Abstract
Rationale
Caffeine is the most consumed stimulant worldwide, and there is great interest in understanding its neurophysiological effects. Resting-state electroencephalography (EEG) studies suggest that caffeine enhances arousal, which suppresses the spectral power of alpha frequencies associated with reduced alertness. However, it is unclear whether caffeine’s neurophysiological effects vary across the human menstrual cycle.
Objective
The objective of our study was to test whether caffeine’s effect on EEG activity differs across the human menstrual cycle.
Methods
Fifty-six female participants were randomly assigned to complete the experiment while in either their menstrual (n = 21), follicular (n = 19), or luteal (n = 16) phase. Each participant completed two study sessions in the same menstrual phase, approximately 1 month apart, during which they were administered either a caffeine pill (200 mg, oral) or a placebo pill in a counterbalanced order using a randomized double-blinded procedure. We measured their eyes-closed resting-state EEG approximately 30 min after pill administration and conducted a spectral power analysis at different frequency bands.
Results
Caffeine reduced EEG power in the alpha1 frequency band (8–10 Hz), but only for participants who self-reported higher weekly caffeine consumption. Importantly, caffeine’s effects did not differ by menstrual phase.
Conclusions
We conclude that when studying caffeine’s effects on resting-state EEG, participants’ baseline caffeine consumption is more influential than their menstrual cycle phase. This study has important implications for the inclusion of menstruating individuals in neurophysiological studies of caffeine.
Similar content being viewed by others
Introduction
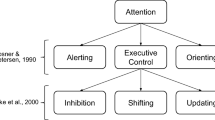
Caffeine (1,3,7-trimethylxanthine) is the most widely used stimulant worldwide; thus, understanding its effects on neural activity has widespread implications for human behavior and performance. Caffeine is a stimulant that increases arousal and sustained attention, in addition to causing systemic physiological effects such as increasing blood pressure (Cooper et al. 2020; Renda and De Caterina 2019). One common measure of arousal is resting-state electroencephalography (EEG), whereby spontaneous brain activity is measured in absence of any task-related effects (Newson and Thiagarajan 2019). Resting-state EEG can be divided into various frequency bands, including delta (1–4 Hz), theta (4–8 Hz), alpha (8–12 Hz), and beta (12–20 Hz). Alpha activity (8–12 Hz) is associated with a state of reduced arousal between fully alert and light sleep. Barry et al. (2005b) showed that a single oral dose of caffeine (250 mg; approximately equivalent to one large cup of coffee) reduced global alpha power, providing electrophysiological evidence of caffeine’s arousal-enhancing effects.
There is considerable interindividual variability in response to caffeine (Renda and De Caterina 2019). Caffeine’s effects can vary by demographic variables and interactions with other systemic processes, such as the human menstrual cycle (Teichmann 1990). The human menstrual cycle has historically been divided into two phases: the follicular phase, characterized by increasing estrogen release as a single follicle develops toward ovulation, and the luteal phase, characterized by increase in progesterone release from the corpus luteum post-ovulation (Owen 1975). The menses (menstrual phase), considered as occurring in the early stages of the follicular phase, is characterized by decreased estrogen and progesterone levels as the uterus sheds its lining through menstruation (Richards 2018). Caffeine studies sometimes exclude menstruating individuals to avoid these hormonal effects (e.g., Huertas et al. 2019), limiting the generalizability of caffeine’s effects for female populations.
To our knowledge, no study to date has examined whether the electrophysiological effects of caffeine vary across the menstrual cycle. However, Bazanova et al. (2017) examined menstrual phase differences in the Berger effect, which is the well-documented suppression of alpha activity when the eyes are opened versus closed (Barry et al. 2007). Bazanova et al. (2017) found that alpha suppression from the Berger effect was greatest in the follicular phase, but only for lower alpha frequencies (i.e., alpha1, 8–10 Hz), which were more dominant in the follicular phase when compared to the luteal and menstrual phases. When alpha activity is separated into sub-bands, the state of reduced arousal is more specific to alpha1 activity (8–10 Hz), whereas alpha2 activity (10–12 Hz) has been associated with a state of increased arousal (Fisher et al. 2012; Knott 2001; Knott et al. 1998). Interestingly, there is some evidence that caffeine produces greater reductions in alpha activity for lower alpha frequencies (Barry et al. 2005b). Taken together, these findings suggest that the effects of caffeine may vary by baseline arousal state, which appears to fluctuate across the menstrual cycle.
The objective of the present study was to systematically investigate the impact of caffeine on resting-state EEG activity across the human menstrual cycle. We hypothesized that caffeine would reduce global alpha power (Barry et al. 2011, 2005b). Furthermore, we expected this caffeine effect to be largest in the follicular phase, which has been associated with lower alpha frequencies that are typically more impacted by caffeine (Baker and Colrain, 2010; Barry et al. 2005b; Bazanova et al. 2017).
Method
Participants
Eighty healthy adult female participants were recruited from the general community in Halifax, Nova Scotia, Canada. Participants were randomly assigned to participate during either their menstrual (2–4 days after onset of the menstrual cycle; n = 26), follicular (15–22 days before onset of the next menstrual cycle; n = 27), or luteal (3–9 days before onset of the next menstrual cycle; n = 27) phase. Phases were defined relative to the expected onset of their next menses to account for interindividual cycle length variation, which primarily occurs in the follicular phase (Lein 1979; Walpurger et al. 2004). Two hormonal assays (measuring salivary progesterone P4 and 17β-estradiol) were also conducted as a secondary verification of menstrual cycle phase. All participants from the follicular and luteal phase groups were naturally cycling, whereas participants in the menstrual phase group were either naturally cycling (n = 11) or using hormonal birth control (n = 15). The overall sample had a mean age of 25.09 years (SD = 6.28) and a mean education of 16.42 years (SD = 2.55), neither of which significantly differed between the three phase groups (ps ≥ 0.12).
To be included in the study, participants needed to be aged 18 to 40 years; be right-handed, as measured by the Edinburgh Handedness Inventory (EHI; Oldfield 1971); have regularly occurring menstruation; and have normal or corrected-to-normal vision. Participants were excluded if they self-reported: a DSM-5 psychiatric illness, current history of drug abuse or dependence, head injury resulting in the loss of consciousness within the last year, a neurological disorder (e.g., multiple sclerosis, epilepsy), regular use of prescription medications (except for oral contraceptive pill for a subset of participants in the menstrual group) within 2 weeks of study participation, significant cardiac illness, or pregnancy within the past year. Additionally, any participants currently breastfeeding were excluded because breastfeeding is known to alter circulating hormone levels (Diaz et al. 1995). All study procedures were consistent with the Declaration of Helsinki and cleared by the Mount Saint Vincent University Research Ethics Board prior to study onset.
Experimental design
The present study employed a mixed experimental design. Phase was treated as a between-subject factor with three levels (menstrual, follicular, and luteal), and caffeine was treated as a within-subject factor with two levels (caffeine or placebo). Each participant attended two study sessions that were one full cycle apart (approximately 28 days; exact timing determined based on their individual cycle length) so that they were assessed during the same menstrual phase. Each participant took a caffeine pill (200 mg) in one session and a placebo pill in the other session. Caffeine or placebo administration was randomized, double-blinded, and order was counterbalanced across participants. The primary measure was eyes-closed resting-state EEG power across different frequency bands (delta, theta, alpha, alpha1, alpha2, and beta; see “Electroencephalography” section below for more details).
Materials
Demographic questionnaire. Participants completed an author-generated questionnaire to confirm that they met inclusion criteria and record demographic variables (i.e., age and years of education).
Caffeine Consumption Questionnaire. Because frequency of typical caffeine use can moderate the cognitive effects of caffeine (e.g., Huertas et al. 2019), we measured participants’ caffeine use using the Caffeine Consumption Questionnaire (CCQ; Shohet and Landrum 2001). The CCQ is a standardized self-report measure of caffeine use that asks participants to report on their typical weekly consumption of a range of common caffeine sources (e.g., coffee, chocolate, soft drinks) at different times of day (morning, afternoon, evening, and night). The total score represents the participant’s typical number of milligrams of caffeine consumed per week.
Caffeine administration. Caffeine or placebo was administered orally in pill form (with water), which facilitated dosing and double-blinding procedures. We ensured that there was a 30-min delay between drug administration and onset of study tasks, as absorption of orally administered caffeine typically peaks 15–45 min after ingestion (Renda and De Caterina 2019). We selected a moderate dose of 200 mg that approximates the amount of caffeine in a medium, black, drip coffee (Foster 2020). Furthermore, this dose has demonstrated robust effects on neural activity in past cognitive studies (e.g., Chen and Parrish 2009; Murd et al. 2010).
Procedure
Study procedures took place at Mount Saint Vincent University (Halifax, NS, Canada). Participants attended an initial session to complete informed consent, fill out study questionnaires, receive their randomized group assignment, and schedule their two experimental sessions, both of which took place at 9AM to control for time-of-day effects (Hines 2004). All participants were asked to abstain from caffeine or other drugs (i.e., alcohol, cigarettes, cannabis, street drugs, and over-the-counter medications) starting at midnight the day prior (i.e., 9 h prior) to each experimental session. Upon arrival at the lab, participants provided verbal confirmation of this abstinence. Saliva was then collected in two 1.7-mL microcentrifuge tubes (VWR® #87,003–294, Mississauga, ON, Canada) using the passive drool collection method. Briefly, participants were instructed to pool saliva in their mouths and then use a straw to drool into each tube. Samples were placed in a − 30 °C freezer for later analysis of salivary hormones. Next, participants were administered their caffeine or placebo pill with water and fitted with their EEG cap and electrodes. Approximately 30 min after pill ingestion, eyes-closed resting-state EEG data were recorded, as well as data from a battery of cognitive tasks (not analyzed in the present study). At the end of their second experimental session, participants were debriefed about the study and provided with their compensation.
Electroencephalography
Continuous EEG data were collected during a 3-min eyes-closed period from 32 Ag+/Ag+-Cl− active scalp electrodes arranged according to the 10–10 system. Two additional electrodes were applied to the mid-forehead and nose to serve as the ground and online references, respectively. In addition, bipolar recordings of horizontal (HEOG) and vertical (VEOG) electro-oculogram activity were taken from supra-/sub-orbital and external canthi sites, respectively. Electrical impedances were kept under 5 kΩ. Data were sampled online at 500 Hz and re-referenced offline to the linked mastoids (TP9 and TP10). Pre-processing was conducted using BrainVision Analyzer 2.0 (Brain Products GmbH, Gilching, Germany). Data were passed through a 0.1–30-Hz Butterworth filter with a 60-Hz notch. Data were segmented into 2-s epochs with 50% overlap. An automated artifact rejection procedure was used that rejected epochs with a voltage step greater than 50 µV/ms, or an absolute difference in voltage (max–min) greater than 100 µV or less than 0.5 µV within any 200-ms interval. Next, a fast-Fourier transformation (FFT) was applied with a 10% Hanning window and periodic variance correction. Data were averaged across epochs for each participant, and participant-level power values were exported in the following frequency bands: delta (1–4 Hz), theta (4–8 Hz), alpha (8–12 Hz), alpha1 (8–10 Hz), alpha2 (10–12 Hz), and beta (12–20 Hz).
Biochemical analysis
Salivary estradiol and progesterone levels were determined by Enzyme Immunoassay (EIA) following manufacturer protocols using the Salivary 17β-Estradiol EIA Kit (#1–3702; sensitivity 0.1 pg/mL) and the Salivary Progesterone (P4) EIA Kit (#1–1502; sensitivity 5 pg/mL) from Salimetrics® (Salimetrics, Carlsbad, CA, USA). For analysis, saliva samples were thawed at room temperature and then centrifuged at 1500 × g for 15 min at room temperature. Samples were analyzed in duplicate, and any duplicates with a coefficient of variation (CV) above 20% between wells were re-run on a subsequent plate. If the CV was again above 20% between wells, the data were excluded from analysis. Furthermore, if a sample value was unexpected based on the expected hormone concentrations (e.g., Bazanova et al. 2017; Brötzner et al. 2014) from that specific phase, the sample was re-run and the concentration that was used in analyses was that from the plate with the lowest CV between duplicates.
For the estradiol assays specifically, any samples that read below the assay’s level of detection were included in analyses but inputted as the lowest average standard concentration detected in the assay (i.e., the standard 6 concentration; 1.017–1.111 pg/mL depending on the specific assay). This decision was made in order to prevent skewing the data via inputting 0 pg/mL or reducing sample sizes via removal of participants. Since there was no effect of study session order for estradiol or progesterone levels (ps ≥ 0.5), sample values were averaged across the two sessions for each participant. As reported by the manufacturer, interassay precision for the estradiol kit was 6.0% and 8.9% for high- and low-level samples, and interassay precision for the progesterone kit was 5.5% and 9.6% for high- and low-level samples, respectively. Intra-assay precision for the estradiol kit was 7.0%, 6.3%, and 8.1% for high-, mid-, and low-level samples, respectively, and for the progesterone kit intra-assay precision was 4.0% and 8.4% for high- and low-level samples, respectively.
Statistical analyses
Data were analyzed using IBM SPSS Statistics (v. 26) and graphed using R Studio (v. 3.6.3). First, all data underwent a natural logarithmic transformation to adjust for positive skewness. For each frequency band, data from specific electrodes were averaged to create four regions of interest (ROIs): left frontal (F3 and F7), right frontal (F4 and F8), left parietal (P3 and P7), and right parietal (P4 and P8). Prior to averaging, data from these electrodes were screened for outliers, which were defined as greater than 1.5 times the interquartile range (IQR). Each outlier was replaced by the value for the other electrode in that ROI (e.g., an outlier at F3 would be replaced by the value at F7 for that participant). If both values in a ROI were outliers, they were both treated as missing values.
To test our hypotheses, a series of 3 × 2 × 2 × 2 mixed ANOVAs were conducted for each frequency band with the following factors: phase (menstrual, follicular, luteal), drug (caffeine, placebo), region (frontal, parietal), and hemisphere (left, right). These models were also run with CCQ score included as a covariate. For analyses of hormonal assay results, salivary concentrations of estradiol and progesterone were compared across three menstrual phases (i.e., menstrual, follicular, luteal). For all analyses, p < 0.05 was considered statistically significant, and partial eta squared (ηp2) was used to report the effect size of main effects and interactions. Significant effects were probed using pairwise comparisons with the Sidak correction. Error bars in figures represent standard error of the mean (SEM). For conciseness, only effects and interactions involving drug or menstrual phase are reported in the main text (see Appendix A for other effects). Supplementary figures are in Appendix B.
Results
Exclusions
Twenty-two participants did not complete their second study session, due in part to restrictions on data collection pertaining to the COVID-19 pandemic that commenced in March 2020. In addition, two participants were missing EEG data from their first session due to file-saving errors. Excluding these participants left 56 participants for the analyses below (menstrual phase = 21, follicular phase = 19, luteal phase = 16). The included participants did not differ significantly from the excluded participants in age, education, or CCQ score (ps ≥ 0.42). For the included participants in menstrual phase group, 10 were naturally cycling and 11 were using hormonal birth control. For the biochemical assay data, only samples available from participants with useable EEG data from both study sessions (n = 56) were included in the analysis. Four individual progesterone samples (i.e., two values from the first session and two values from the second session, each from a different participant; 4/112 × 100% = 3.6% of total number of progesterone samples) were excluded for having CVs greater than 20%; for these participants, the value from their other study session was still used in the analysis to avoid reducing the sample size. Twelve sample values on the estradiol assay (11% of total samples) read below the assay’s level of detection and were replaced by the lowest standard concentration (i.e., standard 6) detected in each assay.
Biochemical assay results
Figure 1 displays the sample distribution of salivary estradiol and progesterone by menstrual group. Estradiol levels differed by menstrual phase (F(2, 53) = 5.75, p = 0.005, partial η2 = 0.18). As expected, estradiol levels were significantly higher in the follicular phase than the menstrual phase (p = 0.005), and were at intermediate levels in the luteal phase, not significantly different from the other two phases (ps ≥ 0.1; Fig. 1a). Progesterone levels also differed by menstrual phase (F(2, 53) = 5.59, p = 0.006, partial η2 = 0.17). As expected, progesterone levels were significantly higher in the luteal phase than the menstrual phase (p = 0.006), while levels in the follicular phase were marginally lower than the luteal phase (p = 0.053) and not significantly different from the menstrual phase (p > 0.5; Fig. 1b).
Resting-state electroencephalography results
See Figs. 5–7 in Appendix B for visualizations of averaged power spectra for each drug-by-menstrual phase combination.
Delta (1–4 Hz). Without CCQ in the model, there was an interaction between drug condition and region (F(1, 53) = 7.43, p = 0.009, partial η2 = 0.12), whereby caffeine reduced delta power in the parietal region (p = 0.027), but not in the frontal region (p = 0.14). Upon adding CCQ to the model, this interaction was no longer significant (p = 0.21), nor were any other drug- or phase-related main effects or interactions. A supplementary figure further supported the absence of any three-way interaction between drug condition, region, and CCQ score (Fig. 8 in Appendix B).
Theta (4–8 Hz). Without CCQ, there was an interaction between drug condition and region (F(1, 53) = 6.01, p = 0.018, partial η2 = 0.10), whereby caffeine reduced theta power more in the parietal region (p < 0.001) than in the frontal region (p = 0.036). There was also a main effect of drug condition F(1, 53) = 13.66, p = 0.001, partial η2 = 0.21) qualified by the above interaction. With CCQ included as a covariate, there were no significant drug- or phase-related effects. A supplementary figure further supported the absence of any three-way interaction between drug condition, region, and CCQ score (Fig. 9 in Appendix B). However, there was a main effect of CCQ score (F(1, 51) = 4.33, p = 0.042, partial η2 = 0.08), whereby participants with higher CCQ scores had lower global theta power.
Alpha (8–12 Hz). There were no significant drug- or phase-related main effects or interactions in either model (i.e., without CCQ or with CCQ included).
Alpha1 (8–10 Hz). Without CCQ, there was an interaction between drug condition and region (F(1, 53) = 5.47, p = 0.023, partial η2 = 0.09), whereby caffeine marginally reduced alpha1 power in the parietal region (p = 0.070), but not in the frontal region (p > 0.5). Interestingly, adding CCQ to the model revealed a significant interaction between drug condition and CCQ score (F(1, 51) = 6.54, p = 0.014, partial η2 = 0.11). As shown in Fig. 2, participants with low CCQ scores showed no effect of caffeine, whereas participants with high CCQ scores displayed a decrease in alpha1 power with the administration of caffeine.
To further visualize this drug-by-CCQ interaction, we subtracted alpha1 power values in the placebo condition from values in the caffeine condition at each ROI for each participant, producing four values per participant. These four values were averaged to create a difference score for each participant. As shown in Fig. 3, higher CCQ scores were significantly correlated with greater caffeine-induced reductions in global alpha1 power (r = − 0.36, p = 0.007).
Alpha2 (10–12 Hz). Without CCQ, there were no significant drug- or phase-related main effects or interactions. After adding CCQ as a covariate, however, there was an interaction between hemisphere, region, and phase (F(1, 51) = 3.26, p = 0.046, partial η2 = 0.11). While post hoc pairwise comparisons of the three phase groups at each hemisphere-region combination were non-significant (ps ≥ 0.22), Fig. 4 displays a trend for higher alpha2 power in the luteal phase, particularly in the right parietal region.
Beta (12–20 Hz). Without CCQ, there was a main effect of drug condition (F(1, 51) = 5.15, p = 0.027, partial η2 = 0.09), whereby caffeine reduced global beta power. Upon adding CCQ to the model, this drug effect was no longer significant (p = 0.38), and no other drug- or phase-related main effects or interactions were observed. A supplementary figure further supported the absence of any two-way interaction between drug condition and CCQ score (Fig. 10 in Appendix B).
Discussion
This study investigated the effect of caffeine on resting-state alpha activity, and whether this drug effect varied across the human menstrual cycle. We hypothesized that administering 200 mg of caffeine would reduce global alpha power (Barry et al. 2011, 2005b). We also expected that this reduction would be greater in the follicular phase, which has been associated with the lower alpha frequencies that tend to be more strongly impacted by caffeine (Baker and Colrain 2010; Barry et al. 2005b; Bazanova et al. 2017). We found partial support for these hypotheses. We discuss the interpretations, limitations, and potential significance of our work.
Effect of caffeine on resting-state electroencephalography
Consistent with our hypothesis and past research, administering caffeine reduced alpha power (Barry et al. 2011, 2005b; Meng et al. 2017). However, we only observed this reduction within the alpha1 frequency band (8–10 Hz), while power values in the alpha2 frequency band (10–12 Hz) were not significantly impacted. This finding is consistent with the interpretation that caffeine increases resting-state arousal, given that lower alpha frequencies have been typically associated with reduced arousal (Fisher et al. 2012; Knott 2001; Knott et al. 1998). This finding is similar to the results of Barry et al. (2005b), who observed that caffeine administration led to greater power reductions at lower alpha frequencies. We also found that alpha power was significantly higher in parietal regions compared to frontal regions, which is consistent with the large body of evidence on the topography of alpha waves (Başar 2012), and increases our confidence in the validity of our measurements. In addition, we observed a trend for caffeine-related alpha1 power reductions to be greater in parietal regions when compared to frontal regions, which was likely due to the higher overall alpha power in the parietal region that would provide caffeine with a greater opportunity to exert its effects.
Caffeine’s effects also varied depending on self-reported estimates of participants’ typical weekly caffeine consumption, such that individuals with higher CCQ scores tended to experience larger caffeine-induced reductions in alpha1 power (see Figs. 2 and 3). As depicted in Fig. 3, most participants’ CCQ scores were at the lower end of the scale, such that this relationship was mainly driven by a minority of participants with higher CCQ scores. Given that we asked all participants to abstain from caffeine starting at midnight the day prior to their study sessions (i.e., approximately 9 h before the onset of the study session), one possible explanation for the caffeine-by-CCQ interaction is that caffeine was reversing the withdrawal effects experienced by individuals who consume caffeine more regularly. There is some evidence that caffeine withdrawal in regular users is associated with increases in alpha power that are reversed by subsequent caffeine administration (Keane et al. 2008; Reeves et al. 1995). As seen in Fig. 2, our data do not appear to support this withdrawal-reversal interpretation, since alpha1 power levels in the placebo condition were actually lower among participants with higher CCQ scores when compared to participants with lower CCQ scores. Another possibility is that the causality of the interaction goes the other way; that is, people who have greater neurophysiological responses to caffeine experience greater effects of caffeine on arousal and are therefore more inclined to consume it. We cannot distinguish between these two possibilities with our current design, but our findings do suggest that caffeine consumption is an important moderator of caffeine’s effects on alpha activity.
It is also worth noting that including CCQ as a covariate in our models abolished any effects of caffeine on delta, theta, or beta power, and both our inferential statistics and our graphs in Appendix B indicated that there were no meaningful interactions between drug condition and CCQ score in these frequency bands. The only remaining significant interaction after controlling for CCQ was caffeine’s reduction of alpha1 power for participants with higher CCQ scores. These results reinforce the importance of accounting for individual differences in caffeine consumption; otherwise any observed effects of caffeine on resting-state EEG have the potential to be spurious.
When interpreting our EEG results, it is important to make the distinction between arousal and activation. If we consider resting-state alpha activity to be a measure of central nervous system (CNS) arousal (Barry et al. 2005a, 2005b), then our EEG results support idea that, at least for individuals with high weekly caffeine consumption, caffeine boosts arousal through neural mechanisms that work to reduce lower alpha frequencies. Barry et al. (2005b) defined activation as “the task-related mobilization of arousal” (p. 2694). Thus, individuals who have consumed caffeine may need to engage in a cognitive task to experience a benefit to their performance, though this proposal is beyond the scope of the present study.
Effect of menstrual phase
Caffeine’s effects on resting-state alpha activity did not appear to vary by menstrual phase. We measured participants’ salivary estradiol and progesterone and, as expected, we found that estradiol levels were highest in the follicular phase and progesterone levels were highest in the luteal phase (see Fig. 1; Richards 2018). The biochemical assay results support the validity of our method for determining menstrual phase (i.e., defined relative to the expected onset of their next menses). Moreover, the assay results suggest that insufficient menstrual phase delineation between groups was not a likely reason for the absence of caffeine-by-phase interaction. Importantly, we predicted that caffeine would exert stronger effects in the follicular phase because previous research has suggested that lower alpha frequencies are both more prominent in the follicular phase (Bazanova et al. 2017), and more impacted by caffeine (Barry et al. 2005b). Since we did not find differences in alpha1 power between menstrual phase groups, it is not surprising that caffeine’s effects also did not differ across menstrual phases.
However, we did observe a trend for higher alpha2 power in the luteal phase of the menstrual cycle, particularly in the right parietal region (see Fig. 4). Although this effect was marginally significant, the effect size was medium to large (partial η2 = 0.11) and the pattern is consistent with other work: some studies have shown that the luteal phase is associated with higher alpha2 power (Baker and Colrain 2010; Bazanova et al. 2014), and higher individual alpha frequency (IAF; Brötzner et al. 2014). As noted previously, higher alpha frequencies have been associated with increased arousal (Fisher et al. 2012; Knott 2001; Knott et al. 1998). Bazanova et al. (2017) reasoned that alpha2 power may be higher in the luteal phase because of elevated progesterone levels that have been shown to “[raise] the variability of high-frequency impulses” (p. 57; see also Koulen et al. 2008). Given that caffeine administration had no impact on EEG power in the alpha2 frequency band, the elevated alpha2 power in the luteal phase does not appear to be consequential when investigating caffeine’s effects on resting-state EEG during an eyes-closed paradigm.
Limitations and future directions
Our study was not without limitations. For feasibility reasons, we could not conduct a full within-subject design that tested caffeine and placebo pills at all three menstrual phases (i.e., six time points per person). Such a design could have further accounted for individual differences in menstrual cycles. Critically, we acknowledge that our lack of interaction between caffeine and menstrual phase may be due to low power, which arose from a combination of (1) the between-subject measurement of menstrual phase and (2) the limits placed on our sample size by pandemic-related dropouts. Thus, our findings should be considered preliminary until a future study can feasibly conduct the full within-subject design with a larger sample. Furthermore, we decided to preserve the sample size of our menstrual phase group by including both naturally cycling participants and participants using hormonal birth control, since hormone was not administered for 7 days per month to elicit periodic withdrawal bleeding (Christin-Maitre 2013). Nevertheless, there was still a possibility of carryover effects from hormone administration during other phases (van Heusden and Fauser 2002). Another limitation was that, as noted above, our eyes-closed resting-state paradigm was not designed to elicit task-related activity. Although our findings further our understanding of caffeine’s electrophysiological effects, it is unclear whether they would generalize to caffeine’s effects in daily life because people are typically engaged in a task when they are consuming caffeine. Other limitations of our work that should be considered in future research include lack of a subjective measure of arousal, which could have been used to corroborate the neurophysiological effects; the relatively short (i.e., 9 h) drug abstinence period prior to the EEG data collection (although lengthening this period would have likely increased the potential for caffeine-related withdrawal effects); and a lack of data about other biological variables such as participant weight. Finally, we only reported salivary estradiol and progesterone levels, but other hormones involved in the human reproductive system may be worth analyzing in future studies on caffeine, resting-state EEG, and the menstrual cycle (e.g., follicle-stimulating hormone, FSH; luteinizing hormone, LH; testosterone).
Conclusions and significance
To our knowledge, this is the first study to test the effect of caffeine administration on resting-state EEG at distinct phases of the human menstrual cycle. We provide evidence that caffeine may increase arousal through mechanisms that reduce the spectral power of lower alpha frequencies (alpha1; 8–10 Hz). Moreover, we provide preliminary evidence that this caffeine effect does not vary across the phases of the human menstrual cycle. Instead, caffeine’s dampening effects on alpha1 power were only observed in individuals with higher weekly caffeine consumption. These results have important implications for caffeine research in the field of human electrophysiology. Based on our findings, we propose that it is more important for resting-state EEG researchers to consider their participants’ baseline caffeine consumption than their menstrual cycle phase. We encourage future studies to consider incorporating menstruating individuals into their study designs so that our knowledge of caffeine’s electrophysiological effects can better generalize to the broader human population.
References
Baker FC, Colrain IM (2010) Daytime sleepiness, psychomotor performance, waking EEG spectra and evoked potentials in women with severe premenstrual syndrome. J Sleep Res https://doi.org/10.1111/j.1365-2869.2009.00782.x
Barry RJ, Clarke AR, Johnstone SJ (2011) Caffeine and opening the eyes have additive effects on resting arousal measures. Clin Neurophysiol https://doi.org/10.1016/j.clinph.2011.02.036
Barry RJ, Clarke AR, Johnstone SJ, Magee CA, Rushby JA (2007) EEG differences between eyes-closed and eyes-open resting conditions. Clin Neurophysiol https://doi.org/10.1016/j.clinph.2007.07.028
Barry RJ, Clarke AR, McCarthy R, Selikowitz M, Rushby JA (2005a). Arousal and activation in a continuous performance task: an exploration of state effects in normal children. J Psychophysiol https://doi.org/10.1027/0269-8803.19.2.91
Barry RJ, Rushby JA, Wallace MJ, Clarke AR, Johnstone SJ, Zlojutro I (2005b) Caffeine effects on resting-state arousal. Clin Neurophysiol https://doi.org/10.1016/j.clinph.2005.08.008
Başar E (2012) A review of alpha activity in integrative brain function: fundamental physiology sensory coding cognition and pathology. Int J Psychophysiol https://doi.org/10.1016/j.ijpsycho.2012.07.002
Bazanova OM, Kondratenko AV, Kuzminova OI, Muravlyova KB, Petrova SE (2014) EEG alpha indices depending on the menstrual cycle phase and salivary progesterone level. Hum Physiol https://doi.org/10.1134/S0362119714020030
Bazanova OM, Nikolenko ED, Barry RJ (2017) Reactivity of alpha rhythms to eyes opening (the Berger effect) during menstrual cycle phases. Int J Psychophysiol https://doi.org/10.1016/j.ijpsycho.2017.05.001
Brötzner CP, Klimesch W, Doppelmayr M, Zauner A, Kerschbaum HH (2014) Resting state alpha frequency is associated with menstrual cycle phase, estradiol and use of oral contraceptives. Brain Res https://doi.org/10.1016/j.brainres.2014.06.034
Chen Y, Parrish TB (2009) Caffeine dose effect on activation-induced BOLD and CBF responses. Neuroimage https://doi.org/10.1016/j.neuroimage.2009.03.012
Christin-Maitre S (2013) History of oral contraceptive drugs and their use worldwide. Clin Endocrinol Metab https://doi.org/10.1016/j.beem.2012.11.004
Cooper RK, Lawson SC, Tonkin SS, Ziegler AM, Temple JL, Hawk LW (2020) Caffeine enhances sustained attention among adolescents. Exp Clin Psychopharmacol https://doi.org/10.1037/pha0000364
Diaz S, Seron-Ferre M, Croxatto HB, Veldhuis J (1995) Neuroendocrine mechanisms of lactational infertility in women. Biol Res 28:155–163
Fisher DJ, Daniels R, Jaworska N, Knobelsdorf A, Knott VJ (2012) Effects of acute nicotine administration on resting EEG in nonsmokers. Exp Clin Psychopharmacol https://doi.org/10.1037/a0025221
Foster J (2020) The complete guide to Starbucks caffeine. Caffeine Informer. https://www.caffeineinformer.com/the-complete-guide-to-starbucks-caffeine
Hines CB (2004) Time-of-day effects on human performance. J Cathol Educ 7:390–413
Huertas F, Blasco E, Moratal C, Lupiañez J (2019) Caffeine intake modulates the functioning of the attentional networks depending on consumption habits and acute exercise demands. Sci Rep https://doi.org/10.1038/s41598-019-46524-x
Keane MA, James JE, Hogan MJ (2008) Effects of dietary caffeine on topographic EEG after controlling for withdrawal and withdrawal reversal. Neuropsychobiology https://doi.org/10.1159/000120625
Knott JV (2001) Electroencephalographic characterization of cigarette smoking behavior. Alcohol https://doi.org/10.1016/s0741-8329(00)00140-3
Knott VJ, Harr A, Ilivitsky V, Mahoney C (1998) The cholinergic basis of the smoking-induced EEG activation profile. Neuropsychobiology https://doi.org/10.1159/000026524
Koulen P, Madry C, Duncan RS, Hwang JY, Nixon E, McClung N et al (2008) Progesterone potentiates IP3-mediated calcium signaling through Akt/PKB. Cell Physiol Biochem https://doi.org/10.1159/000113758
Lein A (1979) The cycling female: her menstrual rhythm. Freeman, San Francisco https://doi.org/10.1086/411469
Meng J, Mundahl JH, Streitz TD, Maile K, Gulachek NS, He J, He B (2017) Effects of soft drinks on resting state EEG and brain-computer interface performance. IEEE Access https://doi.org/10.1109/ACCESS.2017.2751069
Murd C, Aru J, Hiio M, Luiga I, Bachmann T (2010) Caffeine enhances frontal relative negativity of slow brain potentials in a task-free experimental setup. Brain Res Bull https://doi.org/10.1016/j.brainresbull.2010.01.013
Newson JJ, Thiagarajan TC (2019) EEG frequency bands in psychiatric disorders: a review of resting state studies. Front in Hum Neurosci https://doi.org/10.3389/fnhum.2018.00521
Oldfield RC (1971) The assessment and analysis of handedness: The Edinburgh Inventory. Neuropsychologia https://doi.org/10.1007/978-0-387-79948-3_6053
Owen Jr. JA (1975) Physiology of the menstrual cycle. Am J Clin Nutr https://doi.org/10.1093/ajcn/28.4.333
Reeves RR, Struve FA, Patrick G, Bullen JA (1995) Topographic quantitative EEG measures of alpha and theta power changes during caffeine withdrawal: preliminary findings from normal subjects. Clin Electroencephalogr https://doi.org/10.1177/155005949502600306
Renda G, De Caterina R (2019) Caffeine. Princ Nutr Nutr Fundam Individ Nutr https://doi.org/10.1016/B978-0-12-804572-5.00045-8
Richards JA (2018) The ovarian cycle. In: Vitamins and Hormones, 1st edn. Elsevier Inc. https://doi.org/10.1016/bs.vh.2018.01.009
Shohet KL, Landrum RE (2001) Caffeine consumption questionnaire: a standardized measure for caffeine consumption in undergraduate students. Psychol Rep https://doi.org/10.2466/pr0.2001.89.3.521
Teichmann AT (1990) Influence of oral contraceptives on drug therapy. Am J Obstet Gynecol https://doi.org/10.1016/0002-9378(90)90563-M
van Heusden AM, Fauser BC (2002) Residual ovarian activity during oral steroid contraception. Human Reproduction Update https://doi.org/10.1093/humupd/8.4.345
Walpurger V, Pietrowsky R, Kirschbaum C, Wolf OT (2004) Effects of the menstrual cycle on auditory event-related potentials. Horm Behav https://doi.org/10.1016/j.yhbeh.2004.07.002
Funding
Support was provided by the Natural Sciences and Engineering Research Council of Canada (NSERC) through a Discovery Grant awarded to D. F. (funding reference number 2016–05394).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Aziz, J.R., Oprea, A., Bissonnette, J.N. et al. Effect of caffeine on resting-state alpha activity across the human menstrual cycle. Psychopharmacology 239, 3161–3170 (2022). https://doi.org/10.1007/s00213-022-06197-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-022-06197-3