Abstract
Purpose
Τhe study examined changes in hemodynamics and functional connectivity in patients with systemic lupus erythematosus (SLE) with or without neuropsychiatric manifestations.
Methods
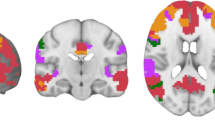
Participants were 44 patients with neuropsychiatric SLE (NPSLE), 20 SLE patients without such manifestations (non-NPSLE), and 35 healthy controls. Resting-state functional MRI (rs-fMRI) was used to obtain whole-brain maps of (a) perfusion dynamics derived through time shift analysis (TSA), (b) regional functional connectivity (intrinsic connectivity contrast (ICC) coefficients), and (c) hemodynamic-connectivity coupling. Group differences were assessed through independent samples t-tests, and correlations of rs-fMRI indices with clinical variables and neuropsychological test scores were, also, computed.
Results
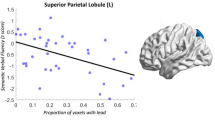
Compared to HC, NPSLE patients demonstrated intrinsic hypoconnectivity of anterior Default Mode Network (DMN) and hyperconnectivity of posterior DMN components. These changes were paralleled by elevated hemodynamic lag. In NPSLE, cognitive performance was positively related to higher intrinsic connectivity in these regions, and to higher connectivity-hemodynamic coupling in posterior DMN components. Uncoupling between hemodynamics and connectivity in the posterior DMN was associated with worse task performance. Non-NPSLE patients displayed hyperconnectivity in posterior DMN and sensorimotor regions paralleled by relatively increased hemodynamic lag.
Conclusion
Adaptation of regional brain function to hemodynamic changes in NPSLE may involve locally decreased or locally increased intrinsic connectivity (which can be beneficial for cognitive function). This process may also involve elevated coupling of hemodynamics with functional connectivity (beneficial for cognitive performance) or uncoupling, which may be detrimental for the cognitive skills of NPSLE patients.



Similar content being viewed by others
Data availability
The computed metrics derived from resting state fMRI recordings will be available upon request.
References
Bertsias GK, Boumpas DT (2010) Pathogenesis, diagnosis and management of neuropsychiatric SLE manifestations. Nat Rev Rheumatol 6:358–367
Ainiala H, Loukkola J, Peltola J, Abady M, Shoenfeld Y, Zandman-Goddard G (2001) The prevalence of neuropsychiatric syndromes in systemic lupus erythematosus. Neurology. 57:496–500
Cohen D, Rijnink EC, Nabuurs RJA et al (2017) Brain histopathology in patients with systemic lupus erythematosus: identification of lesions associated with clinical neuropsychiatric lupus syndromes and the role of complement. Rheumatology 56:77–86
Emmer BJ, van Osch MJ, Wu O et al (2010) Perfusion MRI in neuropsychiatric systemic lupus erythemathosus. J Magn Reson Imaging 32:283–288
Zimny A, Szmyrka-Kaczmarek M, Szewczyk P et al (2014) In vivo evaluation of brain damage in the course of systemic lupus erythematosus using magnetic resonance spectroscopy, perfusion weighted and diffusion-tensor imaging. Lupus 23:10–19
Papadaki E, Fanouriakis A, Kavroulakis E et al (2018) Neuropsychiatric lupus or not? Cerebral hypoperfusion by perfusion-weighted MRI in normal-appearing white matter in primary neuropsychiatric lupus erythematosus. Ann Rheum Dis 77:441–448
Wang PI, Cagnoli PC, McCune WJ et al (2012) Perfusion-weighted MR imaging in cerebral lupus erythematosus. Acad Radiol 19:965–970
Gasparovic CM, Roldan CA, Sibbitt WL et al (2010) Elevated cerebral blood flow and volume in systemic lupus measured by dynamic susceptibility contrast magnetic resonance imaging. J Rheumatol 37:1834–1843
Jia J, Xie J, Li H et al (2019) Cerebral blood flow abnormalities in neuropsychiatric systemic lupus erythematosus. Lupus. 28(9):1128–1133. https://doi.org/10.1177/0961203319861677
Zhuo Z, Su L, Duan Y et al (2020) Different patterns of cerebral perfusion in SLE patients with and without neuropsychiatric manifestations. Hum Brain Mapp 41(3):755–766. https://doi.org/10.1002/hbm.24837
Cao ZY, Wang N, Jia JT et al (2021) Abnormal topological organization in systemic lupus erythematosus: a resting-state functional magnetic resonance imaging analysis. Brain Imag Behav 15:14–24. https://doi.org/10.1007/s11682-019-00228-y
Preziosa P, Rocca MA, Ramirez GA et al (2020) Structural and functional brain connectomes in patients with systemic lupus erythematosus. Eur J Neurol 27(1):113–1e2. https://doi.org/10.1111/ene.14041
Bonacchi R, Rocca MA, Ramirez GA et al (2020) Resting state network functional connectivity abnormalities in systemic lupus erythematosus: correlations with neuropsychiatric impairment. Mol Psychiatry. https://doi.org/10.1038/s41380-020-00907-z
Simos NJ, Dimitriadis SI, Kavroulakis E et al (2020) Quantitative identification of functional connectivity disturbances in neuropsychiatric lupus based on resting-state fMRI: a robust machine learning approach. Brain Sci 10(11):777. https://doi.org/10.3390/brainsci10110777
Nystedt J, Mannfolk P, Jönsen A, Nilsson P, Strandberg TO, Sundgren PC (2019) Functional connectivity changes in core resting state networks are associated with cognitive performance in systemic lupus erythematosus. J Comp Neurol 527(11):1837–1856
Yu H, Qiu X, Zhang YQ et al (2019) Abnormal amplitude of low frequency fluctuation and functional connectivity in non-neuropsychiatric systemic lupus erythematosus: a resting-state fMRI study. Neuroradiology. 61(3):331–340
Liu S, Cheng Y, Xie Z et al (2018) A conscious resting state fMRI study in SLE patients without major neuropsychiatric manifestations. Front Psychiatry 9:677
Niu C, Tan X, Liu X et al (2018) Cortical thickness reductions associate with abnormal resting-state functional connectivity in non-neuropsychiatric systemic lupus erythematosus. Brain Imaging Behav 12(3):674–684
Nystedt J, Mannfolk P, Jönsen A et al (2018) Functional connectivity changes in systemic lupus erythematosus: a resting-state study. Brain Connect 8(4):220–234
Zhang XD, Jiang XL, Cheng Z et al (2017) Decreased coupling between functional connectivity density and amplitude of low frequency fluctuation in non-neuropsychiatric systemic lupus erythematosus: a resting-stage functional MRI study. Mol Neurobiol 54(7):5225–5235
Hou J, Lin Y, Zhang W et al (2013) Abnormalities of frontal-parietal resting-state functional connectivity are related to disease activity in patients with systemic lupus erythematosus. PLoS One 8(9):e74530. https://doi.org/10.1371/journal.pone.0074530
Khalil AA, Ostwaldt A-C, Nierhaus T et al (2017) Relationship between changes in the temporal dynamics of the blood-oxygen-level-dependent signal and hypoperfusion in acute ischemic stroke. Stroke 48:925–931
Khalil AA, Villringer K, Filleböck V et al (2020) Non-invasive monitoring of longitudinal changes in cerebral hemodynamics in acute ischemic stroke using BOLD signal delay. J Cereb Blood Flow Metab 40:23–34
Lv Y, Margulies DS, Cameron Craddock R et al (2013) Identifying the perfusion deficit in acute stroke with resting-state functional magnetic resonance imaging. Ann Neurol 73:136–140
Tong Y, Lindsey KP, Hocke LM, Vitaliano G, Mintzopoulos D, Frederick BD (2017) Perfusion information extracted from resting state functional magnetic resonance imaging. J Cereb Blood Flow Metab 37:564–576
Mitra A, Snyder AZ, Hacker CD, Raichle ME (2014) Lag structure in resting-state fMRI. J Neurophysiol 111:2374–2391
Siegel JS, Snyder AZ, Ramsey L, Shulman GL, Corbetta M (2016) The effects of hemodynamic lag on functional connectivity and behavior after stroke. J Cereb Blood Flow Metab 36(12):2162–2176
Amemiya S, Kunimatsu A, Saito N, Ohtomo K (2014) Cerebral hemodynamic impairment: assessment with resting-state functional MR imaging. Radiology. 270(2):548–555
Yan S, Qi Z, An Y, Zhang M, Qian T, Lu J (2019) Detecting perfusion deficit in Alzheimer’s disease and mild cognitive impairment patients by resting-state fMRI. J Magn Reson Imaging 49(4):1099–1104
Antypa D, Simos NJ, Kavroulakis E et al (2021) Anxiety and depression severity in neuropsychiatric SLE are associated with perfusion and functional connectivity changes of the frontolimbic neural circuit: a resting-state f(unctional) MRI study. Lupus Sci Med 8(1):e000473. https://doi.org/10.1136/lupus-2020-000473
Hochberg MC (1997) Updating the American College of Rheumatology revised criteria for the classification of systemic lupus erythematosus. Arthritis Rheum 40(9):1725–1725
Gladman DD, Ibañez D, Urowitz MB (2002) Systemic lupus erythematosus disease activity index 2000. J Rheumatol 29:288–291
Gladman DD, Goldsmith CH, Urowitz MB et al (2000) The Systemic Lupus International Collaborating Clinics/American College of Rheumatology (SLICC/ACR) damage index for systemic lupus erythematosus international comparison. J Rheumatol 27:373–376
(1999) The American College of Rheumatology nomenclature and case definitions for neuropsychiatric lupus syndromes. Arthritis Rheum 42:599–608
Whitefield-Gabrieli S, Nieto-Castanon A (2012 Jun) Conn: a functional connectivity toolbox for correlated and anticorrelated brain networks. Brain Connectivity 2(3):125–141
Layden E. Intrinsic_connectivity_contrast [Internet]. MATLAB Central File Exchange. 2020 [cited 2020 Apr 2]. Available from: https://ch.mathworks.com/matlabcentral/fileexchange/68248-intrinsic_connectivity_contrast
Slotnick SD (2017) Cluster success: fMRI inferences for spatial extent have acceptable false-positive rates. Cogn Neurosci 8:150–155
Slotnick SD, Moo LR, Segal JB, Hart J Jr (2003) Distinct prefrontal cortex activity associated with item memory and source memory for visual shapes. Brain Res Cogn Brain Res 17:75–82
Wiseman SJ, Bastin ME, Jardine CL et al (2016) Cerebral small vessel disease burden is increased in systemic lupus erythematosus. Stroke 47:2722–2728
Barraclough M, McKie S, Parker B et al (2019) Altered cognitive function in systemic lupus erythematosus and associations with inflammation and functional and structural brain changes. Ann Rheum Dis 78(7):934–940
Mikdashi JA (2016) Altered functional neuronal activity in neuropsychiatric lupus: a systematic review of the fMRI investigations. Semin Arthritis Rheum 45(4):455–462
Funding
Financial support for this work was provided by the Hellenic Foundation for Research and Innovation (H.F.R.I.) under the “2nd Call for H.F.R.I. Research Projects to support Post-Doctoral Researchers” (Project Number: 1220).
Author information
Authors and Affiliations
Contributions
Conceptualization: Efrosini Papadaki; Nicholas Simos
Methodology: Efrosini Papadaki; Nicholas Simos; Eleftherios Kavroulakis
Formal analysis and investigation: Nicholas Simos; Eleftherios Kavroulakis
Writing — original draft preparation: Efrosini Papadaki; Despina Antypa; Nicholas Simos
Writing — review and editing: Efrosini Papadaki; George Bertsias; Thomas Maris; Dimitrios Boumpas
Funding acquisition: Eleftherios Kavroulakis
Resources: George Bertsias; Antonis Fanouriakis; Prodromos Sidiropoulos
Supervision: Efrosini Papadaki; Dimitrios Boumpas
Corresponding author
Ethics declarations
Competing interests
The authors have no competing interests to declare that are relevant to the content of this article.
Ethical approval
The hospital review board approved this study and the procedure was thoroughly explained to all patients and volunteers who signed informed consent.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Papadaki, E., Simos, N.J., Kavroulakis, E. et al. Converging evidence of impaired brain function in systemic lupus erythematosus: changes in perfusion dynamics and intrinsic functional connectivity. Neuroradiology 64, 1593–1604 (2022). https://doi.org/10.1007/s00234-022-02924-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-02924-x