Abstract
Purpose
Effective and efficient medication reporting processes are essential in promoting patient safety. Few qualitative studies have explored reporting of medication errors by health professionals, and none have made reference to behavioural theories. The objective was to describe and understand the behavioural determinants of health professional reporting of medication errors in the United Arab Emirates (UAE).
Methods
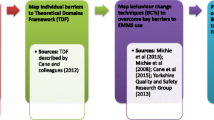
This was a qualitative study comprising face-to-face, semi-structured interviews within three major medical/surgical hospitals of Abu Dhabi, the UAE. Health professionals were sampled purposively in strata of profession and years of experience. The semi-structured interview schedule focused on behavioural determinants around medication error reporting, facilitators, barriers and experiences. The Theoretical Domains Framework (TDF; a framework of theories of behaviour change) was used as a coding framework. Ethical approval was obtained from a UK university and all participating hospital ethics committees.
Results
Data saturation was achieved after interviewing ten nurses, ten pharmacists and nine physicians. Whilst it appeared that patient safety and organisational improvement goals and intentions were behavioural determinants which facilitated reporting, there were key determinants which deterred reporting. These included the beliefs of the consequences of reporting (lack of any feedback following reporting and impacting professional reputation, relationships and career progression), emotions (fear and worry) and issues related to the environmental context (time taken to report).
Conclusion
These key behavioural determinants which negatively impact error reporting can facilitate the development of an intervention, centring on organisational safety and reporting culture, to enhance reporting effectiveness and efficiency.
Similar content being viewed by others
References
National Coordinating Council for Medication Error Reporting and Prevention. 2016 Available at http://www.nccmerp.org [accessed January 2016].
Keers RN, Williams SD, Cooke J, Ashcroft DM (2013) Prevalence and nature of medication administration errors in health care settings: a systematic review of direct observational evidence. Ann Pharmacother 47(2):237–256
Keers RN, Williams SD, Cooke J, Ashcroft DM (2013) Causes of medication administration errors in hospitals: a systematic review of quantitative and qualitative evidence. Drug Saf 36(11):1045–1067
Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM (2009) Prevalence, incidence and nature of prescribing errors in hospital inpatients: a systematic review. Drug Saf 32(5):379–389
Ross S, Bond C, Rothnie H, Thomas S, Macleod MJ (2009) What is the scale of prescribing errors committed by junior doctors? A systematic review. Brit J Clin Pharm 67(6):629–640
Wakefield DS, Wakefield BJ, Uden-Holman BMA (1996) Perceived barriers in reporting medication administration errors. Best Pract and Benchmarking Healthc 1:191–197
Uribe CL, Schweikhart SB, Pathak DS, Marsh GB, Fraley RR (2002) Perceived barriers to medical error reporting: an exploratory investigation. J Healthc Manag 47:263–279
McArdle D, Burns N, Ireland A (2003) Attitudes and beliefs of doctors towards medication error reporting. Int J Health Care Qual Assur 16:326–333
Stratton KM, Nlegen MA, Peppper G, Vaughn T (2004) Reporting of medication errors by pediatric nurses. J Pediatr Nurs 19:385–392
Evans SM, Berry JG, Smith BJ, Esterman A, Selim P, O’Shaughnessy J, et al. (2006) Attitudes and barriers to incident reporting: a collaborative hospital study. Qual Saf Health Care 15:39–43
Sanghera IS, Franklin BD, Dhillon S (2007) The attitudes and beliefs of healthcare professionals on the causes and reporting of medication errors in a UK intensive care unit. Anaesthesia 62:53–61
Armitage G, Newell R, Wright J (2010) Improving the quality of drug error reporting. J Eval Clin Pract 16:1189–1197
Sarvadikar A, Prescott G, Williams D (2010) Attitudes to reporting medication error among differing healthcare professionals. Eur J Clin Pharmacol 66:843–853
Castel ES, Ginsburg LR, Zaheer S (2015) Understanding nurses’ and physicians’ fear of repercussions for reporting errors: clinician characteristics, organization demographics, or leadership factors? BMC Health Serv Res 15:326
Kingston MJ, Evans SM, Smith BJ, Berry J (2004) Attitudes of doctors and nurses towards incident reporting: a qualitative analysis. Med J Aus 181:36–39
Hartnell N, MacKinnon N, Sketeris I, Fleming M (2012) Identifying, understanding and overcoming barriers to medication error reporting in hospitals: a focus group study. BMJ Qual Saf 21:361–368
Williams SD, Phipps DL, Ashcroft DM (2013) Understanding the attitudes of hospital pharmacists to reporting medication incidents: a qualitative study. Res Soc Adm Pharm 9:80–89
Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M (2008) Developing and evaluating complex interventions: the new Medical Research Council guidance. Brit Med J 337:a1665
Davies P, Walker AE, Grimshaw JM (2010) A systematic review of the use of theory in the design of guideline dissemination and implementation strategies and interpretation of the results of rigorous evaluation. Implement Sci 5:14
Cane J, O’Connor D, Michie S (2012) Validation of the Theoretical Domains Framework for use in behaviour change and implementation research. Implement Sci 7:37
Francis JJ, O’Connor D, Curran J (2012) Theories of behaviour change synthesised into a set of theoretical groupings: introducing a thematic series on the Theoretical Domains Framework. Implement Sci 7:35
Health Authority Abu Dhabi Medication Error Reporting Policy version 1, 2009. Available at http://www.haad.ae/haad/tabid/58/Mid/417/ItemID/225/ctl/Details/Default.aspx [Accessed January 2016]
Francis JJ, Johnston M, Robertson C, Glidewell L, Entwistle V, Eccles MP, et al. (2010) What is an adequate sample size? Operationalising data saturation for theory-based interview studies. Psychol Health 25(10):1229–1245
Ritchie J, Spencer L (2002) Qualitative data analysis for applied policy research. Qual Res Companion 305-329
Shenton AK (2004) Strategies for ensuring trustworthiness in qualitative research projects. Educ Inf 22:63–67
Halligan M, Zecevic A (2011) Safety culture in healthcare: a review of concepts, dimensions, measures and progress. BMJ Qual Saf 20(4):338–343
Morello RT, Lowthian JA, Barker AL, McGinnes R, Dunt D, Brand C (2013) Strategies for improving patient safety culture in hospitals: a systematic review. BMJ Qual Saf 22:11–18
Weaver SJ, Lubomksi LH, Wilson RF, Pfoh ER, Martinez KA, Dy SM (2013) Promoting a culture of safety as a patient safety strategy: a systematic review. Ann Intern Med 158:369–374
Michie S, van Stralen MM, West R (2011) The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci 6:42
May CR, Mair F, Finch T, MacFarlane A, Dowrick C, Treweek S, et al. (2009) Development of a theory of implementation and integration: normalization process theory. Implement Sci 4:29
May C, Finch T (2009) Implementing, embedding and integrating practices: an outline of normalization process theory. Sociology 43:535–554
Acknowledgments
The authors would like to acknowledge the following for their contribution and support provided throughout this research: Embassy of the United Arab Emirates for funding Mai Alqubaisi; Katie MacLure, Gordon Rushworth, Cristin Ryan, and Anne Watson for reviewing the draught interview schedule; the ethical review panels and Human Resources Departments of all participating hospitals; and all interviewees.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Mai Alqubaisi, Antonella Tonna, Alison Strath, and Derek Stewart declare that they have no conflict of interest.
Funding
Funding for Mai Alqubaisi’s doctoral studies was provided by the Embassy of the United Arab Emirates.
Rights and permissions
About this article
Cite this article
Alqubaisi, M., Tonna, A., Strath, A. et al. Exploring behavioural determinants relating to health professional reporting of medication errors: a qualitative study using the Theoretical Domains Framework. Eur J Clin Pharmacol 72, 887–895 (2016). https://doi.org/10.1007/s00228-016-2054-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-016-2054-9