Abstract
Rationale
Obsessive–compulsive disorder (OCD) is characterized by executive function impairment and by clinical responsivity to selective serotonin reuptake inhibitors (SSRIs). Executive planning deficits constitute a candidate endophenotype for OCD. It is not known whether this endophenotype is responsive to acute serotonin manipulation.
Objective
The study aimed to investigate the effects of acute SSRI administration on executive function in patients with OCD, first-degree relatives of patients with OCD, and healthy controls.
Methods
A randomized double-blind cross-over study assessed the effects of single-dose escitalopram (20 mg) and placebo on executive planning in 24 patients with OCD, 13 clinically unaffected first-degree relatives of patients with OCD, and 28 healthy controls. Performance on a Tower of London task measuring executive planning was assessed 4 h after oral administration of the pharmacological challenge/placebo and compared across and within groups using a mixed model analysis of variance.
Results
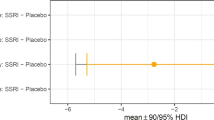
On the outcome measure of interest, i.e., the mean number of choices to obtain the correct solution, there was a marginally significant effect of group (F(2, 59) = 3.1; p = 0.052), with patients (least square (LS) mean 1.43; standard error [SE] 0.06; 95% confidence interval (CI), 1.31–1.55) and their relatives (LS mean 1.46; SE 0.08; 95% CI, 1.30–1.62) performing worse than matched healthy controls (LS mean 1.26; SE 0.05; 95% CI, 1.15–1.37) on placebo. There was a trend towards a significant group × treatment interaction (F(2, 58) = 2.8, p = 0.069), with post hoc tests showing (i) patients (p = 0.009; LS mean difference 0.23; SE 0.08) and relatives (p = 0.03; LS mean difference 0.22; SE 0.10) were more impaired compared to controls and (ii) escitalopram was associated with improved executive planning in patients with OCD (p = 0.013; LS mean difference 0.1; SE 0.04), but not other groups (both p > 0.1; controls: LS mean difference − 0.03; SE 0.04; relatives: LS mean difference 0.02; SE 0.05).
Conclusion
Our findings are consistent with a view that there is impaired executive planning in OCD and that this constitutes a behavioural endophenotype. In patients with OCD, but not in relatives, acute SSRI administration ameliorated this deficit. Further investigation is needed to understand common and differential involvement of neurochemical systems in patients with OCD and their relatives.


Similar content being viewed by others
References
Alves-Neto WC, Guapo VG, Graeff FG, Deakin JFW, Del-Ben CM (2010) Effect of escitalopram on the processing of emotional faces. Braz J Med Biol Res 43(3):285–289. https://doi.org/10.1590/s0100-879x2010005000007
American Psychiatric Association (2013) Diagnostic and statistical manual of mental disorders (5th ed.). In American Journal of Psychiatry. https://doi.org/10.1176/appi.books.9780890425596.744053
Andres S, Lazaro L, Salamero M, Boget T, Penades R, Castro-Fornieles J (2008) Changes in cognitive dysfunction in children and adolescents with obsessive-compulsive disorder after treatment. J Psychiatr Res 42(6):507–514. https://doi.org/10.1016/j.jpsychires.2007.04.004
Bari A, Theobald DE, Caprioli D, Mar AC, Aidoo-Micah A, Dalley JW, Robbins TW (2010) Serotonin modulates sensitivity to reward and negative feedback in a probabilistic reversal learning task in rats. Neuropsychopharmacology 35(6):1290–1301. https://doi.org/10.1038/npp.2009.233
Blier P, Serrano A, Scatton B (1990) Differential responsiveness of the rat dorsal and median raphe 5-HT systems to 5-HT1 receptor agonists and p-chloroamphetamine. Synapse 5(2):120–133. https://doi.org/10.1002/syn.890050206
Chamberlain SR, Fineberg NA, Blackwell AD, Clark L, Robbins TW, Sahakian BJ (2007) A neuropsychological comparison of obsessive-compulsive disorder and trichotillomania. Neuropsychologia 45(4):654–662. https://doi.org/10.1016/j.neuropsychologia.2006.07.016
Elliott R, Sahakian BJ, Matthews K, Bannerjea A, Rimmer J, Robbins TW (1997) Effects of methylphenidate on spatial working memory and planning in healthy young adults. Psychopharmacology 131(2):196–206. https://doi.org/10.1007/s002130050284
Fineberg NA, Hollander E, Pallanti S, Walitza S, Grünblatt E, Dell’Osso BM, Albert U, Geller DA, Brakoulias V, Janardhan Reddy YC, Arumugham SS, Shavitt RG, Drummond L, Grancini B, de Carlo V, Cinosi E, Chamberlain SR, Ioannidis K, Rodriguez CI, Garg K, Castle D, van Ameringen M, Stein DJ, Carmi L, Zohar J, Menchon JM (2020) Clinical advances in obsessive-compulsive disorder: a position statement by the International College of Obsessive-Compulsive Spectrum Disorders. Int Clin Psychopharmacol 35(4):173–193. https://doi.org/10.1097/YIC.0000000000000314
Gottesman II, Gould TD (2003) The endophenotype concept in psychiatry: etymology and strategic intentions. Am J Psychiatry 160(4):636–645. https://doi.org/10.1176/appi.ajp.160.4.636
Grabe HJ, Ruhrmann S, Ettelt S, Buhtz F, Hochrein A, Schulze-Rauschenbach S et al (2006) Familiality of obsessive-compulsive disorder in nonclinical and clinical subjects. Am J Psychiatry 163(11):1986–1992. https://doi.org/10.1176/ajp.2006.163.11.1986
Hajos M, Gartside SE, Sharp T (1995) Inhibition of median and dorsal raphe neurones following administration of the selective serotonin reuptake inhibitor paroxetine. Naunyn Schmiedeberg's Arch Pharmacol 351(6):624–629. https://doi.org/10.1007/bf00170162
Hedges DW, Woon FLM (2007) An emerging role for escitalopram in the treatment of obsessive-compulsive disorder. Neuropsychiatr Dis Treat 3(4):455–461
Hirschtritt ME, Bloch MH, Mathews CA (2017) Obsessive-compulsive disorder: advances in diagnosis and treatment. JAMA 317(13):1358–1367. https://doi.org/10.1001/jama.2017.2200
Lochner C, Chamberlain SR, Kidd M, Fineberg NA, Stein DJ (2016) Altered cognitive response to serotonin challenge as a candidate endophenotype for obsessive-compulsive disorder. Psychopharmacology 233(5):883–891. https://doi.org/10.1007/s00213-015-4172-y
Mataix-Cols D, Alonso P, Pifarre J, Menchon JM, Vallejo J (2002) Neuropsychological performance in medicated vs. unmedicated patients with obsessive-compulsive disorder. Psychiatry Res 109(3):255–264. https://doi.org/10.1016/s0165-1781(02)00024-0
Nestadt G, Samuels J, Riddle M, Bienvenu OJ 3rd, Liang KY, LaBuda M et al (2000) A family study of obsessive-compulsive disorder. Arch Gen Psychiatry 57(4):358–363. https://doi.org/10.1001/archpsyc.57.4.358
Nielen MMA, Den Boer JA (2003) Neuropsychological performance of OCD patients before and after treatment with fluoxetine: evidence for persistent cognitive deficits. Psychol Med 33(5):917–925. https://doi.org/10.1017/s0033291703007682
Owen AM, Downes JJ, Sahakian BJ, Polkey CE, Robbins TW (1990) Planning and spatial working memory following frontal lobe lesions in man. Neuropsychologia 28(10):1021–1034. https://doi.org/10.1016/0028-3932(90)90137-d
Pauls DL, Alsobrook JP 2nd, Goodman W, Rasmussen S, Leckman JF (1995) A family study of obsessive-compulsive disorder. Am J Psychiatry 152(1):76–84. https://doi.org/10.1176/ajp.152.1.76
Rao N (2007) The clinical pharmacokinetics of escitalopram. Clin Pharmacokinet 46(4):281–290. https://doi.org/10.2165/00003088-200746040-00002
Reeves SJ, Mehta MA, Montgomery AJ, Amiras D, Egerton A, Howard RJ, Grasby PM (2007) Striatal dopamine (D2) receptor availability predicts socially desirable responding. NeuroImage 34(4):1782–1789. https://doi.org/10.1016/j.neuroimage.2006.10.042
Sanchez C, Bergqvist PBF, Brennum LT, Gupta S, Hogg S, Larsen A, Wiborg O (2003) Escitalopram, the S-(+)-enantiomer of citalopram, is a selective serotonin reuptake inhibitor with potent effects in animal models predictive of antidepressant and anxiolytic activities. Psychopharmacology 167(4):353–362. https://doi.org/10.1007/s00213-002-1364-z
Sayyah M, Eslami K, AlaiShehni S, Kouti L (2016) Cognitive function before and during treatment with selective serotonin reuptake inhibitors in patients with depression or obsessive-compulsive disorder. Psychiatry J 2016:5480391–5480394. https://doi.org/10.1155/2016/5480391
Shallice T (1982) Specific impairments of planning. Philos Trans R Soc Lond Ser B Biol Sci 298(1089):199–209. https://doi.org/10.1098/rstb.1982.0082
Skandali N, Rowe JB, Voon V, Deakin JB, Cardinal RN, Cormack F, Passamonti L, Bevan-Jones WR, Regenthal R, Chamberlain SR, Robbins TW, Sahakian BJ (2018) Dissociable effects of acute SSRI (escitalopram) on executive, learning and emotional functions in healthy humans. Neuropsychopharmacology 43(13):2645–2651. https://doi.org/10.1038/s41386-018-0229-z
Soomro GM, Altman D, Rajagopal S, Oakley-Browne M (2008) Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD). Cochrane Database Syst Rev 1:CD001765. https://doi.org/10.1002/14651858.CD001765.pub3
Stein DJ, Carey PD, Lochner C, Seedat S, Fineberg N, Andersen EW (2008) Escitalopram in obsessive-compulsive disorder: response of symptom dimensions to pharmacotherapy. CNS Spectr 13(6):492–498. https://doi.org/10.1017/S1092852900016722
Vaghi MM, Hampshire A, Fineberg NA, Kaser M, Bruhl AB, Sahakian BJ et al (2017) Hypoactivation and dysconnectivity of a frontostriatal circuit during goal-directed planning as an endophenotype for obsessive-compulsive disorder. Biol Psychiatry Cogn Neurosci Neuroimaging 2(8):655–663. https://doi.org/10.1016/j.bpsc.2017.05.005
van den Heuvel OA, Veltman DJ, Groenewegen HJ, Cath DC, van Balkom AJLM, van Hartskamp J, Barkhof F, van Dyck R (2005) Frontal-striatal dysfunction during planning in obsessive-compulsive disorder. Arch Gen Psychiatry 62(3):301–309. https://doi.org/10.1001/archpsyc.62.3.301
Waugh J, Goa KL (2003) Escitalopram: a review of its use in the management of major depressive and anxiety disorders. CNS Drugs 17(5):343–362. https://doi.org/10.2165/00023210-200317050-00004
Zartaloudi E, Laws KR, Bramon E (2019) Endophenotypes of executive functions in obsessive compulsive disorder? A meta-analysis in unaffected relatives. Psychiatr Genet 29(6):211–219. https://doi.org/10.1097/YPG.0000000000000241
Acknowledgements
We are grateful to the European College of Neuropsychopharmacology (ECNP) Obsessive-Compulsive and Related Disorders Research Network (OCRN), the International College of Obsessive-Compulsive Spectrum Disorders (ICOCS), and the European Cooperation in Science and Technology COST Action (CA16207) European Network for Problematic Usage of the Internet for providing networking support. Dr. Chamberlain’s consults for Promentis and Ieso Digital Health. Dr. Fineberg leads an NHS treatment service for OCD. She holds Board membership for various registered charities linked to OCD. She gives expert advice on psychopharmacology to the UK MHRA. Dr. Robbins consults for Cambridge Cognition, Unilever, Shionogi, Tacheda, Greenfield Bioventures, and Cassava.
Funding
The authors received support from the Medical Research Council of South Africa (Lochner and Stein), the Obsessive-Compulsive Foundation (Stein), and the National Research Foundation of South Africa (Lochner) and an unrestricted grant from Lundbeck H/S. Dr. Chamberlain’s role in this project was funded by a Wellcome Trust Clinical Fellowship (110049/Z/15/Z). Dr. Fineberg declares that in the past 3 years, she had held research or networking grants from the ECNP, UK NIHR, EU H2020, MRC, and University of Hertfordshire. In the past 3 years, she had accepted a paid speaking engagement in a webinar sponsored by Abbott. Previously, she had accepted paid speaking engagements in various industry supported symposia and have recruited patients for various industry-sponsored studies in the field of OCD treatment. Dr. Robbins is supported by Wellcome Trust Grant 146301/Z/14/Z/. He holds research grants from Shionogi and GlaxoSmithKline. Dr. Stein has received research grants and/or consultancy honoraria from Lundbeck and Sun.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(DOCX 48 kb)
Rights and permissions
About this article
Cite this article
Lochner, C., Chamberlain, S.R., Kidd, M. et al. The effects of acute serotonin challenge on executive planning in patients with obsessive–compulsive disorder (OCD), their first-degree relatives, and healthy controls. Psychopharmacology 237, 3117–3123 (2020). https://doi.org/10.1007/s00213-020-05597-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00213-020-05597-7