Abstract
Purpose
This study aimed to explore medication-related decision-making by health professionals from different disciplines and specialties caring for people with advanced dementia living in long-term care facilities, focusing on dilemmas associated with starting, continuing or deprescribing medications commonly regarded as potentially inappropriate.
Methods
Four focus groups were undertaken, each on a different medication type (antibiotics, lipid-lowering agents, opioids and acetylcholinesterase inhibitors). Transcripts underwent qualitative analysis using line by line inductive coding and then a person-centred framework to highlight themes across medication types.
Results
Sixteen participants participated in focus groups. Regardless of medication type or dilemma, results suggested decision-making for residents with advanced dementia should begin with discussing goals of care and engaging with families, and be viewed as an iterative process involving regular monitoring and adjustment. Decision-making was seen as requiring a dialectical approach involving multiple perspectives, with an emphasis on establishing communication between health professionals, family and the person with dementia to better understand goals/preferences for care.
Conclusion
Inter-professional collaboration enables sharing of clinical experience/expertise, differing disciplinary perspectives and knowledge about the resident. Continuing a medication should be considered an active decision that carries as much responsibility as starting or deprescribing.
Similar content being viewed by others
References
Van Der Steen J, Radbruch L, Hertogh C, De Boer M, Hughes J, Larkin P et al (2014) White paper defining optimal palliative care in older people with dementia: a Delphi study and recommendations from the European Association for Palliative Care. Palliat Med 28(3):197–209
Prince M, Comas-Herrera A, Knapp M, Guerchet M, Karagiannidou M (2016) World Alzheimer report 2016: improving healthcare for people living with dementia: coverage, quality and costs now and in the future
Birch D, Draper J (2008) A critical literature review exploring the challenges of delivering effective palliative care to older people with dementia. J Clin Nurs 17(9):1144–1163
Parsons C, Hughes C, Passmore A, Lapane K (2010) Withholding, discontinuing and withdrawing medications in dementia patients at the end of life: a neglected problem in the disadvantaged dying? Drugs Aging 27(6):435–449. https://doi.org/10.2165/11536760-000000000-00000
Parsons C, McCorry N, Murphy K, Byrne S, O’sullivan D, O’mahony D et al (2014) Assessment of factors that influence physician decision making regarding medication use in patients with dementia at the end of life. Int J Geriatr Psych 29(3):281–290
Shega J, Ellner L, Lau D, Maxwell T (2009) Cholinesterase inhibitor and N-methyl-D-aspartic acid receptor antagonist use in older adults with end-stage dementia: a survey of hospice medical directors. J Palliat Med 12(9):779–783
Holmes H. (2009) Rational prescribing for patients with a reduced life expectancy. Clin Pharmacol Ther 85(1)
Ostini R, Hegney D, Jackson C, Tett S (2012) Knowing how to stop: ceasing prescribing when the medicine is no longer required. J Manag Care Pharm 18(1):68–72
NHMRC Cognitive Decline Partnership Centre, University of Sydney, in collaboration with the Australian Deprescribing Network and NPS MedicineWise. Quality Use of Medicines to Optimise Ageing in Older Australians: recommendations for a national strategic action plan to reduce inappropriate polypharmacy. Sydney, NSW, Australia; 2018
Paque K, Vander Stichele R, Elseviers M, Pardon K, Dilles T, Deliens L, Christiaens T (2018) Barriers and enablers to deprescribing in people with a life-limiting disease: a systematic review. Palliat Med 33(1):37–48
Flanagan J (1954) The critical incident technique. Psychol Bull 51(4):327–358
Bendtsen P, Hensing G, McKenzie L, Stridsman A-K (1999) Prescribing benzodiazepines—a critical incident study of a physician dilemma. Soc Sci Med 49(4):459–467
Bendtsen P, Hensing G, Ebeling C, Schedin A (1999) What are the qualities of dilemmas experienced when prescribing opioids in general practice? Pain. 82(1):89–96
Tong A, Sainsbury P, Craig J (2007) Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care 19(6):349–357
Westbury J, Gee P, Ling T, Brown D, Franks K, Bindoff I, Bindoff A, Peterson GM (2018) RedUSe: reducing antipsychotic and benzodiazepine prescribing in residential aged care facilities. Med J Aust 208(9):398–403
Brodaty H, Aerts L, Harrison F, Jessop T, Cations M, Chenoweth L, Shell A, Popovic GC, Heffernan M, Hilmer S, Sachdev PS, Draper B (2018) Antipsychotic deprescription for older adults in long-term care: the HALT study. J Am Med Dir Assoc 19(7):592–600
Kemppainen J (2000) The critical incident technique and nursing care quality research. J Adv Nurs 32(5):1264–1271
Nielsen J, Clemmensen T, Yssing C (2002) Getting access to what goes on in people’s heads?: reflections on the think-aloud technique. Proceedings of the second Nordic conference on Human-computer interaction :101–100 ACM
Eklund JH, Holmström I, Kumlin T, Kaminsky E, Skoglund K, Höglander J et al (2019) “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Education and Counseling 102(1):3–11
Crotty M, Halbert J, Rowett D, Giles L, Birks R, Williams H, Whitehead C (2004) An outreach geriatric medication advisory service in residential aged care: a randomised controlled trial of case conferencing. Age Ageing 33(6):612–617
Connor S, Egan K, Kwilosz D, Larson D, Reese D (2002) Interdisciplinary approaches to assisting with end-of-life care and decision making. Am Behav Sci 46(3):340–356
Kurvers R, Wolf M, Naguib M, Krause J (2015) Self-organized flexible leadership promotes collective intelligence in human groups. R Soc Open Sci 2(12):150222
Gheewala P, Peterson G, Curtain C, Nishtala P, Hannan P, Castelino R (2014) Impact of the pharmacist medication review services on drug-related problems and potentially inappropriate prescribing of renally cleared medications in residents of aged care facilities. Drugs Aging 31(11):825–835
Davies N, Mathew R, Wilcock J, Manthorpe J, Sampson E, Lamahewa K et al (2016) A co-design process developing heuristics for practitioners providing end of life care for people with dementia. BMC palliative care 15(1):68
Reeve E, Bell S, Hilmer S (2015) Barriers to optimising prescribing and deprescribing in older adults with dementia: a narrative review. Curr Clin Pharmacol 10(3):168–177
Turner J, Edwards S, Stanners M, Shakib S, Bell S (2016) What factors are important for deprescribing in Australian long-term care facilities? Perspectives of residents and health professionals. BMJ Open 6(3):e009781
Reeve E, Low L-F, Hilmer S (2016) Beliefs and attitudes of older adults and carers about deprescribing of medications: a qualitative focus group study. Br J Gen Pract 66(649):e552–ee60
D’Agata E, Mitchell S (2008) Patterns of antimicrobial use among nursing home residents with advanced dementia. Arch Intern Med 168(4):357–362
McLachlan A, Bath S, Naganathan V, Hilmer S, Le Couteur D, Gibson S et al (2011) Clinical pharmacology of analgesic medicines in older people: impact of frailty and cognitive impairment. Br J Clin Pharmacol 71(3):351–364
Reeve E, Farrell B, Thompson W, Herrmann N, Sketris I, Magin P et al (2018) Evidence-based clinical practice guideline for deprescribing cholinesterase inhibitors and memantine in people with dementia. The University of Sydney, Sydney, Australia, Recommendations
Parsons C (2016) Withdrawal of antidementia drugs in older people: who, when and how? Drugs Aging 33(8):545–556
Narayan S, Nishtala P (2018) Population-based study examining the utilization of preventive medicines by older people in the last year of life. Geriatr Gerontol Int 18(6):892–898
Van Der Cammen T, Rajkumar C, Onder G, Sterke C, Petrovic M (2014) Drug cessation in complex older adults: time for action. Age Ageing 43(1):20–25
Page A, Clifford R, Potter K, Schwartz D, Etherton-Beer C (2016) The feasibility and effect of deprescribing in older adults on mortality and health: a systematic review and meta-analysis. Br J Clin Pharmacol 82(3):583–623
Ailabouni N, Nishtala P, Mangin D, Tordoff J (2016) Challenges and enablers of deprescribing: a general practitioner perspective. PLoS One 11(4):e0151066
Anderson K, Stowasser D, Freeman C, Scott I (2014) Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open 4(12):e006544
Nisbett R, Wilson T (1977) The halo effect: evidence for unconscious alteration of judgments. J Pers Soc Psychol 35(4):250
Acknowledgements
The authors would like to thank all participants who participated in the focus groups as part of this study.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors. DD was supported by a UTS Doctoral Scholarship.
Author information
Authors and Affiliations
Contributions
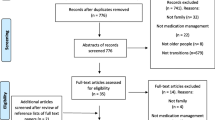
DD contributed to the development of the research questions, conducted the search, analysed the articles and drafted the manuscript. TL and MA contributed to the development of research questions and analysis of data and helped to draft the manuscript. AB and PD contributed to the analysis of data. All authors contributed to and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval was from the University of Technology Sydney (UTS) Human Research Ethics Committee (Approval Reference No. ETH16-0291). All participants gave written informed consent to participate.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Disalvo, D., Luckett, T., Bennett, A. et al. Multidisciplinary perspectives on medication-related decision-making for people with advanced dementia living in long-term care: a critical incident analysis. Eur J Clin Pharmacol 76, 567–578 (2020). https://doi.org/10.1007/s00228-019-02820-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02820-z