Abstract
Purpose
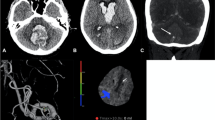
Delayed cerebral ischemia (DCI) remains a contributor to poor outcome following aneurysmal subarachnoid hemorrhage (aSAH). We evaluated cerebral circulation time (CCT) on digital subtraction angiography (DSA) during endovascular treatment (EVT) in WFNS grade I aSAH patients as a predictor of DCI.
Methods
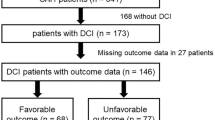
Of 135 consecutive WNFS grade I aSAH patients, 90 were included. Age, gender, time of DSA from ictus (< 72 h or > 72 h), Fisher scale, severe vasospasm, development of DCI, EVD-dependent hydrocephalus, re-bleeding, and procedural complications were recorded. CCT was calculated retrospectively from multiphase DSA. Association with DCI was established through univariate and, subsequently, multivariable logistic regression. An optimal threshold value was identified using ROC curve analysis. Patient groups defined by threshold CCT value, DCI, and, subsequently, time of DSA from ictus were analyzed using χ2 and Fisher’s exact test.
Results
CCT was the only significant factor in the multivariable logistic regression for the outcome development of DCI (OR/second increase in CCT = 1.46 [95% CI 1.14–1.86, p = .003]). When CCT was dichotomized at 8.5 s, the odds ratio for developing DCI was 7.12 (95% CI 1.93–26.34, p = .003) for CCT > 8.5 s compared with < 8.5 s. There was a significant difference for DCI in all patient groups dichotomized by CCT < 8.5 s and > 8.5 s (all patients, p = .001; patients imaged before and after 72 h of ictus, p = .024 and p = .034, respectively).
Conclusion
A CCT > 8.5 s on DSA during EVT in WFNS grade I aSAH patients is associated with an increased risk of developing DCI and may aid in the management of high-risk patients.



Similar content being viewed by others
Data availability
Data are available upon reasonable request from Dr. René van den Berg; r.vdberg@amsterdamumc.nl.
References
Rabinstein AA, Friedman JA, Weigand SD et al (2004) Predictors of cerebral infarction in aneurysmal subarachnoid hemorrhage. Stroke 35:1862–1866
Budohoski KP, Guilfoyle M, Helmy A et al (2014) The pathophysiology and treatment of delayed cerebral ischaemia following subarachnoid haemorrhage. J Neurol Neurosurg Psychiatry 85:1343–1353
Etminan N, Beseoglu K, Heiroth HJ et al (2013) Early perfusion computerized tomography imaging as a radiographic surrogate for delayed cerebral ischemia and functional outcome after subarachnoid hemorrhage. Stroke 44:1260–1266
Cremers CHP, Van Der Schaaf IC, Wensink E et al (2014) CT perfusion and delayed cerebral ischemia in aneurysmal subarachnoid hemorrhage: a systematic review and meta-analysis. J Cereb Blood Flow Metab 34:200–207
Malinova V, Dolatowski K, Schramm P et al (2016) Early whole-brain CT perfusion for detection of patients at risk for delayed cerebral ischemia after subarachnoid hemorrhage. J Neurosurg 125:128–136
Wintermark M, Ko NU, Smith WS et al (2006) Vasospasm after subarachnoid hemorrhage: utility of perfusion CT and CT angiography on diagnosis and management. Am J Neuroradiol 27:26–34
Murphy A, Lee TY, Marotta TR et al (2018) Prospective multicenter study of changes in MTT after aneurysmal SAH and relationship to delayed cerebral ischemia in patients with good- and poor-grade admission status. Am J Neuroradiol 39:2027–2033
Diringer MN, Bleck TP, Hemphill JC et al (2011) Critical care management of patients following aneurysmal subarachnoid hemorrhage: recommendations from the neurocritical care society’s multidisciplinary consensus conference. Neurocrit Care 15:211–240
Connolly ES, Rabinstein AA, Carhuapoma JR et al (2012) Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the american heart association/american stroke association. Stroke 43:1711–1737
Malinova V, Tsogkas I, Behme D et al (2020) Defining cutoff values for early prediction of delayed cerebral ischemia after subarachnoid hemorrhage by CT perfusion. Neurosurg Rev 43:581–587
GREITZ T (1956) A radiologic study of the brain circulation by rapid serial angiography of the carotid artery. Acta Radiol Suppl 1–123
Gado M, Eichling J, Grubb R et al (1975) Appraisal of the angiographic circulation time as an index of cerebral blood flow. Radiology 115:107–112
Udoetuk JD, Stiefel MF, Hurst RW et al (2007) Admission angiographic cerebral circulation time may predict subsequent angiographic vasospasm after aneurysmal subarachnoid hemorrhage. Neurosurgery 61:1152–1159
von Elm E, Altman DG, Egger M et al (2007) The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370:1453–1457
Crobeddu E, Mittal MK, Dupont S et al (2012) Predicting the lack of development of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Stroke 43:697–701
De Rooij NK, Greving JP, Rinkel GJE, Frijns CJM (2013) Early prediction of delayed cerebral ischemia after subarachnoid hemorrhage: development and validation of a practical risk chart. Stroke 44:1288–1294
De Oliveira Manoel AL, Jaja BN, Germans MR et al (2015) The VASOGRADE: a simple grading scale for prediction of delayed cerebral ischemia after subarachnoid hemorrhage. Stroke 46:1826–1831
Vergouwen MDI, Vermeulen M, van Gijn J et al (2010) Definition of delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage as an outcome event in clinical trials and observational studies: proposal of a multidisciplinary research group. Stroke 41:2391–2395
Stein SC, Browne KD, Chen XH et al (2006) Thromboembolism and delayed cerebral ischemia after subarachnoid hemorrhage: an autopsy study. Neurosurgery 59:781–787
Friedrich B, Müller F, Feiler S et al (2012) Experimental subarachnoid hemorrhage causes early and long-lasting microarterial constriction and microthrombosis: an in-vivo microscopy study. J Cereb Blood Flow Metab 32:447–455
Brawanski N, Kashefiolasl S, Won SY et al (2019) Does aneurysm side influence the infarction side and patients’ outcome after subarachnoid hemorrhage? PLoS ONE 14:1–11
Tholance Y, Barcelos GK, Perret-Liaudet A et al (2017) Placing intracerebral probes to optimise detection of delayed cerebral ischemia and allow for the prediction of patient outcome in aneurysmal subarachnoid haemorrhage. J Cereb Blood Flow Metab 37:2820–2832
Gölitz P, Hoelter P, Rösch J et al (2018) Ultra-early detection of microcirculatory injury as predictor of developing delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Clin Neuroradiol 28:501–507
Lin CF, Hsu SPC, Lin CJ et al (2016) Prolonged cerebral circulation time is the best parameter for predicting vasospasm during initial CT perfusion in subarachnoid hemorrhagic patients. PLoS ONE 11:1–13
Dankbaar JW, Rijsdijk M, Van Der Schaaf IC et al (2009) Relationship between vasospasm, cerebral perfusion, and delayed cerebral ischemia after aneurysmal subarachnoid hemorrhage. Neuroradiology 51:813–819
Kumar G, Dumitrascu OM, Chiang CC et al (2019) Prediction of delayed cerebral ischemia with cerebral angiography: a meta-analysis. Neurocrit Care 30:62–71
Hiroki O, Hiroshi M, Masahiko T, Shigeharu S (2000) Impact of cerebral microcirculatory changes on cerebral blood flow during cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke 31:1621–1627
Takahashi Y, Sasahara A, Yamazaki K et al (2017) Disturbance of CT perfusion within 24 h after onset is associated with WFNS grade but not development of DCI in patients with aneurysmal SAH. Acta Neurochir (Wien) 159:2319–2324
Slupe AM, Kirsch JR (2018) Effects of anesthesia on cerebral blood flow, metabolism, and neuroprotection. J Cereb Blood Flow Metab 38:2192–2208
Greitz T (1968) Normal cerebral circulation time as determined by carotid angiography with sodium and methylglucamine diatrizoate (urografin). Acta radiol 7:331–336
Iseda T, Nakano S, Yoneyama T et al (2000) Angiographic cerebral circulation time before and after endovascular therapy for symptomatic vasospasm. Clin Radiol 55:679–683
Milburn JM, Moran CJ, Cross DWT et al (1997) Effect of intraarterial papaverine on cerebral circulation time. Am J Neuroradiol 18:1081–1085
Minami H, Kuwamura K, Tamaki N (2001) Intraarterial infusion of papaverine and change of cerebral hemodynamics in symptomatic cerebral vasospasm. Kobe J Med Sci 47:169–179
Turowski B, du Mesnil de Rochemont R, Beck J, et al (2005) Assessment of changes in cerebral circulation time due to vasospasm in a specific arterial territory: effect of angioplasty. Neuroradiology 47:134–143
Author information
Authors and Affiliations
Contributions
Study concepts/study design, MS, RvdB; data acquisition or data analysis/interpretation, all authors; manuscript drafting or manuscript revision for important intellectual content, all authors; approval of final version of submitted manuscript, all authors; agree to ensure any questions related to the work are appropriately resolved, all authors.
Corresponding author
Ethics declarations
Ethics approval
The Medical Research Involving Human Subjects Act does not apply to this study and therefore an approval of the Institutional Medical Ethics Review Committee was not necessary.
Consent to participate
For this type of study, formal consent is not required.
Consent for publication
No identifying data was included in the current study.
Competing interests
RvdB reports a consultancy agreement with Cerenovus neurovascular outside the submitted work (paid to institution). CBLMM reports grants from TWIN, during the conduct of the study, and grants from CVON/Dutch Heart Foundation, European Commission, Dutch Health Evaluation Program, and from Stryker outside the submitted work (paid to institution) and is a shareholder of Nico-lab. All other authors did not receive support from any organization for the submitted work, had no financial relationships with any organizations that might have an interest in the submitted work in the previous three years, and had no other relationships or activities that could appear to have influenced the submitted work.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Schembri, M., Verbaan, D., Emmer, B.J. et al. Cerebral circulation time on DSA during endovascular treatment in WFNS grade I aneurysmal SAH patients—a predictor of DCI?. Neuroradiology 63, 2131–2138 (2021). https://doi.org/10.1007/s00234-021-02749-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-021-02749-0