Abstract
Purpose
Cerebral hyperperfusion syndrome (CHPS) can result after anastomotic surgery as the reperfusion is established in chronically ischemic cerebral territories in patients of moyamoya disease (MMD). In this study, we have evaluated the feasibility of arterial spin labelling (ASL) perfusion MRI to predict cerebral hyperperfusion syndrome based on changes of cerebral blood flow (CBF) after revascularisation surgery in patients of MMD.
Methods
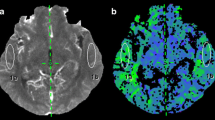
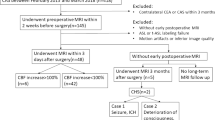
Our prospective study included 25 patients with MMD who underwent superficial temporal artery-middle cerebral artery (STA-MCA) bypass with or without dural/muscle synangiosis. ASL MRI was performed before and 1–7 days after surgery. On the side planned for operation, 5-mm ROI circle was drawn on the predetermined regions in frontal lobe, temporal lobe, parietal lobe and basal ganglia in proximal and distal territories of MCA to calculate ipsilateral CBF values (CBFi). An attempt was made to select the same location on contralateral side (non-operative) (CBFc) for each measurement for calculation of hemispheric normalised CBF (nCBFh) ratios. To adjust for inter individual variation among MR imagers and CBF, additional regions of interest were drawn within the cerebellum (CBFcbl) for cerebellar CBF normalised ratios (nCBFCbl).
Results
Of the 25 patients (26 operated hemispheres), 5 patients showed significant immediate postoperative symptoms suggestive of CHPS. Based on our findings, sensitivity and specificity of ASL perfusion to detect CHPS were evaluated. ASL was found to have 47–100% sensitivity and 45–88% specificity to detect CHPS. We have tried to calculate the prevalence of CHPS in postoperative patients of moyamoya disease, which in our study ranged from 6.83 to 40.70%.
Conclusion
Based on our results, we concluded that ASL perfusion is an appropriate alternative to standard nuclear medicine studies to monitor the changes in perfusion after STA-MCA bypass surgery in moyamoya patients. ASL MR perfusion can be used to identify changes in cerebral blood flow (CBF) for early detection of cerebral hyperperfusion syndrome in patients with otherwise normal conventional MRI sequences with very high sensitivity but moderate specificity.






Similar content being viewed by others
References
Janda PH, Bellew JG, Veerappan V (2009) Moyamoya disease: case report and literature review. J Am Osteopath Assoc 109(10):547–553
Kaku Y, Iihara K, Nakajima N (2012) Cerebral blood flow and metabolism of hyperperfusion after cerebral revascularization in patients with moyamoya disease. J Cereb Blood Flow Metab 32:2066–2075
Uchino H, Kuroda S, Hirata K (2012) Predictors and clinical features of postoperative hyperperfusion after surgical revascularization for moyamoya disease: a serial single photon emission CT/positron emission tomography study. Stroke 43:2610–2616
Zaharchuk G, Do HM, Marks MP (2011) Arterial spin-labeling MRI can identify the presence and intensity of collateral perfusion in patients with Moyamoya disease. Stroke 42:2485–2491
Hayashi K, Horie N, Suyama K, Nagata I (2012) Incidence and clinical features of symptomatic cerebral hyperperfusion syndrome after vascular reconstruction. World Neurosurg 78:447–454
Sundt TM Jr, Sharbrough FW, Piepgras DG, Kearns TP, Messick JM, O'Fallon WM (1981) Correlation of cerebral blood flow and electroencephalographic changes during carotid endarterectomy: with results of surgery and hemodynamics of cerebral ischemia. Mayo Clin Proc 56:533–543
Sugino T, Mikami T, Miyata K, Suzuki K, Houkin K, Mikuni N (2013) Arterial spin-labeling magnetic resonance imaging after revascularization of moyamoya disease. J Stroke Cerebrovasc Dis 22(6):811–816
Lee S, Yun TJ, Yoo RE (2018) Monitoring cerebral perfusion changes after revascularization in patients with moyamoya disease by using arterial spin-labeling MR imaging. Radiology 288(2):565–572
Goetti R, O’Gorman R, Khan N, Kellenberger CJ, Scheer I (2013) Arterial spin label- ling MRI for assessment of cerebral perfusion in children with moyamoya disease: comparison with dynamic susceptibility contrast MRI. Neuroradiology 55(5):639–647
Fan AP, Guo J, Khalighi MM, Gulaka PK, Shen B (2017) Long-delay arterial spin labeling provides more accurate cerebral blood flow measurements in moyamoya patients. Stroke 28(9):2441–2449
Wang R, Yu S, Alger JR (2014) Multi-delay arterial spin labeling perfusion MRI in moyamoya disease--comparison with CT perfusion imaging. Eur Radiol 24(5):1135–1144
Schmid S, Heijtel DF, Mutsaerts HJ (2015) Comparison of velocity- and acceleration-selective arterial spin labeling with [15O]H2O positron emission tomography. J Cereb Blood Flow Metab 35(8):1296–1303
Tortora D, Scavetta C, Rebella G (2020) Spatial coefficient of variation applied to arterial spin labeling MRI may contribute to predict surgical revascularization outcomes in pediatric moyamoya vasculopathy. Neuroradiology 62(8):1003–1015
Fahlström M, Lewén A, Enblad P, Larsson EM, Wikström J (2020) High intravascular signal arterial transit time artifacts have negligible effects on cerebral blood flow and cerebrovascular reserve capacity measurement using single post label delay arterial spin-labeling in patients with moyamoya disease. AJNR Am J Neuroradiol 41(3):430–436
Ukai R, Mikami T, Nagahama H, Wanibuchi M, Akiyama Y, Miyata K (2020) Arterial transit artifacts observed by arterial spin labeling in moyamoya disease. J Stroke Cerebrovasc Dis 29(9):105058
Author information
Authors and Affiliations
Contributions
Dr. Vivek Agarwal made a substantial contribution to the concept or design of the work, or acquisition, analysis or interpretation of data; drafted the article or revised it critically for important intellectual content; and approved the version to be published. Dr. Paramjeet Singh made a substantial contribution to the concept or design of the work, or acquisition, analysis or interpretation of data; drafted the article or revised it critically for important intellectual content; and approved the version to be published. Dr. Chirag K Ahuja made a substantial contribution to the concept or design of the work, or acquisition, analysis or interpretation of data, and drafted the article or revised it critically for important intellectual content. Dr. Sunil Kumar Gupta made a substantial contribution to the concept or design of the work, or acquisition, analysis or interpretation of data, and drafted the article or revised it critically for important intellectual content. Dr. Ashish Aggarwal made a substantial contribution to the concept or design of the work, or acquisition, analysis or interpretation of data; drafted the article or revised it critically for important intellectual content; and approved the version to be published. Dr. Rajashekhar Narayanan made a substantial contribution to the concept or design of the work, or acquisition, analysis or interpretation of data, and drafted the article or revised it critically for important intellectual content.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Agarwal, V., Singh, P., Ahuja, C.K. et al. Non-invasive assessment of cerebral microvascular changes for predicting postoperative cerebral hyperperfusion after surgical revascularisation for moyamoya disease: an arterial spin labelling MRI study. Neuroradiology 63, 563–572 (2021). https://doi.org/10.1007/s00234-020-02583-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02583-w