precluded immediate reconstruction.
Level of evidence: Not ratable.
Similar content being viewed by others
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68:394–424
Alderman AK, Kuhn LE, Lowery JC, Wilkins EG (2007) Does patient satisfaction with breast reconstruction change over time? Two-year results of the Michigan Breast Reconstruction Outcomes Study. J Am Coll Surg 204:7–12
Chen W, Lv X, Xu X, Gao X, Wang B (2018) Meta-analysis for psychological impact of breast reconstruction in patients with breast cancer. Breast Cancer 25:464–469
Filip CI, Jecan CR, Raducu L, Neagu TP, Florescu IP (2017) Immediate versus delayed breast reconstruction for postmastectomy patients. Controversies and solutions. Chirurgia (Bucur) 112:378–386
D'Souza N, Darmanin G, Fedorowicz Z (2011) Immediate versus delayed reconstruction following surgery for breast cancer. Cochrane Database Syst Rev 7:CD008674
Juhl AA, Christensen S, Zachariae R, Damsgaard TE (2017) Unilateral breast reconstruction after mastectomy—patient satisfaction, aesthetic outcome and quality of life. Acta Oncol 56:225–231
Thamm OC, Andree C (2018) Immediate versus delayed breast reconstruction: evolving concepts and evidence base. Clin Plast Surg 45:119–127
Nelson JA, Lee IT, Disa JJ (2018) The functional impact of breast reconstruction: an overview and update. Plast Reconstr Surg Glob Open 6:e1640
Craig E, Shah A, Persing S, Salomon J, Fusi S (2015) Simultaneous expander and deep inferior epigastric perforator reconstruction: indications and alloderm sling technique for protecting the anastomosis. Plast Aesthet Res 2:63–68
Saulis AS, Mustoe TA, Fine NA (2007) A retrospective analysis of patient satisfaction with immediate postmastectomy breast reconstruction: comparison of three common procedures. Plast Reconstr Surg 119:1669–1676
Yueh JH, Slavin SA, Adesiyun T, Nyame TT, Gautam S, Morris DJ, Tobias AM, Lee BT (2010) Patient satisfaction in postmastectomy breast reconstruction: a comparative evaluation of DIEP, TRAM, latissimus flap, and implant techniques. Plast Reconstr Surg 125:1585–1595
Kazzazi F, Haggie R, Forouhi P, Kazzazi N, Wyld L, Malata CM (2018) A comparison of patient satisfaction (using the BREAST-Q questionnaire) with bilateral breast reconstruction following risk-reducing or therapeutic mastectomy. J Plast Reconstr Aesthet Surg 71:1324–1331
Yoon AP, Qi J, Brown DL, Kim HM, Hamill JB, Erdmann-Sager J, Pusic AL, Wilkins EG (2018) Outcomes of immediate versus delayed breast reconstruction: results of a multicenter prospective study. Breast 37:72–79
Atisha D, Alderman AK, Lowery JC, Kuhn LE, Davis J, Wilkins EG (2008) Prospective analysis of long-term psychosocial outcomes in breast reconstruction: two-year postoperative results from the Michigan Breast Reconstruction Outcomes Study. Ann Surg 247:1019–1028
Platt J, Zhong T (2018) Patient-centered breast reconstruction based on health-related quality-of-life evidence. Clin Plast Surg 45:137–143
Pusic AL, Klassen AF, Scott AM, Klok JA, Cordeiro PG, Cano SJ (2009) Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg 124:345–353
Pusic AL, Matros E, Fine N, Buchel E, Gordillo GM, Hamill JB, Kim HM, Qi J, Albornoz C, Klassen AF, Wilkins EG (2017) Patient-reported outcomes 1 year after immediate breast reconstruction: results of the mastectomy reconstruction outcomes consortium study. J Clin Oncol 35:2499–2506
Pinsolle V, Grinfeder C, Mathoulin-Pelissier S, Faucher A (2006) Complications analysis of 266 immediate breast reconstructions. J Plast Reconstr Aesthet Surg 59:1017–1024
Santosa KB, Qi J, Kim HM, Hamill JB, Wilkins EG, Pusic AL (2018) Long-term patient-reported outcomes in postmastectomy breast reconstruction. JAMA Surg 153:891–899
Dean NR, Crittenden T (2016) A five year experience of measuring clinical effectiveness in a breast reconstruction service using the BREAST-Q patient reported outcomes measure: a cohort study. J Plast Reconstr Aesthet Surg 69:1469–1477
Lee BT, Agarwal JP, Ascherman JA et al (2017) Evidence-based clinical practice guideline: autologous breast reconstruction with DIEP or pedicled TRAM abdominal flaps. Plast Reconstr Surg 140:651e–664e
Jeong W, Lee S, Kim J (2018) Meta-analysis of flap perfusion and donor site complications for breast reconstruction using pedicled versus free TRAM and DIEP flaps. Breast 38:45–51
Browne JP, Jeevan R, Gulliver-Clarke C, Pereira J, Caddy CM, van der Meulen JHP (2017) The association between complications and quality of life after mastectomy and breast reconstruction for breast cancer. Cancer 123:3460–3467
Klassen AF, Pusic AL, Scott A, Klok J, Cano SJ (2009) Satisfaction and quality of life in women who undergo breast surgery: a qualitative study. BMC Womens Health 9:11
Pusic AL, Chen CM, Cano S, Klassen A, McCarthy C, Collins ED, Cordeiro PG (2007) Measuring quality of life in cosmetic and reconstructive breast surgery: a systematic review of patient-reported outcomes instruments. Plast Reconstr Surg 120:823–837
Pusic AL et al (2006) Measuring quality of life in breast surgery: content development of a new modular system to capture patient-reported outcomes (the MSKCC Breast-Q). ISOQOL Annual Meeting 2006
Cano SJ, Klassen A, Pusic AL (2009) The science behind quality-of-life measurement: a primer for plastic surgeons. Plast Reconstr Surg 123:98e–106e
Colakoglu S, Khansa I, Curtis MS, Yueh JH, Ogunleye A, Haewyon C, Tobias AM, Lee BT (2011) Impact of complications on patient satisfaction in breast reconstruction. Plast Reconstr Surg 127:1428–1436
Spiegel AJ, Eldor L (2010) SIEA flap breast reconstruction. In: Hall-Findlay EJ, Evans GRD (eds) Aesthetic and reconstructive surgery of the breast. Saunders Elsevier, pp 147–159
Alderman AK, Wilkins EG, Kim HM, Lowery JC (2002) Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg 109:2265–2274
Ng SK, Hare RM, Kuang RJ, Smith KM, Brown BJ, Hunter-Smith DJ (2016) Breast reconstruction post mastectomy: patient satisfaction and decision making. Ann Plast Surg 76:640–644
Cohen WA, Mundy LR, Ballard TN, Klassen A, Cano SJ, Browne J, Pusic AL (2016) The BREAST-Q in surgical research: a review of the literature 2009-2015. J Plast Reconstr Aesthet Surg 69:149–162
Mundy LR, Homa K, Klassen AF, Pusic AL, Kerrigan CL (2017) Breast cancer and reconstruction: normative data for interpreting the BREAST-Q. Plast Reconstr Surg 139:1046e–1055e
Liu LQ, Branford OA, Mehigan S (2018) BREAST-Q measurement of the patient perspective in oncoplastic breast surgery: a systematic review. Plast Reconstr Surg Glob Open 6:e1904
Toyserkani NM, Jørgensen MG, Tabatabaeifar S, Damsgaard T, Sørensen JA (2020) Autologous versus implant-based breast reconstruction: a systematic review and meta-analysis of Breast-Q patient-reported outcomes. J Plast Reconstr Aesthet Surg 73:278–285
Zhong T, Hu J, Bagher S, Vo A, OʼNeill AC, Butler K, Novak CB, Hofer SO, Metcalfe KA (2016) A comparison of psychological response, body image, sexuality, and quality of life between immediate and delayed autologous tissue breast reconstruction: a prospective long-term outcome study. Plast Reconstr Surg 138:772–780
Eltahir Y, Werners LL, Dreise MM, Zeijlmans van Emmichoven IA, Werker PM, de Bock GH (2015) Which breast is the best? Successful autologous or alloplastic breast reconstruction: patient-reported quality-of-life outcomes. Plast Reconstr Surg 135:43–50
Santosa KB, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG (2016) Effect of patient age on outcomes in breast reconstruction: results from a multicenter prospective study. J Am Coll Surg 223:745–754
Pirro O, Mestak O, Vindigni V, Sukop A, Hromadkova V, Nguyenova A, Vitova L, Bassetto F (2017) Comparison of patient-reported outcomes after implant versus autologous tissue breast reconstruction using the BREAST-Q. Plast Reconstr Surg Glob Open 5:e1217
Nelson JA, Allen RJ Jr, Polanco T et al (2019) Long-term patient-reported outcomes following postmastectomy breast reconstruction: an 8-year examination of 3268 patients. Ann Surg 270:473–483
Murphy BD, Kerrebijn I, Farhadi J, Masia J, Hofer SOP (2018) Indications and controversies for abdominally-based complete autologous tissue breast reconstruction. Clin Plast Surg 45:83–91
Benditte-Klepetko HC, Lutgendorff F, Kastenbauer T, Deutinger M, van der Horst CM (2014) Analysis of patient satisfaction and donor-site morbidity after different types of breast reconstruction. Scand J Surg 103:249–255
Barone M, Cogliandro A, Signoretti M, Persichetti P (2018) Analysis of symmetry stability following implant-based breast reconstruction and contralateral management in 582 patients with long-term outcomes. Aesthet Plast Surg 42:936–940
Andrade WN, Baxter N, Semple JL (2001) Clinical determinants of patient satisfaction with breast reconstruction. Plast Reconstr Surg 107:46–54
Wilkins EG, Hamill JB, Kim HM, Kim JY, Greco RJ, Qi J, Pusic AL (2018) Complications in postmastectomy breast reconstruction: one-year outcomes of the Mastectomy Reconstruction Outcomes Consortium (MROC) Study. Ann Surg 267:164–170
Bennett KG, Qi J, Kim HM, Hamill JB, Pusic AL, Wilkins EG (2018) Comparison of 2-year complication rates among common techniques for postmastectomy breast reconstruction. JAMA Surg 153:901–908
Sanati-Mehrizy P, Massenburg BB, Rozehnal JM, Gupta N, Rosa JH, Ingargiola MJ, Taub PJ (2015) A comparison of postoperative outcomes in immediate versus delayed reconstruction after mastectomy. Eplasty 15:e44
Beugels J, Kool M, Hoekstra LT, Heuts EM, Tuinder SMH, van der Hulst RRWJ, Piatkowski A (2018) Quality of life of patients after immediate or delayed autologous breast reconstruction: a multicenter study. Ann Plast Surg 81:523–527
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethics approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Portuguese Institute of Oncology - Porto.
Informed consent
Informed consent was obtained from individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Brito, Í.M., Fernandes, A., Andresen, C. et al. Patient satisfaction with breast reconstruction: how much do timing and surgical technique matter?. Eur J Plast Surg 43, 809–818 (2020). https://doi.org/10.1007/s00238-020-01663-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-020-01663-7