Abstract
Purpose
We used a retrospective data mining approach to explore the association between serum amiodarone (AMD) and N-desethylamiodarone (DEA) concentrations and thyroid-related hormone levels.
Methods
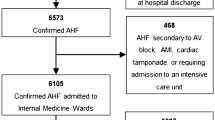
Laboratory data sets from January 2012 to April 2016 were extracted from the computerized hospital information system database at the National Cerebral and Cardiovascular Center (NCVC). Data sets that contained serum AMD and DEA concentrations and thyroid function tests, including thyroid-stimulating hormone (TSH), free thyroxine (FT4), and free triiodothyronine (FT3), were analyzed.
Results
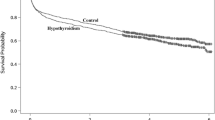
A total of 1831 clinical laboratory data sets from 330 patients were analyzed. Data sets were classified into five groups (euthyroidism, hyperthyroidism, subclinical hyperthyroidism, hypothyroidism, and subclinical hypothyroidism) based on the definition of thyroid function in our hospital. Most abnormal levels of thyroid hormones were observed within the therapeutic range of serum AMD and DEA concentrations. The mean DEA/AMD ratio in the hyperthyroidism group was significantly higher than that in the euthyroidism group (0.95 ± 0.42 vs. 0.87 ± 0.28, p = 0.0209), and the mean DEA/AMD ratio in the hypothyroidism group was significantly lower than that in the euthyroidism group (0.77 ± 0.26 vs. 0.87 ± 0.28, p = 0.0038). The suppressed TSH group (0.98 ± 0.41 vs. 0.87 ± 0.28, p < 0.001) and the elevated FT4 level group (0.90 ± 0.33 vs. 0.84 ± 0.27, p = 0.0037) showed significantly higher DEA/AMD ratios compared with normal level groups. The elevated TSH group showed a significantly lower DEA/AMD ratio compared with the normal group (0.81 ± 0.25 vs. 0.87 ± 0.28, p < 0.0001).
Conclusions
High and low DEA/AMD ratios were associated with AMD-induced hyperthyroidism and hypothyroidism, respectively. The DEA/AMD ratio may be a predictive marker for AMD-induced thyroid dysfunction.



Similar content being viewed by others
References
Vorperian VR, Havighurst TC, Miller S, January CT (1997) Adverse effects of low dose amiodarone: a meta-analysis. J Am Coll Cardiol 30(3):791–798
Martino E, Bartalena L, Bogazzi F, Braverman LE (2001) The effects of amiodarone on the thyroid. Endocr Rev 22(2):240–254. doi:10.1210/edrv.22.2.0427
Sidhu J, Jenkins D (2003) Men are at increased risk of amiodarone-associated thyrotoxicosis in the UK. QJM : monthly journal of the Association of Physicians 96(12):949–950
Schaan BD, Cunha CP, Francisconi A, Zottis B, Brum G, Bruch RS, Gus M (2005) Amiodarone-induced thyroid dysfunction in a tertiary center in South Brazil. Arquivos brasileiros de endocrinologia e metabologia 49(6):916–922. doi:10.1590/S0004-27302005000600010
Lee KF, Lee KM, Fung TT (2010) Amiodarone-induced thyroid dysfunction in the Hong Kong Chinese population. Hong Kong medical journal = Xianggang yi xue za zhi / Hong Kong Academy of Medicine 16(6):434–439
Ahmed S, Van Gelder IC, Wiesfeld AC, Van Veldhuisen DJ, Links TP (2011) Determinants and outcome of amiodarone-associated thyroid dysfunction. Clin Endocrinol 75(3):388–394. doi:10.1111/j.1365-2265.2011.04087.x
Stan MN, Ammash NM, Warnes CA, Brennan MD, Thapa P, Nannenga MR, Bahn RS (2013) Body mass index and the development of amiodarone-induced thyrotoxicosis in adults with congenital heart disease—a cohort study. Int J Cardiol 167(3):821–826. doi:10.1016/j.ijcard.2012.02.015
Zosin I, Balas M (2012) Amiodarone-induced thyroid dysfunction in an iodine-replete area: epidemiological and clinical data. Endokrynologia Polska 63(1):2–9
Martino E, Aghini-Lombardi F, Mariotti S, Bartalena L, Lenziardi M, Ceccarelli C, Bambini G, Safran M, Braverman LE, Pinchera A (1987) Amiodarone iodine-induced hypothyroidism: risk factors and follow-up in 28 cases. Clin Endocrinol 26(2):227–237
Trip MD, Wiersinga W, Plomp TA (1991) Incidence, predictability, and pathogenesis of amiodarone-induced thyrotoxicosis and hypothyroidism. Am J Med 91(5):507–511
Aleksic Z, Aleksic A (2011) Incidence of amiodarone-induced thyroid dysfunction and predictive factors for their occurrence. Med Pregl 64(11–12):533–538
Martino E, Aghini-Lombardi F, Bartalena L, Grasso L, Loviselli A, Velluzzi F, Pinchera A, Braverman LE (1994) Enhanced susceptibility to amiodarone-induced hypothyroidism in patients with thyroid autoimmune disease. Arch Intern Med 154(23):2722–2726
Martino E, Safran M, Aghini-Lombardi F, Rajatanavin R, Lenziardi M, Fay M, Pacchiarotti A, Aronin N, Macchia E, Haffajee C et al (1984) Environmental iodine intake and thyroid dysfunction during chronic amiodarone therapy. Ann Intern Med 101(1):28–34
Martino E, Aghini-Lombardi F, Mariotti S, Bartalena L, Braverman L, Pinchera A (1987) Amiodarone: a common source of iodine-induced thyrotoxicosis. Horm Res 26(1–4):158–171
Zava TT, Zava DT (2011) Assessment of Japanese iodine intake based on seaweed consumption in Japan: a literature-based analysis. Thyroid Res 4:14. doi:10.1186/1756-6614-4-14
Fabre G, Julian B, Saint-Aubert B, Joyeux H, Berger Y (1993) Evidence for CYP3A-mediated N-deethylation of amiodarone in human liver microsomal fractions. Drug metabolism and disposition: the biological fate of chemicals 21(6):978–985
Pollak PT, Bouillon T, Shafer SL (2000) Population pharmacokinetics of long-term oral amiodarone therapy. Clin Pharmacol Ther 67(6):642–652. doi:10.1067/mcp.2000.107047
Bolt MW, Racz WJ, Brien JF, Massey TE (2001) Effects of vitamin E on cytotoxicity of amiodarone and N-desethylamiodarone in isolated hamster lung cells. Toxicology 166(3):109–118
Pollak PT (1999) Clinical organ toxicity of antiarrhythmic compounds: ocular and pulmonary manifestations. Am J Cardiol 84(9A):37R–45R
Brien JF, Jimmo S, Brennan FJ, Ford SE, Armstrong PW (1987) Distribution of amiodarone and its metabolite, desethylamiodarone, in human tissues. Can J Physiol Pharmacol 65(3):360–364
Kashima A, Funahashi M, Fukumoto K, Komamura K, Kamakura S, Kitakaze M, Ueno K (2005) Pharmacokinetic characteristics of amiodarone in long-term oral therapy in Japanese population. Biol Pharm Bull 28(10):1934–1938
Lafuente-Lafuente C, Alvarez JC, Leenhardt A, Mouly S, Extramiana F, Caulin C, Funck-Brentano C, Bergmann JF (2009) Amiodarone concentrations in plasma and fat tissue during chronic treatment and related toxicity. Br J Clin Pharmacol 67(5):511–519. doi:10.1111/j.1365-2125.2009.03381.x
Lee S, Farwell AP (2016) Euthyroid sick syndrome. Comprehensive Physiology 6(2):1071–1080. doi:10.1002/cphy.c150017
Hayashi T, Hasegawa T, Kanzaki H, Funada A, Amaki M, Takahama H, Ohara T, Sugano Y, Yasuda S, Ogawa H, Anzai T (2016) Subclinical hypothyroidism is an independent predictor of adverse cardiovascular outcomes in patients with acute decompensated heart failure. ESC heart failure 3(3):168–176. doi:10.1002/ehf2.12084
Pingitore A, Landi P, Taddei MC, Ripoli A, L'Abbate A, Iervasi G (2005) Triiodothyronine levels for risk stratification of patients with chronic heart failure. Am J Med 118(2):132–136. doi:10.1016/j.amjmed.2004.07.052
Frey A, Kroiss M, Berliner D, Seifert M, Allolio B, Guder G, Ertl G, Angermann CE, Stork S, Fassnacht M (2013) Prognostic impact of subclinical thyroid dysfunction in heart failure. Int J Cardiol 168(1):300–305. doi:10.1016/j.ijcard.2012.09.064
Lo JC, Chertow GM, Go AS, Hsu CY (2005) Increased prevalence of subclinical and clinical hypothyroidism in persons with chronic kidney disease. Kidney Int 67(3):1047–1052. doi:10.1111/j.1523-1755.2005.00169.x
Waldhauser KM, Torok M, Ha HR, Thomet U, Konrad D, Brecht K, Follath F, Krahenbuhl S (2006) Hepatocellular toxicity and pharmacological effect of amiodarone and amiodarone derivatives. J Pharmacol Exp Ther 319(3):1413–1423. doi:10.1124/jpet.106.108993
Kaufmann P, Torok M, Hanni A, Roberts P, Gasser R, Krahenbuhl S (2005) Mechanisms of benzarone and benzbromarone-induced hepatic toxicity. Hepatology (Baltimore, Md) 41(4):925–935. doi:10.1002/hep.20634
Bolt MW, Card JW, Racz WJ, Brien JF, Massey TE (2001) Disruption of mitochondrial function and cellular ATP levels by amiodarone and N-desethylamiodarone in initiation of amiodarone-induced pulmonary cytotoxicity. J Pharmacol Exp Ther 298(3):1280–1289
Chiovato L, Martino E, Tonacchera M, Santini F, Lapi P, Mammoli C, Braverman LE, Pinchera A (1994) Studies on the in vitro cytotoxic effect of amiodarone. Endocrinology 134(5):2277–2282. doi:10.1210/endo.134.5.8156930
Beddows SA, Page SR, Taylor AH, McNerney R, Whitley GS, Johnstone AP, Nussey SS (1989) Cytotoxic effects of amiodarone and desethylamiodarone on human thyrocytes. Biochem Pharmacol 38(24):4397–4403
Holt DW, Tucker GT, Jackson PR, Storey GC (1983) Amiodarone pharmacokinetics. Am Heart J 106(4 Pt 2):840–847
Hanioka N, Matsumoto K, Saito Y, Narimatsu S (2011) Influence of CYP2C8*13 and CYP2C8*14 alleles on amiodarone N-deethylation. Basic & clinical pharmacology & toxicology 108(5):359–362. doi:10.1111/j.1742-7843.2010.00669.x
Sato K, Miyakawa M, Eto M, Inaba T, Matsuda N, Shiga T, Ohnishi S, Kasanuki H (1999) Clinical characteristics of amiodarone-induced thyrotoxicosis and hypothyroidism in Japan. Endocr J 46(3):443–451
Thienpont LM, Van Uytfanghe K, Van Houcke S, Das B, Faix JD, MacKenzie F, Quinn FA, Rottmann M, Van den Bruel A (2014) A progress report of the IFCC Committee for Standardization of Thyroid Function Tests. European thyroid journal 3(2):109–116. doi:10.1159/000358270
Acknowledgements
None.
Authors’ contributions
Mitsutaka Takada conceived the study and design. Mikie Yamato, Kyoichi Wada, and Akira Oita acquired data. Mikie Yamato, Kyoichi Wada, and Mitsutaka Takada analyzed and interpreted data. Mikie Yamato, Kyoichi Wada, and Mitsutaka Takada drafted the manuscript. Mai Fujimoto, Kouichi Hosomi, and Tomohiro Hayashi revised the manuscript. Mikie Yamato and Mistukata Takada analyzed statistical data. Mistutaka Takada did supervision.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This study was approved by the Ethics Committees of the NCVC and Kindai University. For this type of study, formal consent is not required.
Additional information
This study was carried out in the Department of Pharmacy, National Cerebral and Cardiovascular Center, 5-7-1 Fujishiro-dai, Suita, Osaka, Japan.
Electronic supplementary material
ESM 1
(DOCX 221 kb).
Rights and permissions
About this article
Cite this article
Yamato, M., Wada, K., Fujimoto, M. et al. Association between N-desethylamiodarone/amiodarone ratio and amiodarone-induced thyroid dysfunction. Eur J Clin Pharmacol 73, 289–296 (2017). https://doi.org/10.1007/s00228-017-2195-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-017-2195-5