Abstract
Purpose
Our aim was to determine the impact of potentially inappropriate prescriptions (PIP), according to “Screening Tool of Older Persons’ Prescriptions” criteria version 2 (STOPP-2), on mortality and hospital admissions.
Methods
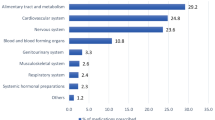
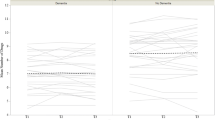
Monocentric retrospective cohort study. Patients over 65 years of age and who were consecutively discharged from internal medicine at a Spanish university hospital in 2016 were included. The mortality and hospital admissions of the cohort of patients were analysed using their electronic health records within two years from the time of discharge. Analysis was done based on the type and number of STOPP-2 criteria as well as taking into account the total number of medications. The subdistribution hazard ratios (SHR) were estimated through a competing proportional hazards model.
Results
A total of 270 patients with a median age of 82 years (interquartile range/IQR 76–86 years), and 152 (56.3%) women were studied. It was found out that 28.3% of patients with PIP died compared to 17.2% of patients without it. Digoxin (B1 STOPP-2 criterion) with a subdistribution hazard ratio (SHR) 2.40 (95% CI 0.63–9.18), selective serotonin re-uptake inhibitors/SSRIs (D4) with a SHR 1.76 (95% CI 0.52–5.96) and neuroleptic drugs (K2) with a SHR 2.01 (95% CI 0.82–4.95) non-significantly increased the risk of death. Dementia (SHR 5.45; 95% CI 2.76–10.78) was then the only statistically significant risk factor for death. Sixty percent of patients with a PIP had shown at least one hospital admission compared to 51% of patients without it. The number of drugs at discharge (SHR 1.03; 95% CI 1.01–1.05) and having 1–2 STOPP-2 criteria (SHR 1.17; 95% CI 1.02–1.35) significantly increased the risk of hospital admission.
Conclusion
The number of drugs at discharge and having any STOPP criteria significantly increased the risk of hospital admission in this cohort. PIP, only according to some specific STOPP-2 criteria involving digoxin, neuroleptics and SSRIs, might associate with a statistically non-significantly higher risk on mortality.
Similar content being viewed by others
Availability of data and material
The datasets generated during and/or analysed during the study are available from the corresponding author subject to a reasonable request.
References
Boeker EB, de Boer M, Kiewiet JJ, Lie-A-Huen L, Dijkgraaf MG, Boermeester MA (2013) Occurrence and preventability of adverse drug events in surgical patients: a systematic review of literature. BMC Health Serv Res 13:364
Hug BL, Keohane C, Seger DL, Yoon C, Bates DW (2012) The costs of adverse drug events in community hospitals. Jt Comm J Qual Patient Saf 38(3):120–126
Kalisch Ellett LM, Pratt NL, Ramsay EN, Barratt JD, Roughead EE (2014) Multiple anticholinergic medication use and risk of hospital admission for confusion or dementia. J Am Geriatr Soc 62(10):1916–1922
Khan LM (2013) Comparative epidemiology of hospital-acquired adverse drug reactions in adults and children and their impact on cost and hospital stay--a systematic review. Eur J Clin Pharmacol 69(12):198596
Leporini C, De Sarro G, Russo E (2014) Adherence to therapy and adverse drug reactions: is there a link? Expert Opin Drug Saf 13(Suppl 1):S41-55
Gallagher P, Ryan C, Byrne S, Kennedy J, O’Mahony D (2008) STOPP (Screening Tool of Older Person’s Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment). Consensus validation Int J Clin Pharmacol Ther 46(2):72–83
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44(2):213–218
Delgado Silveira E, Montero Errasquín B, Muñoz García M et al (2015) Improving drug prescribing in the elderly: a new edition of STOPP/START criteria. Rev Esp Geriatr Gerontol 50(2):89–96
Pardo-Cabello AJ, Manzano-Gamero V, Zamora-Pasadas M et al (2018) Potentially inappropriate prescribing according to STOPP-2 criteria among patients discharged from Internal Medicine: prevalence, involved drugs and economic cost. Arch Gerontol Geriatr 74:150–154
Counter D, Millar JWT, McLay JS (2018) Hospital readmissions, mortality and potentially inappropriate prescribing: a retrospective study of older adults discharged from hospital. Br J Clin Pharmacol 84:1757–1763
Brunetti E, Aurucci ML, Boietti E, et al (2019) Clinical implications of potentially inappropriate prescribing according to STOPP/START version 2 criteria in older polymorbid patients discharged from geriatric and internal medicine wards: a prospective observational multicenter study. J Am Med Dir Assoc S1525–8610(19):30318–4
Thomas RE, Nguyen LT, Jackson D, Naugler C (2020) potentially inappropriate prescribing and potential prescribing omissions in 82,935 older hospitalised adults: association with hospital readmission and mortality within six months. Geriatrics (Basel) 5:37. https://doi.org/10.3390/geriatrics5020037
Hudhra K, Beçi E, Petrela E, Xhafaj D, García-Caballos M, Bueno-Cavanillas A (2016) Prevalence and factors associated with potentially inappropriate prescriptions among older patients at hospital discharge. J Eval Clin Pract 22(5):707–713
Fine JP, Gray RJ (1999) A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 94:496–509
Mekonnen AB, Redley B, de Courten B, Manias E (2021) Potentially inappropriate prescribing and its associations with health-related and system-related outcomes in hospitalised older adults: a systematic review and meta-analysis. Br J Clin Pharmacol 1–23. https://doi.org/10.1111/bcp.14870
Vamos M, Erath JW, Benz AP, Lopes RD, Hohnloser SH (2019) Meta-analysis of effects of digoxin on survival in patients with atrial fibrillation or heart failure: an update. Am J Cardiol 123:69–74
Acknowledgements
The authors thank Shari Meyan Fae Barro for improving the English style.
Author information
Authors and Affiliations
Contributions
AJPC and JDL contributed to the conception or design of the work and/or to the acquisition of data. JDL, AJPC and VMG contributed to the analysis and/or interpretation of results. AJPC and VMG drafted the manuscript. AJPC and VMG carefully revised the manuscript. All authors gave final approval and agree to be accountable for all aspects of the work ensuring integrity and accuracy.
Corresponding author
Ethics declarations
Ethics approval
Given the observational and retrospective nature of the study, and the anonymity of all patients whom clinical data were used, approval by the ethics committee was not requested.
Research involving human participants and/or animals
This observational study was conducted retrospectively from electronic data exclusively obtained for clinical purposes.
Informed consent
Informed consent is not required because of the retrospective and observational nature of study, because the information is anonymized, and the submission does not include data or images that may identify the people.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pardo-Cabello, A.J., Manzano-Gamero, V. & Luna, J.d. The impact of PIPs on mortality and readmissions in older adults: a retrospective cohort study. Eur J Clin Pharmacol 78, 139–145 (2022). https://doi.org/10.1007/s00228-021-03217-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03217-7