Abstract
Purpose
Diffusion tensor imaging (DTI) in flexion (F) and extension (E) may serve as a sensitive diagnostic tool in early symptoms of myelopathy. The aim of this study was to compare values of water diffusion parameters on dynamic cervical DTI in early stage of myelopathy.
Methods
Study enrolled 10 patients with an early stage of cervical myelopathy, in grade I/II of Nurick classification. All subjects were scanned with flexion-extension 3T MRI. Fractional anisotropy (FA), apparent diffusion coefficient (ADC), RD (radial diffusivity), AD (axial diffusivity) and TRACEW (trace diffusion) were measured at C2, compression level (CL) and C7. Parameters were compared between 3 levels and F and E positions.
Results
Flexion DTI revealed significant difference only for TRACEW between C2 and C7 (105.8 ± 18.9 vs. 83.7 ± 14, respectively; p = 0.0029). Extension DTI showed differences for ADC between CL and C7 (1378.9 ± 381.8 vs. 1227.2 ± 269.2; p = 0.001), reduced FA from 664.6 ± 56.3 at C2 down to 553.1 ± 75.5 (p = 0.001) at CL and 584.7 ± 40.7 at C7 (p = 0.002). Differences of RD in E were significant through all levels and reached 612.9 ± 105.1, 955.3 ± 319.4 and 802.1 ± 194.1 at C2, CL and C7, respectively. TRACEW lowered from 92.3 ± 14.4 at C2 to 66.9 ± 21.1 at CL (p = 0.0001) and 64.4 ± 15.5 at C7 (p = 0.0002). Comparison of DTI between F and E showed differences for all parameters except AD. RD was significantly higher in E at CL (p = 0.003) and C7 (0.013), but TRACEW increased in F at CL by 27.4% (p = 0.001) and at C7 by 23.1% (p = 0.013). FA was reduced at CL in E (p = 0.027) and similarly ADC in F (p = 0.048).
Conclusion
Dynamic DTI of the cervical spine is feasible and can detect subtle spinal cord damage of functional relevance in cervical myelopathy. A marked increase of RD and decrease of FA and TRACEW values in extension were found to be indicative for an early structural cord injury in myelopathy.





Similar content being viewed by others
References
Le Bihan D, Mangin JF, Poupon C et al (2001) Diffusion tensor imaging: concepts and applications. J Magn Reson Imaging 13:534–546
Vedantam A, Jirjis MB, Schmit BD, Wang MC, Ulmer JL, Kurpad SN (2014) Diffusion tensor imaging of the spinal cord: insights from animal and human studies. Neurosurgery 74:1–8; discussion 8; quiz 8. https://doi.org/10.1227/NEU.0000000000000171
Demir A, Ries M, Moonen CTW, Vital JM, Dehais J, Arne P, Caillé JM, Dousset V (2003) Diffusion-weighted MR imaging with apparent diffusion coefficient and apparent diffusion tensor maps in cervical spondylotic myelopathy. Radiology 229:37–43. https://doi.org/10.1148/radiol.2291020658
Ellingson BM, Kurpad SN, Schmit BD (2008) Functional correlates of diffusion tensor imaging in spinal cord injury. Biomed Sci Instrum 44:28–33
Czyz M, Tykocki T, Szewczyk P, Jarmundowicz W (2017) Application of diffusion tensor imaging in the prognosis of outcome after traumatic cervical spinal cord injury. J Spinal Stud Surg 1:25–28
Endo T, Suzuki S, Utsunomiya A, Uenohara H, Tominaga T (2011) Prediction of neurological recovery using apparent diffusion coefficient in cases of incomplete spinal cord injury. Neurosurgery 68:329–336. https://doi.org/10.1227/NEU.0b013e3182031ce7
Guan X, Fan G, Wu X, Gu G, Gu X, Zhang H, He S (2015) Diffusion tensor imaging studies of cervical spondylotic myelopathy: a systemic review and meta-analysis. PLoS One 10:e0117707. https://doi.org/10.1371/journal.pone.0117707
Hori M, Okubo T, Aoki S, Kumagai H, Araki T (2006) Line scan diffusion tensor MRI at low magnetic field strength: feasibility study of cervical spondylotic myelopathy in an early clinical stage. J Magn Reson Imaging 23:183–188. https://doi.org/10.1002/jmri.20488
Kara B, Celik A, Karadereler S, Ulusoy L, Ganiyusufoglu K, Onat L, Mutlu A, Ornek I, Sirvanci M, Hamzaoglu A (2011) The role of DTI in early detection of cervical spondylotic myelopathy: a preliminary study with 3-T MRI. Neuroradiology 53:609–616. https://doi.org/10.1007/s00234-011-0844-4
Jones J, Lerner A, Kim PE, Law M, Hsieh PC (2011) Diffusion tensor imaging in the assessment of ossification of the posterior longitudinal ligament: a report on preliminary results in 3 cases and review of the literature. Neurosurg Focus 30:E14. https://doi.org/10.3171/2011.1.FOCUS10262
Maki S, Koda M, Kitamura M, Inada T, Kamiya K, Ota M, Iijima Y, Saito J, Masuda Y, Matsumoto K, Kojima M, Obata T, Takahashi K, Yamazaki M, Furuya T (2017) Diffusion tensor imaging can predict surgical outcomes of patients with cervical compression myelopathy. Eur Spine J 26:2459–2466. https://doi.org/10.1007/s00586-017-5191-7
Wen CY, Cui JL, Liu HS, Mak KC, Cheung WY, Luk KDK, Hu Y (2014) Is diffusion anisotropy a biomarker for disease severity and surgical prognosis of cervical spondylotic myelopathy? Radiology 270:197–204. https://doi.org/10.1148/radiol.13121885
Henderson FC, Geddes JF, Vaccaro AR et al (2005) Stretch-associated injury in cervical spondylotic myelopathy: new concept and review. Neurosurgery 56:1101–1113
Harada T, Tsuji Y, Mikami Y, Hatta Y, Sakamoto A, Ikeda T, Tamai K, Hase H, Kubo T (2010) The clinical usefulness of preoperative dynamic MRI to select decompression levels for cervical spondylotic myelopathy. Magn Reson Imaging 28:820–825. https://doi.org/10.1016/j.mri.2010.03.038
Xu N, Wang S, Yuan H, Liu X, Liu Z (2017) Does dynamic supine magnetic resonance imaging improve the diagnostic accuracy of cervical spondylotic myelopathy? A review of the current evidence. World Neurosurg 100:474–479. https://doi.org/10.1016/j.wneu.2017.01.047
Zeitoun D, El Hajj F, Sariali E et al (2015) Evaluation of spinal cord compression and hyperintense intramedullary lesions on T2-weighted sequences in patients with cervical spondylotic myelopathy using flexion-extension MRI protocol. Spine J 15:668–674. https://doi.org/10.1016/j.spinee.2014.12.001
Zhang L, Zeitoun D, Rangel A, Lazennec JY, Catonné Y, Pascal-Moussellard H (2011) Preoperative evaluation of the cervical spondylotic myelopathy with flexion-extension magnetic resonance imaging: about a prospective study of fifty patients. Spine 36:E1134–E1139. https://doi.org/10.1097/BRS.0b013e3181f822c7
Morishita Y, Maeda T, Naito M, Ueta T, Shiba K (2013) The pincers effect on cervical spinal cord in the development of traumatic cervical spinal cord injury without major fracture or dislocation. Spinal Cord 51:331–333. https://doi.org/10.1038/sc.2012.157
Fehlings MG, Tetreault LA, Riew KD, Middleton JW, Aarabi B, Arnold PM, Brodke DS, Burns AS, Carette S, Chen R, Chiba K, Dettori JR, Furlan JC, Harrop JS, Holly LT, Kalsi-Ryan S, Kotter M, Kwon BK, Martin AR, Milligan J, Nakashima H, Nagoshi N, Rhee J, Singh A, Skelly AC, Sodhi S, Wilson JR, Yee A, Wang JC (2017) A clinical practice guideline for the management of patients with degenerative cervical myelopathy: recommendations for patients with mild, moderate, and severe disease and nonmyelopathic patients with evidence of cord compression. Glob Spine J 7:70S–83S. https://doi.org/10.1177/2192568217701914
Tykocki T, du Plessis J, Wynne-Jones G (2018) Correlation between the severity of myelopathy and cervical morphometric parameters on dynamic magnetic resonance imaging. Acta Neurochir 160:1251–1258. https://doi.org/10.1007/s00701-018-3540-x
Tykocki T, du Plessis J, Wynne-Jones G (2018) Cervical spine and cord angle mismatch in the pathogenesis of myelopathy. World Neurosurg 115:e272–e278. https://doi.org/10.1016/j.wneu.2018.04.033
Tykocki T, du Plessis J, Wynne-Jones G (2018) Analysis of morphometric parameters in cervical canal stenosis on neutral and dynamic magnetic resonance imaging. World Neurosurg 114:e317–e322. https://doi.org/10.1016/j.wneu.2018.02.179
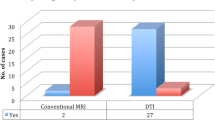
Lee S, Lee YH, Chung T-S, Jeong EK, Kim S, Yoo YH, Kim IS, Yoon CS, Suh JS, Park JH (2015) Accuracy of diffusion tensor imaging for diagnosing cervical spondylotic myelopathy in patients showing spinal cord compression. Korean J Radiol 16:1303–1312. https://doi.org/10.3348/kjr.2015.16.6.1303
Schatlo B, Remonda L, Gruber P, Fandino J, Rohde V, Fathi AR, Berberat J (2018) Cervical spine prospective feasibility study : dynamic flexion-extension diffusion-tensor weighted magnetic resonance imaging. Clin Neuroradiol. https://doi.org/10.1007/s00062-018-0686-0
Jones JGA, Cen SY, Lebel RM, Hsieh PC, Law M (2013) Diffusion tensor imaging correlates with the clinical assessment of disease severity in cervical spondylotic myelopathy and predicts outcome following surgery. AJNR Am J Neuroradiol 34:471–478. https://doi.org/10.3174/ajnr.A3199
Mamata H, Jolesz FA, Maier SE (2005) Apparent diffusion coefficient and fractional anisotropy in spinal cord: age and cervical spondylosis-related changes. J Magn Reson Imaging 22:38–43. https://doi.org/10.1002/jmri.20357
Saksena S, Middleton DM, Krisa L, Shah P, Faro SH, Sinko R, Gaughan J, Finsterbusch J, Mulcahey MJ, Mohamed FB (2016) Diffusion tensor imaging of the normal cervical and thoracic pediatric spinal cord. AJNR Am J Neuroradiol 37:2150–2157. https://doi.org/10.3174/ajnr.A4883
Klawiter EC, Schmidt RE, Trinkaus K, Liang HF, Budde MD, Naismith RT, Song SK, Cross AH, Benzinger TL (2011) Radial diffusivity predicts demyelination in ex vivo multiple sclerosis spinal cords. NeuroImage 55:1454–1460. https://doi.org/10.1016/j.neuroimage.2011.01.007
Cui J-L, Li X, Chan T-Y, Mak KC, Luk KDK, Hu Y (2015) Quantitative assessment of column-specific degeneration in cervical spondylotic myelopathy based on diffusion tensor tractography. Eur Spine J 24:41–47. https://doi.org/10.1007/s00586-014-3522-5
DeBoy CA, Zhang J, Dike S et al (2007) High resolution diffusion tensor imaging of axonal damage in focal inflammatory and demyelinating lesions in rat spinal cord. Brain J Neurol 130:2199–2210. https://doi.org/10.1093/brain/awm122
Kuhn FP, Feydy A, Launay N, Lefevre-Colau MM, Poiraudeau S, Laporte S, Maier MA, Lindberg P (2016) Kinetic DTI of the cervical spine: diffusivity changes in healthy subjects. Neuroradiology 58:929–935. https://doi.org/10.1007/s00234-016-1709-7
Lindberg PG, Sanchez K, Ozcan F, Rannou F, Poiraudeau S, Feydy A, Maier MA (2016) Correlation of force control with regional spinal DTI in patients with cervical spondylosis without signs of spinal cord injury on conventional MRI. Eur Radiol 26:733–742. https://doi.org/10.1007/s00330-015-3876-z
Song S-K, Sun S-W, Ramsbottom MJ, Chang C, Russell J, Cross AH (2002) Dysmyelination revealed through MRI as increased radial (but unchanged axial) diffusion of water. NeuroImage 17:1429–1436
Pierpaoli C, Basser PJ (1996) Toward a quantitative assessment of diffusion anisotropy. Magn Reson Med 36:893–906
O’Donnell LJ, Westin C-F (2011) An introduction to diffusion tensor image analysis. Neurosurg Clin N Am 22:185–viii. https://doi.org/10.1016/j.nec.2010.12.004
Tang L, Wen Y, Zhou Z, von Deneen KM, Huang D, Ma L (2013) Reduced field-of-view DTI segmentation of cervical spine tissue. Magn Reson Imaging 31:1507–1514. https://doi.org/10.1016/j.mri.2013.07.003
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this study.
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tykocki, T., English, P., Minks, D. et al. Predictive value of flexion and extension diffusion tensor imaging in the early stage of cervical myelopathy. Neuroradiology 60, 1181–1191 (2018). https://doi.org/10.1007/s00234-018-2097-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-018-2097-y