Abstract
Purpose
There is a large inter-individual variation in the efficacy of valproic acid (VPA) against epilepsy. The genetic polymorphism influence of sodium channels on VPA response remains a matter of debate. The aim of the study was to explore the effect of SCN1A and SCN2A gene polymorphisms on VPA response in the treatment of epilepsy among Chinese patients.
Methods
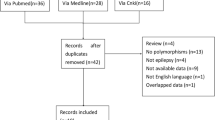
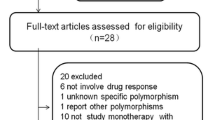
A total of 354 epileptic patients with VPA treatment were genotyped for five single nucleotide polymorphisms (SNP), including SCN1A rs10188577 T>C, rs2298771 T>C, rs3812718 G>A, and SCN2A rs2304016 A>G, rs17183814 G>A. A binary logistic regression analysis was performed to evaluate the association of genotype with VPA antiepileptic effects, adjusting the influence of confounding factors.
Results
Genotype distributions of all selected SNPs were consistent with the Hardy–Weinberg equilibrium in epilepsy patients. SCN1A rs3812718 and SCN2A rs2304016 were found to be significantly associated with VPA response, both in monotherapy and in VPA-based polytherapy. Patients with the rs3812718 A allele were more frequently seen in the VPA-responsive group (P < 0.05), and the rs2304016 G allele was related to an increased risk of resistance to VPA therapy (P < 0.05).
Conclusions
Our study revealed that SCN1A rs3812718 and SCN2A rs2304016 polymorphisms might be markers of VPA response in Chinese epilepsy patients.
Trial registration
ChiCTR-1800016477
Similar content being viewed by others
References
Moshé SL, Perucca E, Ryvlin P, Tomson T (2015) Epilepsy: new advances. Lancet 385:884–898
Verrotti A, Mazzocchetti C (2016) Epilepsy: beyond seizures-the importance of comorbidities in epilepsy. Nat Rev Neurol 12:559–560
Brodie MJ, Besag F, Ettinger AB, Mula M, Gobbi G, Comai S, Aldenkamp AP, Steinhoff BJ (2016) Epilepsy, antiepileptic drugs, and aggression: an evidence-based review. Pharmacol Rev 68:563–602
Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, Moshé SL, Perucca E, Wiebe S, French J (2010) Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia 51:1069–1077
Zhu MM, Li HL, Shi LH, Chen XP, Luo J, Zhang ZL (2017) The pharmacogenomics of valproic acid. J Hum Genet 62:1009–1014
Chateauvieux S, Morceau F, Dicato M, Diederich M (2010) Molecular and therapeutic potential and toxicity of valproic acid. J Biomed Biotechnol 2010
Marson AG, Al-Kharusi AM, Alwaidh M et al (2007) The SANAD study of effectiveness of valproate, lamotrigine, or topiramate for generalised and unclassifiable epilepsy: an unblinded randomised controlled trial. Lancet 369:1016–1026
Oyrer J, Maljevic S, Scheffer IE, Berkovic SF, Petrou S, Reid CA (2018) Ion channels in genetic epilepsy: from genes and mechanisms to disease-targeted therapies. Pharmacol Rev 70:142–173
Catterall WA, Kalume F, Oakley JC (2010) NaV1.1 channels and epilepsy. J Physiol 588:1849–1859
Szulczyk B, Nurowska E (2017) Valproic acid inhibits TTX-resistant sodium currents in prefrontal cortex pyramidal neurons. Biochem Biophys Res Commun 491:291–295
Löscher W (1999) Valproate: a reappraisal of its pharmacodynamic properties and mechanisms of action. Prog Neurobiol 58:31–59
Johannessen CU (2000) Mechanisms of action of valproate: a commentatory. Neurochem Int 37:103–110
Zuliani V, Fantini M, Rivara M (2012) Voltage-gated sodium channels as therapeutic targets in epilepsy and other neurological disorders. Curr Top Med Chem 12:962–970
Catterall WA (2014) Sodium channels, inherited epilepsy, and antiepileptic drugs. Annu Rev Pharmacol Toxicol 54:317–338
Yu FH, Mantegazza M, Westenbroek RE, Robbins CA, Kalume F, Burton KA, Spain WJ, McKnight GS, Scheuer T, Catterall WA (2006) Reduced sodium current in GABAergic interneurons in a mouse model of severe myoclonic epilepsy in infancy. Nat Neurosci 9:1142–1149
Haerian BS, Baum L, Tan HJ, Kwan P, Raymond AA, Saruwatari J, Nakagawa K, Mohamed Z (2012) SCN1AIVS5N+5 polymorphism and response to sodium valproate: a multicenter study. Pharmacogenomics 13:1477–1485
Yip TS, O'Doherty C, Tan NC, Dibbens LM, Suppiah V (2014) SCN1A variations and response to multiple antiepileptic drugs. Pharmacogenomics J 14:385–389
Li X, Zhang J, Wu X, Yan H, Zhang Y, He RH, Tang YJ, He YJ, Tan D, Mao XY, Yin JY, Liu ZQ, Zhou HH, Liu J (2016) Polymorphisms of ABAT, SCN2A and ALDH5A1 may affect valproic acid responses in the treatment of epilepsy in Chinese. Pharmacogenomics 17:2007–2014
Duan SH, Ma JL, Yang XL, Guo YF (2017) Simultaneous multigene mutation screening using SNPscan in patients from ethnic minorities with nonsyndromic hearingimpairment in Northwest China. Mol Med Rep 16:6722–6728
Ma CL, Wu XY, Jiao Z, Hong Z, Wu ZY, Zhong MK (2014) Association of SCN1A, SCN2A and ABCC2 gene polymorphisms with the response to antiepileptic drugs in Chinese Han patients with epilepsy. Pharmacogenomics 15:1323–1336
Zhou BT, Zhou QH, Yin JY, Li GL, Qu J, Xu XJ, Liu D, Zhou HH, Liu ZQ (2012) Effects of SCN1A and GABA receptor genetic polymorphisms on carbamazepine tolerability and efficacy in Chinese patients with partial seizures: 2-year longitudinal clinical follow-up. CNS Neurosci Ther 18:566–572
Zhou BT, Zhou QH, Yin JY, Li GL, Xu XJ, Qu J, Liu D, Zhou HH, Liu ZQ (2012) Comprehensive analysis of the association of SCN1A gene polymorphisms with the retention rate of carbamazepine following monotherapy for new-onset focal seizures in the Chinese Han population. Clin Exp Pharmacol Physiol 39:379–384
Manna I, Gambardella A, Bianchi A, Striano P, Tozzi R, Aguglia U, Beccaria F, Benna P, Campostrini R, Canevini MP, Condino F, Durisotti C, Elia M, Giallonardo AT, Iudice A, Labate A, la Neve A, Michelucci R, Muscas GC, Paravidino R, Zaccara G, Zucca C, Zara F, Perucca E (2011) A functional polymorphism in the SCN1A gene does not influence antiepileptic drug responsiveness in Italian patients with focal epilepsy. Epilepsia 52:e40–e44
Zhou L, Cao Y, Long H, Long L, Xu L, Liu Z, Zhang Y, Xiao B (2015) ABCB1, ABCC2, SCN1A, SCN2A, GABRA1 gene polymorphisms and drug resistant epilepsy in the Chinese Han population. Pharmazie 70:416–420
Sánchez MB, Herranz JL, Leno C, Arteaga R, Oterino A, Valdizán EM, Nicolás JM, Adín J, Armijo JA (2010) Genetic factors associated with drug-resistance of epilepsy: relevance of stratification by patient age and aetiology of epilepsy. Seizure 19:93–101
Yun W, Zhang F, Hu C, Luo X, Xue P, Wang J, Ge Y, Meng H, Guo Y (2013) Effects of EPHX1, SCN1A and CYP3A4 genetic polymorphisms on plasma carbamazepine concentrations and pharmacoresistance in Chinese patients with epilepsy. Epilepsy Res 107:231–237
Haerian BS, Baum L, Kwan P, Tan HJ, Raymond AA, Mohamed Z (2013) SCN1A, SCN2A and SCN3A gene polymorphisms and responsiveness to antiepileptic drugs: a multicenter cohort study and meta-analysis. Pharmacogenomics 14:1153–1166
Hung CC, Chang WL, Ho JL, Tai JJ, Hsieh TJ, Huang HC, Hsieh YW, Liou HH (2012) Association of polymorphisms in EPHX1, UGT2B7, ABCB1, ABCC2, SCN1A and SCN2A genes with carbamazepine therapy optimization. Pharmacogenomics 13:159–169
Tate SK, Depondt C, Sisodiya SM, Cavalleri GL, Schorge S, Soranzo N, Thom M, Sen A, Shorvon SD, Sander JW, Wood NW, Goldstein DB (2005) Genetic predictors of the maximum doses patients receive during clinical use of the anti-epileptic drugs carbamazepine and phenytoin. Proc Natl Acad Sci U S A 102:5507–5512
Tate SK, Singh R, Hung CC, Tai JJ, Depondt C, Cavalleri GL, Sisodiya SM, Goldstein DB, Liou HH (2006) A common polymorphism in the SCN1A gene associates with phenytoin serum levels at maintenance dose. Pharmacogenet Genomics 16:721–726
Eliasson E, Lindh JD, Malmström RE, Beck O, Dahl ML (2013) Therapeutic drug monitoring for tomorrow. Eur J Clin Pharmacol 69(Suppl 1):25–32
Copley RR (2004) Evolutionary convergence of alternative splicing in ion channels. Trends Genet 20:171–176
Heinzen EL, Yoon W, Tate SK, Sen A, Wood NW, Sisodiya SM, Goldstein DB (2007) Nova2 interacts with a cis-acting polymorphism to influence the proportions of drug-responsive splice variants of SCN1A. Am J Hum Genet 80:876–883
Fletcher EV, Kullmann DM, Schorge S (2011) Alternative splicing modulates inactivation of type 1 voltage-gated sodium channels by toggling an amino acid in the first S3-S4 linker. J Biol Chem 286:36700–36708
Anderson LL, Hawkins NA, Thompson CH, Kearney JA, George AL Jr (2017) Unexpected efficacy of a novel sodium channel modulator in Dravet syndrome. Sci Rep 7:1682
Brunklaus A, Ellis R, Reavey E, Forbes GH, Zuberi SM (2012) Prognostic, clinical and demographic features in SCN1A mutation-positive Dravet syndrome. Brain 135:2329–2336
Younus I, Reddy DS (2017) Epigenetic interventions for epileptogenesis: a new frontier for curing epilepsy. Pharmacol Ther 177:108–122
Kumari R, Lakhan R, Kumar S, Garg RK, Misra UK, Kalita J, Mittal B (2013) SCN1AIVS5-91G>A polymorphism is associated with susceptibility to epilepsy but not with drug responsiveness. Biochimie 95:1350–1353
Tang L, Lu X, Tao Y, Zheng J, Zhao P, Li K, Li L (2014) SCN1A rs3812718 polymorphism and susceptibility to epilepsy with febrile seizures: a meta-analysis. Gene 533:26–31
Kwan P, Poon WS, Ng HK, Kang DE, Wong V, Ng PW, Lui CH, Sin NC, Wong KS, Baum L (2008) Multidrug resistance in epilepsy and polymorphisms in the voltage-gated sodium channel genes SCN1A, SCN2A, and SCN3A: correlation among phenotype, genotype, and mRNA expression. Pharmacogenet Genomics 18:989–998
Acknowledgments
We thank all patients and their family members who contributed to this work. We thank Professor Shusen Sun from College of Pharmacy and Health Sciences at Western New England University, USA, for his valuable advice.
Contributions of authors
Zanling Zhang designed the study. Lihong Shi performed the data analysis and wrote the manuscript. Miaomiao Zhu, Huilan Li, and Zhipeng Wen recruited patients and conducted patients’ follow-up. Jia Luo and Cong Lin extracted the DNA. Xiaoping Chen reviewed the manuscript and critically revised the intellectual content of the manuscript.
Funding
This work was supported by a grant from the Natural Science Foundation of Hunan Province (no. 2017JJ2398).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
All procedures performed in studies involving human participants were in accordance with the ethical standards of Xiangya Hospital Central South University Medical Ethics Committee, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 19 kb)
Rights and permissions
About this article
Cite this article
Shi, L., Zhu, M., Li, H. et al. SCN1A and SCN2A polymorphisms are associated with response to valproic acid in Chinese epilepsy patients. Eur J Clin Pharmacol 75, 655–663 (2019). https://doi.org/10.1007/s00228-019-02633-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-019-02633-0