Abstract
Purpose
To establish a consensus on both explicit and implicit criteria in order to identify potentially inappropriate prescribing (PIP) in French older people aged 75 years and over or 65 years and over with multimorbidity.
Methods
Fifteen experts in geriatrics, general practice, pharmacy, and clinical pharmacology were involved in a two-round Delphi survey to assess preliminary explicit and implicit criteria based on an extensive literature review and up-to-date evidence data. Experts were asked to rate their level of agreement using a 5-level Likert scale for inclusion of criteria and also for rationale and therapeutic alternatives. A consensus was considered as reached if at least 75% of the experts rated criteria as “strongly agreed” or “agreed.”
Results
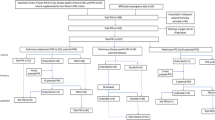
The new tool included a seven-step algorithm (implicit criteria) encompassing the three main domains that define PIP (i.e. overprescribing, underprescribing, and misprescribing) and 104 explicit criteria. Explicit criteria were divided into 6 tables related to inappropriate drug duplications (n = 7 criteria), omissions of medications and/or medication associations (n = 16), medications with an unfavourable benefit/risk ratio and/or a questionable efficacy (n = 39), medications with an unsuitable dose (n = 4) or duration (n = 6), drug-disease (n = 13), and drug-drug interactions (n = 19).
Conclusion
The REMEDI[e]S tool (REview of potentially inappropriate MEDIcation pr[e]scribing in Seniors) is an original mixed tool, adapted to French medical practices, aimed at preventing PIP both at the individual level in clinical practice and the population level in large-scale studies. Therefore, its use could contribute to an improvement in healthcare professionals’ prescribing practices and safer care in older adults.

Similar content being viewed by others
References
Hamilton HJ, Gallagher PF, O’Mahony D (2009) Inappropriate prescribing and adverse drug events in older people. BMC Geriatr 9:5
Mangoni AA, Jackson SHD (2004) Age-related changes in pharmacokinetics and pharmacodynamics: basic principles and practical applications. Br J Clin Pharmacol 57:6–14
Merle L, Laroche M-L, Dantoine T et al (2005) Predicting and preventing adverse drug reactions in the very old. Drugs Aging 22:375–392
Nair NP, Chalmers L, Peterson GM et al (2016) Hospitalization in older patients due to adverse drug reactions; the need for a prediction tool. Clin Interv Aging 497
Dimitrow MS, Airaksinen MSA, Kivelä S-L et al (2011) Comparison of prescribing criteria to evaluate the appropriateness of drug treatment in individuals aged 65 and older: a systematic review. J Am Geriatr Soc 59:1521–1530
O’Connor MN, Gallagher P, O’Mahony D (2012) Inappropriate prescribing: criteria, detection and prevention. Drugs Aging 29:437–452
Motter FR, Fritzen JS, Hilmer SN et al (2018) Potentially inappropriate medication in the elderly: a systematic review of validated explicit criteria. Eur J Clin Pharmacol 74:679–700
Kaufmann CP, Tremp R, Hersberger KE et al (2014) Inappropriate prescribing: a systematic overview of published assessment tools. Eur J Clin Pharmacol 70:1–11
Desnoyer A, Guignard B, Lang P-O et al (2016) Potentially inappropriate medications in geriatrics: which tools to detect them? Presse Med 45:957–970
Poudel A, Ballokova A, Hubbard RE et al (2016) Algorithm of medication review in frail older people: focus on minimizing the use of high-risk medications. Geriatr Gerontol Int 16:1002–1013
Zacarin A, Strumia M, Piau A et al (2020) (2020) Potentially inappropriate medication: adaptation of EU(7)PIM criteria to the French medical practice. Therapie Nov-Dec 75(6):663–673
Pazan F, Kather J, Wehling M (2019) A systematic review and novel classification of listing tools to improve medication in older people. Eur J Clin Pharmacol 75:619–625
Mangin D, Bahat G, Golomb BA et al (2018) International Group for Reducing Inappropriate Medication Use & Polypharmacy (IGRIMUP): position statement and 10 recommendations for action. Drugs Aging 35:575–587
Laroche M-L, Charmes J-P, Merle L (2007) Potentially inappropriate medications in the elderly: a French consensus panel list. Eur J Clin Pharmacol 63:725–731
Lucchetti G, Lucchetti ALG (2017) Inappropriate prescribing in older persons: a systematic review of medications available in different criteria. Arch Gerontol Geriatr 68:55–61
Opondo D, Eslami S, Visscher S et al (2012) Inappropriateness of medication prescriptions to elderly patients in the primary care setting: a systematic review. PLoS One 7:e43617
Storms H, Marquet K, Aertgeerts B et al (2017) Prevalence of inappropriate medication use in residential long-term care facilities for the elderly: a systematic review. Eur J Gen Pract 23:69–77
Hill-Taylor B, Sketris I, Hayden J et al (2013) Application of the STOPP/START criteria: a systematic review of the prevalence of potentially inappropriate prescribing in older adults, and evidence of clinical, humanistic and economic impact. J Clin Pharm Ther 38:360–372
O’Mahony D, O’Sullivan D, Byrne S et al (2015) STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing 44:213–218
Tommelein E, Petrovic M, Somers A et al (2016) Older patients’ prescriptions screening in the community pharmacy: development of the Ghent Older People’s Prescriptions community Pharmacy Screening (GheOP3S) tool. J Public Health 38:e158-170
Drenth-van Maanen AC, van Marum RJ, Knol W et al (2009) Prescribing optimization method for improving prescribing in elderly patients receiving polypharmacy: results of application to case histories by general practitioners. Drugs Aging 26:687–701
Basger BJ, Chen TF, Moles RJ (2012) Validation of prescribing appropriateness criteria for older Australians using the RAND/UCLA appropriateness method. BMJ Open. https://doi.org/10.1136/bmjopen-2012-001431
Wenger NS, Roth CP, Shekelle P et al (2007) Introduction to the assessing care of vulnerable elders-3 quality indicator measurement set. J Am Geriatr Soc 55(Suppl 2):S247-252
Wang-Hansen MS, Wyller TB, Hvidsten LT et al (2019) Can screening tools for potentially inappropriate prescriptions in older adults prevent serious adverse drug events? Eur J Clin Pharmacol 75:627–637
Nobili A, Pasina L, Tettamanti M et al (2009) Potentially severe drug interactions in elderly outpatients: results of an observational study of an administrative prescription database. J Clin Pharm Ther 34:377–386
Oscanoa TJ, Lizaraso F, Carvajal A (2017) Hospital admissions due to adverse drug reactions in the elderly. A meta-analysis. Eur J Clin Pharmacol 73:759–770
Pedrós C, Formiga F, Corbella X et al (2016) Adverse drug reactions leading to urgent hospital admission in an elderly population: prevalence and main features. Eur J Clin Pharmacol 72:219–226
Schmiedl S, Rottenkolber M, Szymanski J et al (2018) Preventable ADRs leading to hospitalization - results of a long-term prospective safety study with 6,427 ADR cases focusing on elderly patients. Expert Opin Drug Saf 17:125–137
Santos TRA, Silveira EA, Pereira LV et al (2017) Potential drug-drug interactions in older adults: a population-based study. Geriatr Gerontol Int 17:2336–2346
Malone DC, Abarca J, Hansten PD et al (2004) Identification of serious drug-drug interactions: results of the partnership to prevent drug-drug interactions. J Am Pharm Assoc 44:142–151
Lindblad CI, Hanlon JT, Gross CR et al (2006) Clinically important drug-disease interactions and their prevalence in older adults. Clin Ther 28:1133–1143
Haute Autorité de Santé (HAS) (2012) Indicateurs de Pratique Clinique (IPC PMSA). https://www.has-sante.fr/jcms/c_1250626/fr/indicateurs-de-pratique-clinique-ipc-pmsa. Accessed 11 Aug 2020
Singh S, Bajorek B (2014) Defining ‘elderly’ in clinical practice guidelines for pharmacotherapy. Pharm Pract (Granada) 12:489
Marriott J, Stehlik P (2012) A critical analysis of the methods used to develop explicit clinical criteria for use in older people. Age Ageing 41:441–450
Campbell SM, Cantrill JA (2001) Consensus methods in prescribing research. J Clin Pharm Ther 26:5–14
McMillan SS, King M, Tully MP (2016) How to use the nominal group and Delphi techniques. Int J Clin Pharm. https://doi.org/10.1007/s11096-016-0257-x
Diamond IR, Grant RC, Feldman BM et al (2014) Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J Clin Epidemiol 67:401–409
Desnoyer A, Blanc A-L, Pourcher V et al (2017) PIM-Check: development of an international prescription-screening checklist designed by a Delphi method for internal medicine patients. BMJ Open 7:e016070
Spinewine A, Swine C, Dhillon S et al (2007) Effect of a collaborative approach on the quality of prescribing for geriatric inpatients: a randomized, controlled trial. J Am Geriatr Soc 55:658–665
Laroche M-L, Sirois C, Reeve E et al (2019) Pharmacoepidemiology in older people: purposes and future directions. Therapie 74:325–332
Reeve E, Farrell B, Thompson W et al (2019) Deprescribing cholinesterase inhibitors and memantine in dementia: guideline summary. Med J Aust 210:174–179
Russ TC, Morling JR (2012) Cholinesterase inhibitors for mild cognitive impairment. Cochrane Database Syst Rev CD009132
Renom-Guiteras A, Meyer G, Thürmann PA (2015) The EU(7)-PIM list: a list of potentially inappropriate medications for older people consented by experts from seven European countries. Eur J Clin Pharmacol 71:861–875
Pazan F, Weiss C, Wehling M et al (2018) The EURO-FORTA (Fit fOR The Aged) list: international consensus validation of a clinical tool for improved drug treatment in older people. Drugs Aging 35:61–71
Matanović SM, Vlahovic-Palcevski V (2012) Potentially inappropriate medications in the elderly: a comprehensive protocol. Eur J Clin Pharmacol 68:1123–1138
Kim M-Y, Etherton-Beer C, Kim C-B et al (2018) Development of a consensus list of potentially inappropriate medications for Korean older adults. Ann Geriatr Med Res 22:121–129
Harmand MGC, Aldea-Perona AM, Del Campo CBF et al (2019) Spanish list of potentially inappropriate drugs in the elderly (ES-PIA project). Eur J Clin Pharmacol. https://doi.org/10.1007/s00228-019-02684-3
By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel (2019) American Geriatrics Society 2019 updated AGS Beers Criteria® for potentially inappropriate medication use in older adults. J Am Geriatr Soc 67:674–694
Boulkedid R, Abdoul H, Loustau M et al (2011) Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS One 6:e20476
Spinewine A, Schmader KE, Barber N et al (2007) Appropriate prescribing in elderly people: how well can it be measured and optimised? Lancet 370:173–184
Wang K, Shen J, Jiang D et al (2019) Development of a list of high-risk perioperative medications for the elderly: a Delphi method. Expert Opin Drug Saf 18:853–859
Keijsers CJPW, van Doorn ABD, van Kalles A et al (2014) Structured pharmaceutical analysis of the systematic tool to reduce inappropriate prescribing is an effective method for final-year medical students to improve polypharmacy skills: a randomized controlled trial. J Am Geriatr Soc 62:1353–1359
Hill-Taylor B, Walsh KA, Stewart S et al (2016) Effectiveness of the STOPP/START (Screening Tool of Older Persons’ potentially inappropriate Prescriptions/Screening Tool to Alert doctors to the Right Treatment) criteria: systematic review and meta-analysis of randomized controlled studies. J Clin Pharm Ther 41:158–169
Brown JD, Hutchison LC, Li C et al (2016) Predictive validity of the Beers and Screening Tool of Older Persons’ Potentially Inappropriate Prescriptions (STOPP) criteria to detect adverse drug events, hospitalizations, and Emergency Department Visits in the United States. J Am Geriatr Soc 64:22–30
Parekh N, Ali K, Davies JG et al (2019) Do the 2015 Beers Criteria predict medication-related harm in older adults? Analysis from a multicentre prospective study in the United Kingdom. Pharmacoepidemiol Drug Saf 28:1464–1469
Kympers C, Tommelein E, Van Leeuwen E et al (2019) Detection of potentially inappropriate prescribing in older patients with the GheOP3S-tool: completeness and clinical relevance. Acta Clin Belg 74:126–136
Gallagher P, Baeyens J-P, Topinkova E et al (2009) Inter-rater reliability of STOPP (Screening Tool of Older Persons’ Prescriptions) and START (Screening Tool to Alert doctors to Right Treatment) criteria amongst physicians in six European countries. Age Ageing 38:603–606
Ivanova I, Elseviers M, Wauters M et al (2018) European repository of explicit criteria of potentially inappropriate medications in old age. Geriatr Gerontol Int 18:1293–1297
Monteiro L, Maricoto T, Solha I et al (2019) Reducing potentially inappropriate prescriptions for older patients using computerized decision support tools: systematic review. J Med Internet Res 21:e15385
Dalton K, O’Brien G, O’Mahony D et al (2018) Computerised interventions designed to reduce potentially inappropriate prescribing in hospitalised older adults: a systematic review and meta-analysis. Age Ageing 47:670–678
Acknowledgements
We would like to acknowledge the assistance of Prof Louis Merle, professor emeritus of clinical pharmacology, Faculty of Medicine of Limoges, for his attentive and critical review of the manuscript.
Author information
Authors and Affiliations
Contributions
BR and MLL conceived and designed the study; BR screened the literature; BR and MLL drafted preliminary criteria; BR conducted the Delphi survey; BR and MLL analyzed the data; JBC, JBB, MCB, JD, JPF, BG, SG, RG, VG, MG, PN, EP, KR, MBVR, and TT participated in the Delphi consensus as experts; BR and MLL interpreted the data. All authors revised the manuscript and approved the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Roux, B., Berthou-Contreras, J., Beuscart, JB. et al. REview of potentially inappropriate MEDIcation pr[e]scribing in Seniors (REMEDI[e]S): French implicit and explicit criteria. Eur J Clin Pharmacol 77, 1713–1724 (2021). https://doi.org/10.1007/s00228-021-03145-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-021-03145-6