Abstract
Purpose
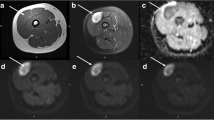
On T2-weighted images, most solid lesions exhibit nonspecific intermediate signal intensity, whereas most cystic lesions exhibit marked hyperintensity. In contrast, on T2-weighted images, a relatively small number of lesions exhibit hypointensity. This review aimed to differentiate, according to the histopathologic findings, head and neck lesions showing hypointensity on T2-weighted images.
Methods
In this review article, hypointense head and neck lesions on T2-weighted images are classified into the following nine categories: calcified or osseous lesions, granulomatous lesions, fibrous lesions, mucous- or proteincontaining lesions, hemosiderin-containing lesions, melanin-containing lesions, thyroglobulin-containing lesions, rapid blood flow, and air-filled spaces.
Conclusion
Knowledge regarding hypointense head and neck lesions on T2-weighted images allows radiologists to make accurate differential diagnoses.
Key points • Hypointense head and neck lesions on T2-weighted images include calcified or osseous lesions, granulomatous lesions, fibrous lesions, mucous- or protein-containing lesions, hemosiderin-containing lesions, melanin-containing lesions, thyroglobulin-containing lesions, rapid blood flow, and air-filled spaces. • Radiologists should recognize the hypointense head and neck lesions on T2-weighted images for the final correct diagnosis, resulting in appropriate patient management. |














Similar content being viewed by others
References
Hoch M, Win W, Hagiwara M, Fatterpekar G, Patel S (2016) Orbital lesions with low signal intensity on T2-weighted imaging. Clin Radiol 71(1):e88–e95. https://doi.org/10.1016/j.crad.2015.10.011
Aribandi M, McCoy VA, Bazan C 3rd (2007) Imaging features of invasive and noninvasive fungal sinusitis: a review. Radiographics 27(5):1283–1296. https://doi.org/10.1148/rg.275065189
Kim SC, Ryoo I, Shin JM, Suh S, Jung HN, Shin SU (2020) MR findings of fungus ball: significance of high signal intensity on T1-weighted images. J Korean Med Sci 35(3):e22. https://doi.org/10.3346/jkms.2020.35.e22
de Graaf P, Goricke S, Rodjan F, Galluzzi P, Maeder P, Castelijns JA, Brisse HJ, European Retinoblastoma Imaging Collaboration (2012) Guidelines for imaging retinoblastoma: imaging principles and MRI standardization. Pediatr Radiol 42(1):2–14. https://doi.org/10.1007/s00247-011-2201-5
Rodjan F, de Graaf P, van der Valk P, Hadjistilianou T, Cerase A, Toti P, de Jong MC, Moll AC, Castelijns JA, Galluzzi P, European Retinoblastoma Imaging Collaboration (2015) Detection of calcifications in retinoblastoma using gradient-echo MR imaging sequences: comparative study between in vivo MR imaging and ex vivo high-resolution CT. AJNR Am J Neuroradiol 36(2):355–360. https://doi.org/10.3174/ajnr.A4163
Kato H, Kanematsu M, Watanabe H, Nagano A, Shu E, Seishima M, Miyazaki T (2016) MR imaging findings of pilomatricomas: a radiological-pathological correlation. Acta Radiol 57(6):726–732. https://doi.org/10.1177/0284185115597717
Pakalniskis MG, Berg AD, Policeni BA, Gentry LR, Sato Y, Moritani T, Smoker WR (2015) The many faces of granulomatosis with polyangiitis: a review of the head and neck Imaging manifestations. AJR Am J Roentgenol 205(6):W619–W629. https://doi.org/10.2214/AJR.14.13864
Allen SD, Harvey CJ (2007) Imaging of Wegener’s granulomatosis. Br J Radiol 80(957):757–765. https://doi.org/10.1259/bjr/34705892
Chapman MN, Fujita A, Sung EK, Siegel C, Nadgir RN, Saito N, Sakai O (2017) Sarcoidosis in the head and neck: an illustrative review of clinical presentations and imaging findings. AJR Am J Roentgenol 208(1):66–75. https://doi.org/10.2214/AJR.16.16058
Fujita A, Sakai O, Chapman MN, Sugimoto H (2012) IgG4-related disease of the head and neck: CT and MR imaging manifestations. Radiographics 32(7):1945–1958. https://doi.org/10.1148/rg.327125032
Thompson A, Whyte A (2018) Imaging of IgG4-related disease of the head and neck. Clin Radiol 73(1):106–120. https://doi.org/10.1016/j.crad.2017.04.004
Murphey MD, Ruble CM, Tyszko SM, Zbojniewicz AM, Potter BK, Miettinen M (2009) From the archives of the AFIP: musculoskeletal fibromatoses: radiologic-pathologic correlation. Radiographics 29(7):2143–2173. https://doi.org/10.1148/rg.297095138
Vandevenne JE, De Schepper AM, De Beuckeleer L, Van Marck E, Aparisi F, Bloem JL, Erkorkmaz Z, Brijs S (1997) New concepts in understanding evolution of desmoid tumors: MR imaging of 30 lesions. Eur Radiol 7(7):1013–1019. https://doi.org/10.1007/s003300050243
Braschi-Amirfarzan M, Keraliya AR, Krajewski KM, Tirumani SH, Shinagare AB, Hornick JL, Baldini EH, George S, Ramaiya NH, Jagannathan JP (2016) Role of imaging in management of desmoid-type fibromatosis: a primer for radiologists. Radiographics 36(3):767–782. https://doi.org/10.1148/rg.2016150153
Liu Y, Li K, Shi H, Tao X (2014) Solitary fibrous tumours in the extracranial head and neck region: correlation of CT and MR features with pathologic findings. Radiol Med 119(12):910–919. https://doi.org/10.1007/s11547-014-0409-9
Blacksin MF, White LM, Hameed M, Kandel R, Patterson FR, Benevenia J (2005) Granular cell tumor of the extremity: magnetic resonance imaging characteristics with pathologic correlation. Skelet Radiol 34(10):625–631. https://doi.org/10.1007/s00256-005-0925-8
Shizukuishi T, Abe O, Haradome H, Fukushima T, Katayama Y, Sugitani M (2014) Granular cell tumor of the neurohypophysis with optic tract edema. Jpn J Radiol 32(3):179–182. https://doi.org/10.1007/s11604-013-0279-4
Prause CA, Zhai Q, Weindling SM (2017) Pharyngeal amyloidomas: variable appearance on imaging. Neuroradiol J 30(3):235–239. https://doi.org/10.1177/1971400917695318
Kawashima A, Alleman WG, Takahashi N, Kim B, King BF Jr, LeRoy AJ (2011) Imaging evaluation of amyloidosis of the urinary tract and retroperitoneum. Radiographics 31(6):1569–1582. https://doi.org/10.1148/rg.316115519
Sekiya K, Watanabe M, Nadgir RN, Buch K, Flower EN, Kaneda T, Sakai O (2014) Nasopharyngeal cystic lesions: Tornwaldt and mucous retention cysts of the nasopharynx: findings on MR imaging. J Comput Assist Tomogr 38(1):9–13. https://doi.org/10.1097/RCT.0b013e3182a77699
Van Tassel P, Lee YY, Jing BS, De Pena CA (1989) Mucoceles of the paranasal sinuses: MR imaging with CT correlation. AJR Am J Roentgenol 153(2):407–412. https://doi.org/10.2214/ajr.153.2.407
Kim EY, Kim HJ, Chung SK, Dhong HJ, Kim HY, Yim YJ, Kim ST, Jeon P, Ko YH (2008) Sinonasal organized hematoma: CT and MR imaging findings. AJNR Am J Neuroradiol 29(6):1204–1208. https://doi.org/10.3174/ajnr.A1042
Tatekawa H, Shimono T, Ohsawa M, Doishita S, Sakamoto S, Miki Y (2018) Imaging features of benign mass lesions in the nasal cavity and paranasal sinuses according to the 2017 WHO classification. Jpn J Radiol 36(6):361–381. https://doi.org/10.1007/s11604-018-0739-y
Hur J, Kim JK, Byun JS, Lee WJ (2015) Imaging characteristics of sinonasal organized hematoma. Acta Radiol 56(8):955–959. https://doi.org/10.1177/0284185114542364
Kawaguchi M, Kato H, Tomita H, Mizuta K, Aoki M, Hara A, Matsuo M (2017) Imaging characteristics of malignant sinonasal tumors. J Clin Med 6(12). https://doi.org/10.3390/jcm6120116
Chapman MC, Soares BP, Li Y, Shum DJ, Glenn OA, Glastonbury CM, Courtier JL (2019) Congenital oral masses: an anatomic approach to diagnosis. Radiographics 39(4):1143–1160. https://doi.org/10.1148/rg.2019180128
Takashima S, Ueda M, Shibata A, Takayama F, Momose M, Yamashita K (2001) MR imaging of the lingual thyroid. Comparison to other submucosal lesions. Acta Radiol 42(4):376–382
Zander DA, Smoker WR (2014) Imaging of ectopic thyroid tissue and thyroglossal duct cysts. Radiographics 34(1):37–50. https://doi.org/10.1148/rg.341135055
Funding
This study was not funded.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kato, H., Kawaguchi, M., Ando, T. et al. Hypointense head and neck lesions on T2-weighted images: correlation with histopathologic findings. Neuroradiology 62, 1207–1217 (2020). https://doi.org/10.1007/s00234-020-02483-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-020-02483-z