Abstract
Purpose
This study sought to analyze the medication knowledge and awareness of medication adjustment options during intercurrent illness (sick day rules) of patients ≥ 70 years treated at a hospital for geriatric medicine in northern Germany.
Methods
The study was designed as a cross-sectional, interview-based pilot study, was approved by the Ethics Committee of Hannover Medical School (No. 10274_BO_K_2022; date of approval: 11 March 2022), and enrolled a convenience sample of 100 patients between May and December 2022.
Results
The median of the average medication knowledge score in the study population (median age 82 years (IQR 75–87); 71% female) was 5 on a scale from 0 to 6 (IQR 3.8–5.6). Women achieved higher average medication knowledge scores than men (median 5.1 (IQR 4–5.6) vs. median 4.3 (IQR 3.6–5.1); p = 0.012), and patients < 80 years achieved higher average medication knowledge scores than patients ≥ 80 years (median 5.4 (IQR 4.9–5.7) vs. median 4.3 (IQR 3.2–5.3); p < 0.001). Sick day rules were known for only 1.1% of drugs for which sick day rules were applicable. Fifty-two percent of the patients reported that their general practitioner contributed most to their medication knowledge, and 66% considered their daily number of drugs to take adequate.
Conclusion
Our study showed that medication knowledge of older patients was overall satisfying. Awareness of sick day rules, however, was poor. Future studies should evaluate the clinical benefits of sick day rules and ways of better communicating sick day rules to patients. In this regard, general practitioners may play a decisive role.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The demographic change in industrialized nations is leading to aging societies and increasing proportions of multimorbid patients who are exposed to polypharmacy, which is commonly defined as the intake of five or more drugs as long-term medication [1]. In Germany, approximately 40% of patients over the age of 65 are exposed to polypharmacy [2].
The ability of patients to understand medication charts and safely and correctly use both prescription medicines and over-the-counter drugs is significantly influenced by their level of health literacy [3]. Advanced age and polypharmacy can lead to deficits in medication knowledge, which may negatively impact on therapy adherence [4] and compromise treatment success [5]. A bicentric study by Freyer and colleagues revealed substantial deficits in medication knowledge among patients of an acute-care hospital and a geriatric rehabilitation clinic [6]. Patients were only able to name approximately half of their discharge medications correctly. Factors influencing knowledge deficits were lack of a medication chart and older age, among others [6]. A study by Krause et al. found that general practitioners (GPs) extensively changed medication regimens of patients discharged from an acute-care geriatric hospital, which may further contribute to deficits in patients’ medication knowledge [7].
Patients who are not familiar with the drugs they are taking, the indications, or options of adjustment during phases of acute illness may not only experience treatment failure—even more serious complications such as adrenal crisis can occur [8]. Insufficient medication knowledge may thus entail an increased use of medical resources [5].
One strategy of dealing with this challenge is communication of so-called sick day rules to patients by healthcare professionals. Sick day rules are instructions to pause or adjust the dosages of certain medications during episodes of acute illness [9,10,11]. For example, patients with adrenal insufficiency should be instructed to double or triple their daily oral dose of hydrocortisone even during minor illness [12]. Patients taking diuretics may be advised to temporarily discontinue those during phases of diarrhea or vomiting to mitigate the risk of dehydration. For similar reasons, it can be advisable to pause antihypertensive agents such as angiotensin-converting enzyme inhibitors during disease states associated with increased loss of fluid (e.g., febrile infections). If antihypertensive agents were continued without cessation during phases of acute illness, serious complications such as hypotension, dizziness, and falls might result. After a patient’s recovery, these medications can be re-initiated [9].
To date, no generally applicable procedure to inform patients about sick day rules has been established. In Scotland, Medicine Sick Day Rules cards containing information about medication adjustments during episodes of acute illness were introduced by the National Health Service (NHS) Highland in 2013 [13]. According to NHS Highland, medicines that should be paused during phases of intercurrent illness are angiotensin-converting enzyme inhibitors, angiotensin-receptor blockers, non-steroidal anti-inflammatory drugs, diuretics, and metformin [13]. Although this initiative by NHS Highland temporally correlated with a decrease in hospital admissions [14, 15], suggesting potential therapeutic benefits, sick day rules cards have neither been standardized in the United Kingdom nor internationally. Besides the medications proposed by NHS Highland, Diabetes Canada added direct renin inhibitors (e.g., aliskiren), sulfonylureas (e.g., gliclazide, glimepiride, glyburide), and sodium–glucose cotransporter 2 inhibitors to their Sick-Day Medication List of drugs to withhold during acute illness and/or states of dehydration [16]. Sodium–glucose cotransporter 2 inhibitors should be paused during intercurrent illness to reduce the risk of potentially life-threatening diabetic ketoacidosis [17]. A review article by Keller also mentioned insulins (e.g., insulin aspart, insulin lispro, insulin degludec, and insulin glargine) as examples of drugs for which sick day rules may be communicated to patients [9].
Morris and colleagues reported that GPs and pharmacists considered sick day rules useful; however, GPs and pharmacists disagreed about who should ultimately be responsible to inform patients about sick day rules [10].
In the present study, we analyzed the medication knowledge and awareness of adjustment options (i.e., sick day rules) of patients aged ≥ 70 years who were treated at a hospital for geriatric medicine in northern Germany. We investigated potential influences of age or sex on medication knowledge and whether patients’ medication knowledge differed between drug groups.
Methods
Study design
The study was designed as a cross-sectional, interview-based pilot study. It was planned to enroll a convenience sample of 100 patients. To this end, patients treated at the Center for Geriatric Medicine (Zentrum für Medizin im Alter), DIAKOVERE Henriettenstift, Hannover, Germany between May and December 2022 were screened for eligibility (see section “Eligibility criteria”) and asked by one of the joint first authors (OK or CTZ) to participate in the study. Patients willing to participate in the study were informed about the aims of the study, and written informed consent was obtained. Patients who met all eligibility criteria and who had provided written informed consent were interviewed by CTZ using a questionnaire specifically designed for this study (see section “Study questionnaire”). Patients were allowed to use their medication chart during the interview. Patients’ relatives—if present at the time of the interview—were allowed to stay and support the study participants during the interview, as this situation better reflected real-world conditions.
Study questionnaire
To address the research questions of this study, a questionnaire was devised by the study authors (Supplementary Material 1 (English version) and Supplementary Material 2 (German version)). The questionnaire was used by CTZ during the interviews and addressed the following medication-related topics: drug name; indication; dosage; and frequency of application.
These medication-related topics were investigated for each drug in the medication charts of the study participants. One point was achievable for the categories drug name and frequency of application, while up to two points were achievable for the categories indication and dosage. The reason for the different maximum scores in the categories drug name and frequency of application (one point) as opposed to the categories indication and dosage (two points) was that more nuanced answers were expected for the latter two categories, requiring a more differentiated scoring system. For each drug, the achieved points were summed up to yield the medication knowledge score (range 0–6, with higher scores indicating better medication knowledge). To allow for meaningful comparisons between patients taking different numbers of drugs, the medication knowledge scores of all drugs of a patient were summed up and subsequently divided by the number of drugs the patient was taking, yielding the average medication knowledge score (range 0–6, with higher scores indicating better medication knowledge). Examples of patient answers and corresponding ratings are provided in Table 1. For instance, a patient who answered that she took “Xarelto, for blood thinning, one tablet in the morning” would achieve 4 out of 6 points for this drug (a perfect, 6-point answer in this example would have been: “Xarelto, for blood thinning to prevent a stroke, one 20-mg tablet in the morning”). Correctness of answers was evaluated based on the medication chart provided to patients by their GP. If patients did not have a GP, the medication chart from the Center for Geriatric Medicine was used to assess answer correctness.
Knowledge of sick day rules was investigated separately by asking patients for each drug of their medication chart to which a sick day rule was applicable (e.g., ACE inhibitors, NSAIDs, diuretics, etc.): “Is there anything to observe for this drug in case of acute illness?”. Examples of patient answers on sick day rules and corresponding ratings are also showcased in Table 1. Of note, over-the-counter (OTC) preparations were excluded from analysis due to the absence of a prescribing physician who could have possibly communicated sick day rules to the patient.
In addition, patients’ opinion about their daily number of drugs was evaluated on a 5-point Likert scale: 1 = “too few”; 2 = “rather too few”; 3 = “adequate number”; 4 = “rather too many”; 5 = “too many”.
Finally, patients were asked who or what contributed most to their medication knowledge, using a predefined 8-item list of answer options (single choice): pharmacy; general practitioner; medical specialist; partner/spouse, relatives, friends; television; the press, magazines; the Internet; or other.
Drugs and drug classes for which sick days rules were considered applicable
Based on our review of the literature [9, 12, 13, 16, 17] and pathophysiological considerations, we decided that, for the purpose of this study, sick day rules were applicable to antihypertensive agents (e.g., angiotensin-converting enzyme inhibitors, dihydropyridine calcium channel blockers, diuretics, etc.), laxatives, insulins, oral antidiabetic agents (e.g., metformin, sulfonylureas, sodium–glucose cotransporter 2 inhibitors, etc.), methotrexate, glucocorticosteroids, and non-steroidal anti-inflammatory drugs.
Pretest
Prior to the start of the study, a pretest with three randomly selected patients was conducted, which confirmed the applicability of the study questionnaire under real-world conditions and the feasibility of the study as a whole. No modifications of the questionnaire were necessary after the pretest.
Eligibility criteria
Patients were eligible for enrollment in the study (i) if they were treated at the Center for Geriatric Medicine, DIAKOVERE Henriettenstift, Hannover, Germany, between May and December 2022 as inpatients or outpatients (in the hospital’s day clinic); (ii) if they were aged ≥ 70 years; (iii) if they had been regularly taking at least five different drugs for at least the past three months; and (iv) if they were able to provide written informed consent.
Drug classification
Drugs were classified according to the Anatomical Therapeutic Chemical (ATC) Classification for Germany, version 2022 [18]. For statistical analyses, first-level ATC codes were used.
Statistical analyses
All statistical analyses were performed with IBM SPSS Statistics for Windows, version 28 (Armonk, New York, USA). Quantitative variables were tested for normal distribution with the Shapiro–Wilk test. Due to skewed distribution, quantitative variables are depicted as medians with interquartile ranges (IQRs). For quantitative variables, the Mann–Whitney U test or Kruskal–Wallis test was used to investigate potential differences between two groups or ≥ three groups, respectively. Categorical variables are reported as absolute and relative frequencies. P values (two-sided) < 0.05 were considered statistically significant. Due to the exploratory character of our study, no adjustments for multiple testing were conducted.
Results
Study population and interview characteristics
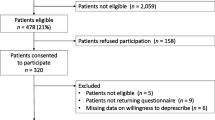
250 patients were screened between May and December 2022 to enroll the pre-planned convenience sample of 100 participants (Fig. 1). The most frequent reason for exclusion was use of less than five drugs per day. The median age in the study cohort (n = 100) was 82 years (IQR 75–87 years; range 70–96 years) and 71% of the patients were female. Forty-one percent of the patients were < 80 years, while 59% were ≥ 80 years.
Patients took a median of 8 drugs per day (IQR 6–10 drugs; range 5–17 drugs). The number of drugs per day did not differ statistically significantly between men and women (median 8 drugs (IQR 7–9.5 drugs) vs. median 8 drugs (IQR 6–10 drugs); p = 0.863), nor between younger (i.e., < 80 years) and older (i.e., ≥ 80 years) patients (median 7 drugs (IQR 6–10 drugs) vs. median 8 drugs (IQR 7–10 drugs); p = 0.131).
The median duration of the interviews was 24.5 min (IQR 20–30 min; range 15–60 min), and 95% of the patients used their medication chart as support. Patients’ relatives were present in 8% of the interviews.
Average medication knowledge score
The median of the average medication knowledge score in the total study population was 5 (IQR 3.8–5.6; range 0.9–6). Women achieved higher average medication knowledge scores than men (median 5.1 (IQR 4–5.6) vs. median 4.3 (IQR 3.6–5.1); p = 0.012), and patients < 80 years achieved higher average medication knowledge scores than patients ≥ 80 years (median 5.4 (IQR 4.9–5.7) vs. median 4.3 (IQR 3.2–5.3); p < 0.001).
Comparison of drug groups
To investigate potential differences in patients’ medication knowledge about different drug groups, the four most frequently used drug groups in the study population (i.e., ATC groups A (alimentary tract and metabolism), B (blood and blood forming organs), C (cardiovascular system), and N (nervous system); Table 2) and the remaining drugs (summarized as “other”) were compared. The latter group comprised ATC groups D (dermatologicals), G (genitourinary system and sex hormones), H (systemic hormonal preparations, excluding sex hormones and insulins), J (antiinfectives for systemic use), L (antineoplastic and immunomodulating agents), M (musculoskeletal system), P (antiparasitic products, insecticides, and repellents), R (respiratory system), S (sensory organs), and V (various). Patients’ medication knowledge scores did not differ between ATC groups A (median 5 (IQR 4–6)), B (median 5 (IQR 4–6)), C (median 5 (IQR 4–6)), N (median 6 (IQR 4–6)), and the group of “other” drugs (median 5 (IQR 4–6)) (p = 0.688).
Knowledge of sick day rules
Sick day rules were applicable to approximately one-third of drugs used by the study population (33.1%; 271/819). Of note, sick day rules were known for only 3 of these 271 drugs (1.1%). The 3 drugs for which sick day rules were known (candesartan, furosemide, methotrexate) were taken by 3 different patients. For the remaining 268 drugs (98.9%), patients were not aware that sick day rules existed.
Patients’ opinion about their daily number of drugs to take
Two-thirds (66%) of the patients considered their daily number of drugs to take “adequate” (Fig. 2). Every fifth patient (20%) and 13% of the patients found that they had to take “rather too many” or “too many” drugs per day, respectively.
Contribution to medication knowledge
More than half of the patients (52%) reported that their general practitioner contributed most to their medication knowledge, with medical specialists (e.g., cardiologists, neurologists, etc.) occupying the second rank (17%) (Fig. 3). Astonishingly, the media only played a minor role in contributing to patients’ medication knowledge (television: 0%; the press, magazines: 1%; the Internet: 3%). Twelve percent of the patients used “other” information sources. When specifically asked about those “other” information sources, all twelve patients named the package insert.
Discussion
Our study provided three main results. First, female sex and younger age (< 80 years) were associated with higher medication knowledge. Second, two-thirds of the patients considered their number of drugs to take per day appropriate, suggesting a high level of trust in prescribers, especially general practitioners (GPs), who also contributed most to patients’ medication knowledge in our study. Third, sick day rules were only known for a minority (1.1%) of drugs for which sick day rules were applicable, whereas for the remaining 98.9% of drugs, patients were unaware that medication adjustment options existed in the event of acute illness.
Comparable to our study, Okuyan and colleagues detected an association between higher age and lower medication knowledge [19]. It might be speculated that patients aged ≥ 80 years in our study generally displayed reduced cognitive functions compared to their younger counterparts, and that this might have been the underlying reason for lower medication knowledge scores. However, even though we did not perform comprehensive neuropsychological testings, cognitive impairment was excluded as part of the clinical evaluation of eligibility. A possible explanation for the lower medication knowledge of patients ≥ 80 years might be delegation of the responsibility for medication preparation and administration to relatives or a nursing service, although this was not investigated in our study. Another explanation might be engagement of patients ≥ 80 years with a healthcare system that has largely been paternalistic and fostered a “doctor knows best” attitude, with fewer opportunities to ask questions and be involved in shared decision making. In contrast to the Okuyan et al. study [19, 20], in which male patients achieved higher medication knowledge scores than female patients, male sex was associated with lower medication knowledge in our investigation.
Although other studies used different methodologies to assess medication knowledge, which substantially limits comparability with our results, it may be assumed that the average medication knowledge in our study was relatively high compared to other investigations (median of 5 for the average medication knowledge score on a scale from 0 to 6). By contrast, in a study by Timmerman et al., which focused on prescriptions of analgesics, around 50% of the study population had no knowledge of at least one aspect (i.e., medication name, dosage, or frequency of application) of their prescription [4]. Similarly, 54.8% of the patients interviewed by Sancar et al. did not know the reason they were taking drugs, and 60.3% did not know when or how to take their medication [21].
In a study by Yasein and co-workers, only 34.8% of the study population showed full concordance between the self-reported number of drugs and the number of drugs in the medical records [22]. The rest of the patients either underestimated (43.4%) or overestimated (21.8%) the number of drugs, without differences between male and female patients [22]. Analogous results were obtained by Zwietering and colleagues, who reported that the number of medications patients stated to use only agreed in approximately 30% to the number of drugs listed in their medication charts [23].
In our study, 95% of patients used their medication charts as support. Freyer et al. found that use of a medication chart is associated with better medication knowledge, and that higher age is associated with less medication knowledge [6], consistent with our results. Freyer and colleagues also noted that medication charts frequently were not up-to-date [6]. Most of the medication charts used by our study participants were professional medication schedules created by patients’ GPs; however, sometimes hospital discharge letters, handwritten tables, (empty) drug packagings with handwritten notes on top, or even smartphone photos were used as “medication charts” by the patients. All of these modalities certainly aided participants in answering our study questionnaire and likely were superior to not using a medication chart at all. Yet, for the purpose of pharmacotherapy safety and a quicker and better overview for attending physicians, it would be desirable—as stipulated in the German eHealth Act (E-Health-Gesetz) from 2015 [24]—to use a nationally standardized (electronic) format for medication charts and to regularly update medication charts.
Despite the overall encouraging results of our study (median of 5 for the average medication knowledge score on a scale from 0 to 6), there is still room for improvement of patients’ medication education, especially among male patients and among patients ≥ 80 years. This is important because the number of German inhabitants aged 85 or older is rapidly growing. Since 1991, their number more than doubled from 1.2 million to 2.6 million by 2021 [25]. This demographic challenge requires enormous efforts by all healthcare workers to safeguard adequate pharmacotherapy and healthcare for older people [22].
In 2008, Modig et al. stated that older people only rarely use the Internet as a source of information about their medication [26], a notion which appears to be corroborated by our study in which only 3% of participants stated that the Internet contributed most to their medication knowledge. Other media such as television and the press were even less represented (0% and 1%, respectively). It is noteworthy that in the media era of the 21th century 69% of participants in our study reported that physicians (GPs but also medical specialists) contributed most to their medication knowledge. Pharmacists, by contrast, apparently did not contribute significantly to patients’ medication knowledge in the present study. It must be noted that we did not specifically explore which source(s) of information participants considered as trustworthy. Older persons’ level of trust in different sources of information should be the subject of future follow-up studies.
The implementation of sick day rules was assessed by NHS Highland for drugs used in the treatment of common diseases of older people (e.g., arterial hypertension, chronic heart failure, diabetes mellitus type 2) [14, 15] but also more specifically for patients with endocrine disorders by Pal and Bhadada [27]. Malik and colleagues issued recommendations for adjusting medication regimens for patients with chronic kidney disease who fast during Ramadan [28]. The cited studies not only emphasized the usefulness of sick day rules, but also made suggestions on how, when, and by whom sick day rules should be communicated to patients [14, 15, 27, 28]. By contrast, only few studies investigated patients’ awareness of sick day rules. Salehmohamed et al. reported that knowledge of sick day rules may differ between patients being treated with the same class of medication (in their study corticosteroids) but for different indications [8]. Our findings reveal major knowledge deficits of older patients regarding options for medication adjustment during episodes of acute illness. To the best of our knowledge, physicians’ awareness of sick day rules has not been investigated to date but should be assessed in future studies as it might significantly influence patients’ awareness of sick day rules.
Older patients are generally more susceptible to adverse effects of drugs due to altered pharmacokinetics and pharmacodynamics [29]. Potentially life-threatening events such as acute kidney injury might be prevented if drugs such as diuretics, angiotensin-converting enzyme inhibitors, angiotensin receptor blockers, or non-steroidal anti-inflammatory drugs are temporarily discontinued during intercurrent illness, but also during radiological or surgical procedures, although the evidence base for this recommendation is limited [11, 30]. Nonetheless, sick-day rules have been widely propagated for use in primary care by NHS Scotland and the Scottish Patient Safety Programme [13,14,15].
Although Morris et al. reported that patients who were actively engaged in their medication management expressed greater confidence [10], standardized strategies to inform patients about sick day rules do not exist to date. Morris et al. stated that simply handing out a sick day rule plan to patients was insufficient and saw the need for a “wider, collective, [sic] commitment” and for a “clarity in roles and responsibilities” in the future [10]. It is of paramount importance to define who will take over responsibility for this task and at what timepoint in the medication process [10].
Possible ways to make patients aware of the need of medication adjustment are IT system reminders [10], MedicAlert bracelets, or awareness cards, which are already used by some patients treated with corticosteroids in Ireland [8]. In the Morris et al. study, applying highlighted stickers on the back of drug packagings of drugs for which sick day rules are applicable, together with 5-min briefings, was suggested as a possible solution, but also judged as too time-consuming as this would be necessary for every patient taking drugs that can be adjusted during acute illness [10].
Limitations of our study mainly arise from its monocentric setting and the relatively small number of patients enrolled, limiting the generalizability and transferability of our results to other healthcare settings and geographical regions. Although the questionnaire used in our study was not formally validated, a pretest was conducted to ensure the study questionnaire’s applicability under real-world conditions in a hospital setting.
In conclusion, our study showed that medication knowledge of older patients was overall satisfying. Use of a medication chart may have contributed substantially to the sound medication knowledge in our study population. Awareness of sick day rules, however, was poor. Future studies should evaluate the clinical benefits of sick day rules and ways of better communicating sick day rules to patients. In this regard, general practitioners may play a decisive role.
Availability of data and materials
The data that support the findings of this study are available upon reasonable request from the corresponding author.
References
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE (2017) What is polypharmacy? BMC Geriatr, A systematic review of definitions. https://doi.org/10.1186/s12877-017-0621-2
Mosshammer D, Haumann H, Morike K, Joos S (2016) Polypharmacy—an upward trend with unpredictable effects. Dtsch Arztebl Int. https://doi.org/10.3238/arztebl.2016.0627
Centers for Disease Control and Prevention (2022) Health Literacy—Medications. https://www.cdc.gov/healthliteracy/researchevaluate/medications.html. Accessed 17 May 2023
Timmerman L, Stellema R, Stronks DL, Groeneweg G, Huygen FJPM (2014) Adherence to pharmacological pain therapy in patients with nonmalignant pain: the role of patients’ knowledge of pain medication. Pain Pract. https://doi.org/10.1111/papr.12139
Chan FW, Wong FY, So WY, Kung K, Wong CK (2013) How much do elders with chronic conditions know about their medications? BMC Geriatr. https://doi.org/10.1186/1471-2318-13-59
Freyer J, Greißing C, Buchal P, Kabitz H, Kasprick L, Schuchmann M, Sultzer R, Schiek S, Bertsche T (2016) Discharge medication—what do patients know about their medication on discharge? Dtsch Med Wochenschr. https://doi.org/10.1055/s-0042-108618
Krause O, Glaubitz S, Hager K, Schleef T, Wiese B, Junius-Walker U (2020) Post-discharge adjustment of medication in geriatric patients: A prospective cohort study. Z Gerontol Geriatr. https://doi.org/10.1007/s00391-019-01601-8
Salehmohamed MR, Griffin M, Branigan T, Cuesta M, Thompson CJ (2018) Patients treated with immunosuppressive steroids are less aware of sick day rules than those on endocrine replacement therapy and may be at greater risk of adrenal crisis. Ir J Med Sci. https://doi.org/10.1007/s11845-017-1607-y
Keller F (2021) Adverse Drug Effects—how to detect, how to avoid? Dtsch Med Wochenschr. https://doi.org/10.1055/a-1116-5210
Morris RL, Ashcroft D, Phipps D, Bower P, O’Donoghue D, Roderick P, Harding S, Lewington A, Blakeman T (2016) Preventing Acute Kidney Injury: a qualitative study exploring “sick day rules” implementation in primary care. BMC Fam Pract. https://doi.org/10.1186/s12875-016-0480-5
Whiting P, Morden A, Tomlinson LA, Caskey F, Blakeman T, Tomson C, Stone T, Richards A, Savović J, Horwood J (2017) What are the risks and benefits of temporarily discontinuing medications to prevent acute kidney injury? A systematic review and meta-analysis. BMJ Open. https://doi.org/10.1136/bmjopen-2016-012674
Elshimy G, Chippa V, Jeong JM (2022) Adrenal Crisis. In: StatPearls. StatPearls Publishing LLC, Treasure Island (FL)
Scottish Patient Safety Programme (2013) Primary Care Medicines Sick Day Rules Card. https://ihub.scot/improvement-programmes/scottish-patient-safety-programme-spsp/spsp-programmes-of-work/spsp-medicines-collaborative/high-risk-situations-involving-medicines/medicines-sick-day-rules-card/. Accessed 21 Aug 2022
Morrison C, Wilson M (2014) Medicine Sick Day Rules Cards – Interim Evaluation. https://ihub.scot/media/5915/nhsh-interim-evaluation-medicine-sick-day-rules.pdf. Accessed 21 Aug 2022
Morrison C, Wilson M (2015) Medicine Sick Day Rules cards: a safe and effective tool to improve medicines safety in NHS Highland. Int J Pharm Pract. https://doi.org/10.1111/ijpp.12213
Diabetes Canada (2018) Appendix 8 Sick-Day Medication List. https://guidelines.diabetes.ca/cpg/appendices/appendix8. Accessed 21 Aug 2022
Bamgboye AO, Oni IO, Collier A (2021) Predisposing factors for the development of diabetic ketoacidosis with lower than anticipated glucose levels in type 2 diabetes patients on SGLT2-inhibitors: a review. Eur J Clin Pharmacol. https://doi.org/10.1007/s00228-020-03051-3
Federal Institute for Drugs and Medical Devices (2022) ATC-Classification. https://www.bfarm.de/EN/Code-systems/Classifications/ATC/_node.html. Accessed 31 Dec 2022
Okuyan B, Sancar M, Izzettin FV (2013) Assessment of medication knowledge and adherence among patients under oral chronic medication treatment in community pharmacy settings. Pharmacoepidemiol Drug Saf. https://doi.org/10.1002/pds.3275
Okuyan B, Sancar M, Izzettin FV, Morisky DE (2013) Erratum to and corrections on the article entitled “Assessment of medication knowledge and adherence among patients under oral chronic medication treatment in community pharmacy settings.” Pharmacoepidemiol Drug Saf. https://doi.org/10.1002/pds.3394
Sancar M, Yalcin Mutlu B, Okuyan B, Vehbi Izzettin F (2011) Determination of geriatric patients’ drug profile and identify their pharmaceutical care requirements by determining potential risk factors. European Geriatric Medicine. https://doi.org/10.1016/j.eurger.2011.07.011
Yasein NA, Barghouti FF, Irshaid YM, Suleiman AA (2013) Discrepancies between elderly patient’s self-reported and prescribed medications: a social investigation. Scand J Caring Sci. https://doi.org/10.1111/j.1471-6712.2012.01012.x
Zwietering NA, Westra D, Winkens B, Cremers H, van der Kuy PHM, Hurkens KP (2019) Medication in older patients reviewed multiple ways (MORE) study. Int J Clin Pharm. https://doi.org/10.1007/s11096-019-00879-3
Bundesministerium für Gesundheit (2022) E-Health-Gesetz. https://www.bundesgesundheitsministerium.de/service/begriffe-von-a-z/e/e-health-gesetz.html. Accessed 05 May 2023
Statistisches Bundesamt (2023) Ältere Menschen. https://www.destatis.de/DE/Themen/Querschnitt/Demografischer-Wandel/Aeltere-Menschen/bevoelkerung-ab-65-j.htm. Accessed 05 May 2023
Modig S, Kristensson J, Ekwall AK, Hallberg IR, Midlöv P (2009) Frail elderly patients in primary care—their medication knowledge and beliefs about prescribed medicines. Eur J Clin Pharmacol. https://doi.org/10.1007/s00228-008-0581-8
Pal R, Bhadada SK (2020) Managing common endocrine disorders amid COVID-19 pandemic. Diabetes Metab Syndr. https://doi.org/10.1016/j.dsx.2020.05.050
Malik S, Bhanji A, Abuleiss H, Hamer R, Shah SH, Rashad R, Junglee N, Waqar S, Ghouri N (2021) Effects of fasting on patients with chronic kidney disease during Ramadan and practical guidance for healthcare professionals. Clin Kidney J. https://doi.org/10.1093/ckj/sfab032
Davies EA, O’Mahony MS (2015) Adverse drug reactions in special populations—the elderly. Br J Clin Pharmacol. https://doi.org/10.1111/bcp.12596
Sykes L, Nipah R, Kalra P, Green D (2018) A narrative review of the impact of interventions in acute kidney injury. J Nephrol. https://doi.org/10.1007/s40620-017-0454-2
Acknowledgements
Benjamin Krichevsky and Johannes Heck dedicate this article to their inspiring former teacher Dr. Richard Wagner, University Hospital Würzburg, Free State of Bavaria, Germany.
Funding
Open Access funding enabled and organized by Projekt DEAL. There are no funders to report for this submission.
Author information
Authors and Affiliations
Contributions
OK, CTZ, JH: conceptualized the study. CTZ: conducted the interviews. CTZ, JH: performed the statistical analyses. OK, CTZ, JH: interpreted the study results. CTZ, JH: drafted the first version of the manuscript, created the tables and figures. MSW, SS, BK, SG, DOS: assisted with the preparation of the manuscript. JH: supervised the project. All authors: commented on previous versions of the manuscript, read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethical approval
This study was approved by the Ethics Committee of Hannover Medical School (No. 10274_BO_K_2022; date of approval: 11 March 2022) and adheres to the Declaration of Helsinki (1964) and its later amendments (current version dating from 2013).
Consent to participate
All patients provided written informed consent to participate in this study.
Consent to publish
All patients provided written informed consent that their patient-related data may be used for publications.
Competing interests
The authors state that they have no conflicts of interest to declare.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Olaf Krause and Corinna T. Ziemann are joint first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Krause, O., Ziemann, C.T., Schulze Westhoff, M. et al. What do older patients know about their medication? A cross-sectional, interview-based pilot study. Eur J Clin Pharmacol 79, 1365–1374 (2023). https://doi.org/10.1007/s00228-023-03548-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-023-03548-7