Abstract
Purpose
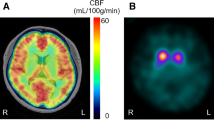
Corticobasal syndrome (CBS) and Parkinson’s disease (PD) both present with asymmetrical extrapyramidal symptoms, often leading to a diagnostic dilemma. Patients with CBS frequently show cerebral blood flow (CBF) asymmetry alongside asymmetrical cortical atrophy. This study aimed to evaluate the clinical utility of arterial spin labeling (ASL) magnetic resonance imaging (MRI) to detect CBF asymmetry in patients with CBS.
Methods
We retrospectively investigated asymmetries of regional CBF and cortical volume, measured using ASL and T1-weighted MRI, in 13 patients with CBS and 22 age-matched patients with PD. Regional CBF and cortical volume values were derived from nine brain regions on each side. CBF and volume asymmetries were calculated as %difference in each region, respectively.
Results
CBF asymmetry showed significantly greater differences in seven of nine regions, such as the perirolandic area (− 8.7% vs. − 1.4%, p < 0.001) and parietal cortex (− 9.7% vs. − 1.3%, p < 0.001) in patients with CBS compared with patients with PD. In contrast, significant differences in volume asymmetry were observed in three regions included within the seven regions showing CBF asymmetry, which indicated that CBF asymmetry has greater sensitivity than volume asymmetry to detect asymmetricity in CBS.
Conclusion
ASL imaging showed significant CBF asymmetry in a wider range of brain regions in patients with CBS, which suggests that noninvasive MRI with ASL imaging is a promising tool for the diagnosis of CBS, with advantages that include the simultaneous evaluation of asymmetrical hypoperfusion in addition to focal atrophy.




Similar content being viewed by others
Data availability
Data is available on reasonable request.
Code availability
Not applicable.
References
Dickson DW, Bergeron C, Chin SS et al (2002) Office of Rare Diseases neuropathologic criteria for corticobasal degeneration. J Neuropathol Exp Neurol 61:935–946. https://doi.org/10.1093/jnen/61.11.935
Boeve BF, Maraganore DM, Parisi JE et al (1999) Pathologic heterogeneity in clinically diagnosed corticobasal degeneration. Neurology 53:795–800. https://doi.org/10.1212/wnl.53.4.795
Armstrong MJ, Litvan I, Lang AE et al (2013) Criteria for the diagnosis of corticobasal degeneration. Neurology 80:496–503. https://doi.org/10.1212/WNL.0b013e31827f0fd1
Mathew R, Bak TH, Hodges JR (2012) Diagnostic criteria for corticobasal syndrome: a comparative study. J Neurol Neurosurg Psychiatry 83:405–410. https://doi.org/10.1136/jnnp-2011-300875
Cubo E, Martín PM, Martin-Gonzalez JA et al (2010) Motor laterality asymmetry and nonmotor symptoms in Parkinson’s disease. Mov Disord 25:70–75. https://doi.org/10.1002/mds.22896
Djaldetti R, Ziv I, Melamed E (2006) The mystery of motor asymmetry in Parkinson’s disease. Lancet Neurol 9:796–802. https://doi.org/10.1016/S1474-4422(06)70549-X
Kitagaki H, Hirono N, Ishii K, Mori E (2000) Corticobasal degeneration: evaluation of cortical atrophy by means of hemispheric surface display generated with MR images. Radiology 216:31–38. https://doi.org/10.1148/radiology.216.1.r00ma0531
Soliveri P, Monza D, Paridi D et al (1999) Cognitive and magnetic resonance imaging aspects of corticobasal degeneration and progressive supranuclear palsy. Neurology 53:502–507. https://doi.org/10.1212/wnl.53.3.502
Di Stasio F, Suppa A, Marsili L et al (2019) Corticobasal syndrome: neuroimaging and neurophysiological advances. Eur J Neurol 26:701-e52. https://doi.org/10.1111/ene.13928
Takaya S, Sawamoto N, Okada T et al (2018) Differential diagnosis of parkinsonian syndromes using dopamine transporter and perfusion SPECT. Parkinsonism Relat Disord 47:15–21. https://doi.org/10.1016/j.parkreldis.2017.11.333
Hossain AK, Murata Y, Zhang L et al (2003) Brain perfusion SPECT in patients with corticobasal degeneration: analysis using statistical parametric mapping. Mov Disord 18:697–703. https://doi.org/10.1002/mds.10415
Okuda B, Tachibana H, Kawabata K et al (1999) Cerebral blood flow correlates of higher brain dysfunctions in corticobasal degeneration. J Geriatr Psychiatry Neurol 12:189–193. https://doi.org/10.1177/089198879901200404
Okuda B, Tachibana H, Kawabata K et al (2001) Comparison of brain perfusion in corticobasal degeneration and Alzheimer’s disease. Dement Geriatr Cogn Disord 12:226–231. https://doi.org/10.1159/000051262
Mille E, Levin J, Brendel M et al (2017) Cerebral glucose metabolism and dopaminergic function in patients with corticobasal syndrome. J Neuroimaging 27:255–261. https://doi.org/10.1111/jon.12391
Niethammer M, Tang CC, Feigin A et al (2014) A disease-specific metabolic brain network associated with corticobasal degeneration. Brain 137:3036–3046. https://doi.org/10.1093/brain/awu256
Pardini M, Huey ED, Spina S et al (2019) FDG-PET patterns associated with underlying pathology in corticobasal syndrome. Neurology 92:e1121–e1135. https://doi.org/10.1212/WNL.0000000000007038
Markus HS, Lees AJ, Lennox G et al (1995) Patterns of regional cerebral blood flow in corticobasal degeneration studied using HMPAO SPECT; comparison with Parkinson’s disease and normal controls. Mov Disord 10:179–187. https://doi.org/10.1002/mds.870100208
Zhang L, Murata Y, Ishida R et al (2001) Differentiating between progressive supranuclear palsy and corticobasal degeneration by brain perfusion SPET. Nucl Med Commun 22:767–772. https://doi.org/10.1097/00006231-200107000-00007
Kimura H, Kado H, Koshimoto Y et al (2005) Multislice continuous arterial spin-labeled perfusion MRI in patients with chronic occlusive cerebrovascular disease: a correlative study with CO2 PET validation. J Magn Reson Imaging 22:189–198. https://doi.org/10.1002/jmri.20382
Detre JA, Rao H, Wang DJ et al (2012) Applications of arterial spin labeled MRI in the brain. J Magn Reson Imaging 35:1026–1037. https://doi.org/10.1002/jmri.23581
Melzer TR, Watts R, MacAskill MR et al (2011) Arterial spin labelling reveals an abnormal cerebral perfusion pattern in Parkinson’s disease. Brain 134:845–855. https://doi.org/10.1093/brain/awq377
Ikawa M, Kimura H, Kitazaki Y et al (2018) Arterial spin labeling MR imaging for the clinical detection of cerebellar hypoperfusion in patients with spinocerebellar degeneration. J Neurol Sci 394:58–62. https://doi.org/10.1016/j.jns.2018.09.007
Ikawa M, Yoneda M, Muramatsu T et al (2013) Detection of preclinically latent hyperperfusion due to stroke-like episodes by arterial spin-labeling perfusion MRI in MELAS patients. Mitochondrion 13:676–680. https://doi.org/10.1016/j.mito.2013.09.007
Dashjamts T, Yoshiura T, Hiwatashi A et al (2010) Asymmetrical cerebral perfusion demonstrated by noninvasive arterial spin-labeling perfusion imaging in a patient with corticobasal degeneration. Jpn J Radiol 28:75–78. https://doi.org/10.1007/s11604-009-0382-8
Tomlinson CL, Stowe R, Patel S et al (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25:2649–2653. https://doi.org/10.1002/mds.23429
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184. https://doi.org/10.1136/jnnp.55.3.181
Dai W, Garcia D, de Bazelaire C, Alsop DC (2008) Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med 60:1488–97. https://doi.org/10.1002/mrm.21790
Hammers A, Allom R, Koepp MJ et al (2003) Three-dimensional maximum probability atlas of the human brain, with particular reference to the temporal lobe. Hum Brain Mapp 19:224–247. https://doi.org/10.1002/hbm.10123
Gousias IS, Rueckert D, Heckemann RA et al (2008) Automatic segmentation of brain MRIs of 2-year-olds into 83 regions of interest. Neuroimage 40:672–684. https://doi.org/10.1016/j.neuroimage.2007.11.034
Chen S, Guan M, Lian HJ et al (2014) Crossed cerebellar diaschisis detected by arterial spin-labeled perfusion magnetic resonance imaging in subacute ischemic stroke. J Stroke Cerebrovasc Dis 23:2378–2383. https://doi.org/10.1016/j.jstrokecerebrovasdis.2014.05.009
Hauser RA, Murtaugh FR, Akhter K et al (1996) Magnetic resonance imaging of corticobasal degeneration. J Neuroimaging 6:222–226. https://doi.org/10.1111/jon199664222
Upadhyay N, Suppa A, Piattella MC et al (2016) Gray and white matter structural changes in corticobasal syndrome. Neurobiol Aging 37:82–90. https://doi.org/10.1016/j.neurobiolaging.2015.10.011
Gröschel K, Hauser TK, Luft A et al (2004) Magnetic resonance imaging-based volumetry differentiates progressive supranuclear palsy from corticobasal degeneration. Neuroimage 21:714–724. https://doi.org/10.1016/j.neuroimage.2003.09.070
Funding
This study was supported in part by Grant-in-Aid for Scientific Research (C) Grant Number 20K07900 from the Japan Society for the Promotion of Science (JSPS KAKENHI) (to M.I.).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Research Ethics Committee of the University of Fukui (20170130).
Consent to participate
This retrospective case–control study was approved by the Research Ethics Committee of the University of Fukui (20170130) with a waiver of the requirement for patients’ informed consent.
Consent to publication
Not applicable.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Yamaguchi, T., Ikawa, M., Enomoto, S. et al. Arterial spin labeling imaging for the detection of cerebral blood flow asymmetry in patients with corticobasal syndrome. Neuroradiology 64, 1829–1837 (2022). https://doi.org/10.1007/s00234-022-02942-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-02942-9