Abstract
Purpose
Posterior circulation ischemic stroke (PCIS) possesses unique features. However, previous studies have primarily or exclusively relied on anterior circulation stroke cases to build machine learning (ML) models for predicting onset time. To date, there is no research reporting the effectiveness and stability of ML in identifying PCIS onset time. We aimed to build diffusion-weighted imaging-based ML models to identify the onset time of PCIS patients.
Methods
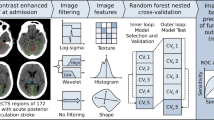
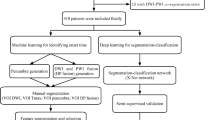
Consecutive PCIS patients within 24 h of definite symptom onset were included (112 in the training set and 49 in the independent test set). Images were processed as follows: volume of interest segmentation, image feature extraction, and feature selection. Five ML models, naïve Bayes, logistic regression, tree ensemble, k-nearest neighbor, and random forest, were built based on the training set to estimate the stroke onset time (binary classification: ≤ 4.5 h or > 4.5 h). Relative standard deviations (RSD), receiver operating characteristic (ROC) curves, and the calibration plot was performed to evaluate the stability and performance of the five models.
Results
The random forest model had the best performance in the test set, with the highest area under the curve (AUC, 0.840; 95% CI: 0.706, 0.974). This model also achieved the highest accuracy, sensitivity, specificity, positive predictive value, and negative predictive value (83.7%, 64.3%, 91.4%, 75.0%, and 86.5%, respectively). Furthermore, the model had high stability (RSD = 0.0094).
Conclusion
The PCIS case-based ML model was effective for estimating the symptom onset time and achieved considerably high specificity and stability.





Similar content being viewed by others
Data availability
Data reported in this study are available upon reasonable request to the corresponding author.
Abbreviations
- ADC:
-
Apparent diffusion coefficient
- AIS:
-
Acute ischemic stroke
- AUC:
-
Area under the curve
- CTP:
-
CT perfusion imaging
- DWI:
-
Diffusion-weighted imaging
- FLAIR:
-
Fluid-attenuated inversion recovery
- KNN:
-
K-nearest neighbor
- LR:
-
Logistic regression
- ML:
-
Machine learning
- NB:
-
Naïve Bayes
- NIHSS:
-
National Institutes of Health Stroke Scale
- NPV:
-
Negative predictive value
- PCIS:
-
Posterior circulation ischemic stroke
- PDM:
-
PWI-DWI mismatch
- PPV:
-
Positive predictive value
- PWI:
-
Perfusion-weighted imaging
- RF:
-
Random forest
- ROC:
-
Receiver operating characteristic
- RSD:
-
Relative standard deviation
- TE:
-
Tree ensemble
- TSS:
-
Time-since-stroke
References
Sparaco M, Ciolli L, Zini A (2019) Posterior circulation ischaemic stroke-a review part I: anatomy, aetiology and clinical presentations. Neurol Sci : Off J Ital Neurol Soc Ital Soc Clin Neurophysiol 40:1995–2006. https://doi.org/10.1007/s10072-019-03977-2
Sparaco M, Ciolli L, Zini A (2019) Posterior circulation ischemic stroke-a review part II: imaging and acute treatment. Neurol Sci : Off J Ital Neurol Soc Ital Soc Clin Neurophysio 40:2007–2015. https://doi.org/10.1007/s10072-019-03936-x
Berge E, Whiteley W, Audebert H, et al (2021) European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. European stroke journal 6:I-lxii. https://doi.org/10.1177/2396987321989865
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 50:e344–e418. https://doi.org/10.1161/str.0000000000000211
Bluhmki E, Chamorro A, Dávalos A, Machnig T, Sauce C, Wahlgren N, Wardlaw J, Hacke W (2009) Stroke treatment with alteplase given 3.0-4.5 h after onset of acute ischaemic stroke (ECASS III): additional outcomes and subgroup analysis of a randomised controlled trial. Lancet Neurol 8:1095–1102. https://doi.org/10.1016/s1474-4422(09)70264-9
Serena J, Dávalos A, Segura T, Mostacero E, Castillo J (2003) Stroke on awakening: looking for a more rational management. Cerebrovasc Dis (Basel Switzerland) 16:128–133. https://doi.org/10.1159/000070592
Mackey J, Kleindorfer D, Sucharew H et al (2011) Population-based study of wake-up strokes. Neurology 76:1662–1667. https://doi.org/10.1212/WNL.0b013e318219fb30
Rimmele DL, Thomalla G (2014) Wake-up stroke: clinical characteristics, imaging findings, and treatment option - an update. Front Neurol 5:35. https://doi.org/10.3389/fneur.2014.00035
Lee H, Lee EJ, Ham S, Lee HB, Lee JS, Kwon SU, Kim JS, Kim N, Kang DW (2020) Machine Learning Approach to Identify Stroke Within 4.5 Hours. Stroke 51:860–866. https://doi.org/10.1161/strokeaha.119.027611
Jiang L, Wang S, Ai Z, Shen T, Zhang H, Duan S, Chen YC, Yin X, Sun J (2022) Development and external validation of a stability machine learning model to identify wake-up stroke onset time from MRI. Eur Radiol 32:3661–3669. https://doi.org/10.1007/s00330-021-08493-6
Zhu H, Jiang L, Zhang H, Luo L, Chen Y, Chen Y (2021) An automatic machine learning approach for ischemic stroke onset time identification based on DWI and FLAIR imaging. NeuroImage Clin 31:102744. https://doi.org/10.1016/j.nicl.2021.102744
Ho KC, Speier W, Zhang H, Scalzo F, El-Saden S, Arnold CW (2019) A machine learning approach for classifying ischemic stroke onset time from imaging. IEEE Trans Med Imaging 38:1666–1676. https://doi.org/10.1109/tmi.2019.2901445
Zhang H, Polson JS, Nael K, Salamon N, Yoo B, El-Saden S, Scalzo F, Speier W, Arnold CW (2021) Intra-domain task-adaptive transfer learning to determine acute ischemic stroke onset time. Comput Med Imaging Graphics : Off J Comput Med Imaging Soc 90:101926. https://doi.org/10.1016/j.compmedimag.2021.101926
Kim K, Kim BJ, Huh J et al (2021) Delayed lesions on diffusion-weighted imaging in initially lesion-negative stroke patients. J Stroke 23:69–81. https://doi.org/10.5853/jos.2020.02110
Lindsberg PJ, Pekkola J, Strbian D, Sairanen T, Mattle HP, Schroth G (2015) Time window for recanalization in basilar artery occlusion: speculative synthesis. Neurology 85:1806–1815. https://doi.org/10.1212/wnl.0000000000002129
Adams HP Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, Marsh EE 3rd (1993) Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke 24:35–41. https://doi.org/10.1161/01.str.24.1.35
Bader-El-Den M, Teitei E, Perry T (2019) Biased random forest for dealing with the class imbalance problem. IEEE Trans Neural Netw Learn Syst 30:2163–2172. https://doi.org/10.1109/tnnls.2018.2878400
Blagus R, Lusa L (2013) SMOTE for high-dimensional class-imbalanced data. BMC Bioinformatics 14:106. https://doi.org/10.1186/1471-2105-14-106
Breiman L (2001) Random Forests. Mach Learn 45:5–32. https://doi.org/10.1023/A:1010933404324
Thomalla G, Cheng B, Ebinger M et al (2011) DWI-FLAIR mismatch for the identification of patients with acute ischaemic stroke within 4·5 h of symptom onset (PRE-FLAIR): a multicentre observational study. Lancet Neurol 10:978–986. https://doi.org/10.1016/s1474-4422(11)70192-2
Markus HS, Michel P (2022) Treatment of posterior circulation stroke: acute management and secondary prevention. Int J Stroke : Off J Int Stroke Soc 17:723–732. https://doi.org/10.1177/17474930221107500
Keselman B, Gdovinová Z, Jatuzis D et al (2020) Safety and outcomes of intravenous thrombolysis in posterior versus anterior circulation stroke: results from the safe implementation of treatments in stroke registry and meta-analysis. Stroke 51:876–882. https://doi.org/10.1161/strokeaha.119.027071
Tong X, Liao X, Pan Y et al (2016) Intravenous thrombolysis is more safe and effective for posterior circulation stroke: data from the Thrombolysis Implementation and Monitor of Acute Ischemic Stroke in China (TIMS-China). Medicine 95:e3848. https://doi.org/10.1097/md.0000000000003848
Huang Q, Song HQ, Ma QF, Song XW, Wu J (2019) Effects of time delays on the therapeutic outcomes of intravenous thrombolysis for acute ischemic stroke in the posterior circulation: an observational study. Brain Behav 9:e01189. https://doi.org/10.1002/brb3.1189
Cortijo E, García-Bermejo P, Calleja AI, Pérez-Fernández S, Gómez R, del Monte JM, Reyes J, Arenillas JF (2014) Intravenous thrombolysis in ischemic stroke with unknown onset using CT perfusion. Acta Neurol Scand 129:178–183. https://doi.org/10.1111/ane.12160
Morelli N, Rota E, Iafelice I, Petracca F, Magnacavallo A, Michieletti E, Guidetti D (2014) Parenchyma, pipes, perfusion and penumbra imaging: the multimodal CT in wake-up stroke basilar thrombosis. Eur Neurol 71:155–156. https://doi.org/10.1159/000355469
Hill MD, Kenney C, Dzialowski I, Boulanger JM, Demchuk AM, Barber PA, Watson TW, Weir NU, Buchan AM (2013) Tissue Window in Stroke Thrombolysis study (TWIST): a safety study. Can J Neurol Sci Le J Can Des Sci Neurol 40:17–20. https://doi.org/10.1017/s0317167100012890
Parsons MW, Pepper EM, Chan V, Siddique S, Rajaratnam S, Bateman GA, Levi CR (2005) Perfusion computed tomography: prediction of final infarct extent and stroke outcome. Ann Neurol 58:672–679. https://doi.org/10.1002/ana.20638
Campbell BCV, Majoie C, Albers GW et al (2019) Penumbral imaging and functional outcome in patients with anterior circulation ischaemic stroke treated with endovascular thrombectomy versus medical therapy: a meta-analysis of individual patient-level data. Lancet Neurol 18:46–55. https://doi.org/10.1016/s1474-4422(18)30314-4
Zhang YL, Zhang JF, Wang XX, Wang Y, Anderson CS, Wu YC (2021) Wake-up stroke: imaging-based diagnosis and recanalization therapy. J Neurol 268:4002–4012. https://doi.org/10.1007/s00415-020-10055-7
Huisa BN, Liebeskind DS, Raman R, Hao Q, Meyer BC, Meyer DM, Hemmen TM (2013) Diffusion-weighted imaging-fluid attenuated inversion recovery mismatch in nocturnal stroke patients with unknown time of onset. J Stroke Cerebrovasc Dis : Off J Natl Stroke Assoc 22:972–977. https://doi.org/10.1016/j.jstrokecerebrovasdis.2012.01.004
Odland A, Særvoll P, Advani R, Kurz MW, Kurz KD (2015) Are the current MRI criteria using the DWI-FLAIR mismatch concept for selection of patients with wake-up stroke to thrombolysis excluding too many patients? Scand J Trauma Resuscitation Emerg Med 23:22. https://doi.org/10.1186/s13049-015-0101-7
Keshari R, Vatsa M, Singh R, Noore A (2018) Learning structure and strength of CNN filters for small sample size training. In: 2018 IEEE/CVF Conf Comput Vis Pattern Recognition 9349–9358. https://doi.org/10.1109/CVPR.2018.00974
Acknowledgements
We thank Dawei Yang, MD, for his suggestions on the Discussion section. We express our gratitude for the support provided by the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZYLX202101).
Funding
This study was funded by the Beijing Municipal Administration of Hospitals Clinical Medicine Development of Special Funding Support (ZYLX202101).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This retrospective study was approved by our Institutional Review Board (number 2021–014).
Informed consent
The informed consent requirement was waived by the Ethics Committee due to the retrospective nature of the study.
Competing interests
Zhenghan Yang reports funds from the Beijing Municipal Administration of Hospitals. The other authors have no relevant financial or non-financial interests to disclose.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Zhenhao Liu and Shiyu Zhang are co-first authors
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Liu, Z., Zhang, S., Wang, Y. et al. Posterior circulation ischemic stroke: radiomics-based machine learning approach to identify onset time from magnetic resonance imaging. Neuroradiology (2024). https://doi.org/10.1007/s00234-024-03353-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00234-024-03353-8