Abstract
The vagal regulation of cardiac function involves acetylcholine (ACh) receptor activation followed by negative chronotropic and negative as well as positive inotropic effects. The resulting signaling pathways may include Gi/o protein-coupled reduction in adenylyl cyclase (AC) activity, direct Gi/o protein-coupled activation of ACh-activated potassium current (IKACh), inhibition of L-type calcium ion channels, and/or the activation of protein phosphatases. Here, we studied the role of the protein phosphatases 1 (PP1) and 2A (PP2A) for muscarinic receptor signaling in isolated atrial preparations of transgenic mice with cardiomyocyte-specific overexpression of either the catalytic subunit of PP2A (PP2A-TG) or the inhibitor-2 (I2) of PP1 (I2-TG) or in double transgenic mice overexpressing both PP2A and I2 (DT). In mouse left atrial preparations, carbachol (CCh), cumulatively applied (1 nM–10 µM), exerted at low concentrations a negative inotropic effect followed by a positive inotropic effect at higher concentrations. This biphasic effect was noted with CCh alone as well as when CCh was added after β-adrenergic pre-stimulation with isoprenaline (1 µM). Whereas the response to stimulation of β-adrenoceptors or adenosine receptors (used as controls) was changed in PP2A-TG, the response to CCh was unaffected in atrial preparations from all transgenic models studied here. Therefore, the present data tentatively indicate that neither PP2A nor PP1, but possibly other protein phosphatases, is involved in the muscarinic receptor-induced inotropic and chronotropic effects in the mouse heart.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Acetylcholine (ACh) binds to muscarinic ACh receptors expressed in the sarcolemma of cardiomyocytes. The Gi-coupled M2 ACh receptor is the main muscarinic ACh receptor in the mammalian heart, expressed in the atrium and ventricle as well as in the conduction system including the sinoatrial (SA) node and atrioventricular (AV) node (overview in Saw et al. (2018)). Effects of M2 receptor stimulation in the heart are hyperpolarization in the SA node and a slowed spontaneous depolarization resulting in reduced sinus rate, a shortened action potential duration and probably as a result a decreased contractile force in the atrium, and a decreased conduction velocity in the AV node (Dhein et al. 2001).
Recent studies have demonstrated that muscarinic ACh receptor activation in sinoatrial nodal cells leads to a decrease in beating rate either via reduced activation of the hyperpolarization-activated current (If) or L-type Ca2+ current by a Gi-mediated reduction in adenylyl cyclase (AC) activity or via direct Gi-coupled activation of ACh-activated potassium current (IK.ACh) (Lyashkov et al. 2009).
In left atrial preparations of wild-type mice, carbachol (CCh), an ACh analogue, induced a transient negative inotropic effect followed by a positive inotropic response (Kitazawa et al. 2009). Using antagonists or muscarinic M2 or M3 receptor single knockout mice or M2 and M3 muscarinic receptor double knockout mice, the authors demonstrated that the negative inotropic effect of CCh was M2 receptor–mediated and the positive inotropic effect of CCh was M3 receptor–mediated (Kitazawa et al. 2009).
In guinea pig cardiac preparations (isolated perfused heart or isolated ventricular cardiomyocytes), acetylcholine decreased the isoprenaline-stimulated phosphorylation of phospholamban (PLB) and troponin inhibitor (TnI), but without reducing cAMP levels or the protein kinase A activity ratio (Gupta et al. 1994). The addition of the protein phosphatase inhibitor okadaic acid blocked the ACh-mediated effects on protein phosphorylation. It was suggested by the authors that ACh reduced protein phosphorylation independently of cAMP (Gupta et al. 1994). Later, the data were expanded to inotropic effects in guinea pig papillary muscles. Carbachol reduced the positive inotropic effect of isoprenaline and these effects were blocked by inhibition of phosphatases. Therefore, it was suggested that the ventricular cardiac effects of muscarine receptor stimulation involve protein phosphatase activation (Neumann et al. 1995; Neumann and Scholz 1998). Similar results were reported in canine ventricular preparations where cantharidin attenuated the carbachol-induced negative inotropic effect (Chu et al. 2003).
Here, we tested the hypothesis that protein phosphatases are involved in the cardiac response to muscarinic receptor stimulation. Since it is currently not known which protein phosphatases are involved, we started to test this hypothesis by studying the inotropic and chronotropic effects in isolated atrial preparations of PP2A-transgenic mice (PP2A-TG), PP1-inhibitor-2 mice (I2-TG), double transgenic mice (PP2A-TGxI2-TG = DT), and as control wild-type mice (WT). In I2-TG mice, we noted not only a reduced cardiac PP1 activity, but also a reduced PP2A activity (Krause et al. 2018). This effect has been neglected up to now. Here, we generated the double transgenic model with reduced cardiac PP1 activity (like in I2-TG), but increased PP2A activity (like in PP2A-TG). For the experimental setup, our choice fell on atrial preparations, firstly because carbachol is effective under both basal and adrenergically stimulated conditions and secondly because in isolated right atrial preparations, the effect on the sinus node can be elegantly examined. Since muscarinic receptor stimulation usually, in mice and man, results in concentration- and time-dependent negative and positive inotropic effects in cardiac preparations, we compared the response to muscarinic receptor stimulation with the response to β-adrenoceptor stimulation and A1-adenosine receptor stimulation.
Materials and methods
Transgenic mice
For this study, transgenic mice with cardiomyocyte-specific overexpression either of the catalytic subunit of PP2A (PP2A-TG) (Gergs et al. 2004) or of the inhibitor-2 of PP1 (I2-TG) (Krause et al. 2018) were used. Some experiments were performed with double transgenic mice (PP2A-TGxI2-TG = DT) obtained by crossbreeding PP2A-TG with I2-TG mice. Transgene-positive mice (CD1 background) were routinely identified by PCR assay of ear punch genomic DNA. On the protein level, the overexpression of the catalytic subunit of PP2A was 2.5-fold in PP2A-TG hearts (Gergs et al. 2004) and the overexpression of I2PP1 was ninefold in I2-TG hearts (Krause et al. 2018). The phenotypes of the mouse models have been described before (Cheng et al. 2010; Gergs et al. 2004, 2022; Hoehn et al. 2015; Wijnker et al. 2011). Briefly, the life span and fertility of the monotransgenic mice were unchanged compared to WT, and the life span of DT mice (monitored up to the date of the experiment) was also unchanged compared to WT. PP2A-TG mice develop age-dependently cardiac hypertrophy, decreased cardiac function, and diminished response to β-adrenergic stimulation (Gergs et al. 2004). The phenotype of I2-TG mice is unremarkable compared to WT (Krause et al. 2018). For the experiments, 6 to 8-month-old mice of each gender were used (we did not detect any difference between cardiac preparations from male or female mice during this study). The investigation conforms to the Guide for the Care and Use of Laboratory Animals published by the National Research Council (US) 2011 (National Academies Press (US) 2011). Animals were maintained and handled according to approved protocols of the animal welfare committees of the Martin-Luther University of Halle-Wittenberg, Germany. All efforts were made to minimize suffering.
Mouse atrial preparations
A force of contraction of mouse left and right atrial preparations was recorded under isometric conditions as often described by our group (Gergs et al. 2013, 2017, 2019b, 2021; Neumann et al. 2003). In brief, mice were euthanatized by i. p. injection of pentobarbital sodium (50 mg kg−1). Then, hearts were excised and the right and left atria were isolated and mounted in 10-ml organ baths containing a Tyrodes’s solution composed of 119.8 mM NaCl 5.4 mM KCl, 1.8 mM CaCl2, 1.05 mM MgCl2, 0.42 mM NaH2PO4, 22.6 mM NaHCO3, 0.05 mM Na2EDTA, 0.28 mM ascorbic acid, and 5.05 mM glucose. The bathing solution was continuously gassed with 95% O2 and 5% CO2 to stabilize the pH 7.4 and maintained at 37 °C. A force of contraction (FOC) was measured with inductive force transducers connected to a bridge amplifier and digitizer (PowerLab system, ADInstruments, Oxford, UK). Each atrial preparation was stretched to the length of its individual maximal FOC. The left atrial preparations were electrically stimulated at 1 Hz (field stimulation) with rectangular pulses of 5 ms duration and a voltage that was ~ 10–20% over the threshold of initiation of contraction. The right atrial preparations were prepared with an intact sinus node to maintain spontaneous beating and were used to study chronotropic effects. Before contraction experiments with carbachol were started, adenosine deaminase (1 µg·ml−1 for 30 min) was added to avoid any interferences of residual or released adenosine (Boknik et al. 2009). From the recorded force of contraction, the first derivate (dF/dt) and the time parameters of single contractions (left atrial preparations) and the beating rate (right atrial preparations) were calculated using the chart software (ADInstruments, Oxford, UK).
This biphasic response to CCh was analyzed by calculation of the relative change in the force of contraction for each CCh concentration normalized to the individual baseline force before the effect begins as described earlier (Froldi et al. 1994; Gergs et al. 2008). That means in detail: the “pre-drug value” for the negative inotropic effect of the concentration Xn is the positive inotropic effect of the concentration before (Xn-1). Correspondingly, the “pre-drug value” for the positive inotropic effect of the concentration Xn is the negative inotropic effect of the very same concentration (Xn). This procedure was performed for all concentrations Xn(n = 10−9 to 10−5). These negative and positive relative changes in force were added, respectively, to get a concentration–response curve and expressed in %.
Protein phosphatase assays
Protein phosphatase activity was measured with [32P]-phosphorylase a as substrate as described before (Gergs et al. 2004). Complete frozen heart samples were pulverized in liquid nitrogen. Then, the tissue powder was homogenized in a homogenization buffer containing 20 mM Tris–HCl (pH 7.4), 5 mM EDTA, 2 mM EGTA, 0.1% (v/v) β-mercaptoethanol, 0.5 mM phenylmethylsulfonyl fluoride, and 1 mM benzamidine three times for 30 s each with a Polytron PT-10 (Kinematica, Luzern, Switzerland) at 4 °C. Finally, the homogenate was cleared by centrifugation (10 min; 14,000 × g; 4 °C) and the protein concentration of the supernatant was measured using a Bradford assay. The homogenates were diluted to 0.5 mg protein/ml in 50 mM Tris–HCl (pH 7.4) and aliquots of 10 µl (containing 5 µg of protein) were continued to be used. To differentiate between PP1 and PP2A activity, 10 nM okadaic acid (buffer only for the total activity) was added to the half of samples and preincubated for 10 min at 30 °C. Twenty microliters of a reaction mixture containing the [32P]-labeled substrate and 2.5 mM Tris–HCl (pH 7.4), 12.5 mM caffeine, 0.25 mM EDTA, and 0.25% (v/v) β-mercaptoethanol were added to the preincubated homogenates. After 30 min at 30 °C, the reaction was terminated by adding 20 µl of 50% trichloroacetic acid on ice together with 30 µl of 20 mg/ml bovine serum albumin. The precipitated proteins were sedimented by centrifugation (14,000 × g; 5 min; 4 °C) and an aliquot of the supernatants with the released phosphate was counted in a liquid scintillation counter. The samples including 10 nM okadaic acid were representative mainly for the PP1 activity. The PP2A activity was calculated by: total activity – activity with okadaic acid.
Reagents
(-)-Isoprenaline ( +)-bitartrate, carbachol, and R-PIA (R(-)-N(6)-(2)-phenylisopropyl adenosine) were purchased from Sigma-Aldrich (Munich, Germany). All other chemicals used were of the highest purity grade commercially available and demineralized water was used throughout the experiments.
Statistics
All data are presented as means ± SEM. The statistical analyses were performed either by the Student’s t-test if appropriate or by the analysis of variance (ANOVA) followed by Tukey’s multiple comparisons test for more than two variables. For small sample groups (n < 6), a non-parametric test was chosen. A p-value < 0.05 was set as the statistical significance level. For statistical calculations and graphical presentations, the software GraphPad Prism 9.0 (GraphPad Software, San Diego, CA, USA) was used.
Results
We carried out contraction experiments under isometric conditions in isolated atrial preparations from WT, PP2A-TG, I2-TG, and DT mice. The left atria were field-stimulated at 1 Hz to analyze the force of contraction and the spontaneously beating right atria were used to analyze the beating rate, more specifically to analyze the effects on the sinus node.
Effects of isoprenaline
In isolated left atrial preparations, cumulatively applied isoprenaline (1 nM – 1 µM) only increased the force of contraction. The potency of isoprenaline to induce a positive inotropic effect was comparable in all genotypes tested (-logEC50: 7.03–7.14) (Fig. 1A, B). Whereas the potency of isoprenaline was not different, the efficacy of isoprenaline was increased in I2-TG and DT left atrial preparations (Fig. 1A, B). In spontaneously beating right atrial preparations, the effects were different: cumulatively applied isoprenaline (1 nM–1 µM) increased the beating rate from about 300 bpm to the same maximum (about 600 bpm) in all genotypes (Fig. 1C), but the potency of isoprenaline to induce a positive chronotropic effect was reduced clearly in PP2A-TG and to a lesser extent in DT (Fig. 1D).
Summarized concentration–response curves for the effect of isoprenaline on force of contraction in electrically driven (1 Hz) left atrial preparations (A, B) and on the beating rate in right atrial preparations (C, D) from PP2A-TG, I2-TG, DT, and WT. Numbers in brackets give the number of experiments. Ctr is the pre-drug value. A Force of contraction in milli Newton (mN) and B shows the same data in % of control (Ctr) to visualize the efficiency of isoprenaline. *First p < 0.05 vs. Ctr; #p < 0.05 vs. WT. C Beating rate in beats per minute (bpm). *First p < 0.05 vs. Ctr; #p < 0.05 vs. WT and I2-TG. D The logarithm of the EC50 values demonstrates the potency of isoprenaline to increase the beating rate in right atrial preparations. Significant differences (p < 0.05) are indicated by brackets
Effects of carbachol
In mouse left atrial preparations, cumulatively applied CCh (1 nM–10 µM) exerted a negative inotropic effect followed by a positive inotropic effect at higher concentrations (Fig. 2A). Moreover, even at a given low concentration of CCh, there was an initial fall in force of contraction followed over time by an increase in force of contraction that usually did not surpass pre-drug value. This biphasic response makes it difficult to independently quantitate the negative and positive inotropic effects of CCh. To dissect the differences, we calculated the relative change in the force of contraction for each CCh concentration normalized to the individual baseline force before the effect begins as others and we ourselves have done in previous studies (Froldi et al. 1994; Gergs et al. 2008). The negative and positive relative changes in force were added, respectively, to get a concentration–response curve. A drawback of this method is that both negative and positive inotropic effects were underestimated, but the primary aim was to compare the response to CCh in different genotypes rather than to measure the exact inotropic response.
Concentration–response curves for the effect of carbachol on force of contraction in electrically driven (1 Hz) left atrial preparations from PP2A-TG, I2-TG, DT, and WT. Numbers in brackets give the number of experiments. Ctr is the value before carbachol application. A Original recordings demonstrate the biphasic effect of carbachol. Ordinates: force of contraction (mN); horizontal bars: time (min). B Only the negative inotropic effect of carbachol is plotted and C only the positive inotropic effect of carbachol is plotted as delta milli Newton in % of pre-drug value, respectively, as described in the method section. *First p < 0.05 vs. Ctr; #p < 0.05 vs. WT and I2-TG
In the first set of experiments, CCh was cumulatively applied alone (that means without any pre-stimulation). The potency of CCh for the negative (-logEC50: 6.4–6.9) or positive (-logEC50: 6.5–6.7) inotropic effect in left atrial preparations was not different between genotypes (Fig. 2B, C). But the maximum response to CCh was reduced in left atrial preparations from PP2A-TG compared to WT and I2-TG (p < 0.05 for the negative inotropic effect; not significant for the positive inotropic effect).
Next, the atrial preparations were pre-stimulated by 1 µM isoprenaline before CCh was applied. Also in this setting, CCh had a biphasic effect in left atrial preparations (Fig. 3A). Again, the potency of CCh for the negative (-logEC50: 6.4–6.9) and probably for the positive (EC50: not calculable because of a missing plateau at the end of the concentration–response curve) inotropic effect was not different between genotypes (Fig. 3B, C). The maximum negative inotropic response to CCh was increased in left atrial preparations from I2-TG and DT compared to WT and PP2A-TG (Fig. 3B).
Concentration–response curves for the effect of isoprenaline followed by carbachol on force of contraction in electrically driven (1 Hz) left atrial preparations from PP2A-TG, I2-TG, DT, and WT. Numbers in brackets give the number of experiments. Iso indicates the maximum response to isoprenaline (1 µM) and was used here as control for the carbachol application. A Original recordings demonstrate that the biphasic effect of carbachol is still present, but shifted to higher concentrations. Ordinates: force of contraction (mN); horizontal bars: time (min). B Only the negative inotropic effect of carbachol after pre-stimulation with Iso is plotted and C only the positive inotropic effect of carbachol after pre-stimulation with Iso is plotted as delta milli Newton in % of pre-drug value, respectively, as described in the method section. *First p < 0.05 vs. Iso; #p < 0.05 vs. WT and PP2A-TG
In right atrial preparations, CCh alone exerted a negative chronotropic effect that was not different between the genotypes (-logEC50: 6.0–6.5) (Fig. 4A). Similar results were found in isoprenaline-stimulated right atrial preparations, where the negative chronotropic effect of CCh was again not different between the genotypes (-logEC50: 6.2–6.7) (Fig. 4B).
Summarized concentration–response curves for the effect of carbachol alone (A) or after pre-stimulation with 1 µM isoprenaline (Iso) (B) on the beating rate in right atrial preparations from PP2A-TG, I2-TG, DT, and WT are shown. Numbers in brackets give the number of experiments. Ctr is the pre-drug value. Iso indicates the maximum response to isoprenaline and was used here as control for the carbachol application. *First p < 0.05 vs. Ctr or Iso
Effects of R-PIA
For comparison, we analyzed the effects of the adenosine A1 receptor agonist R-PIA. R-PIA only exerts negative inotropic and chronotropic effects in atrial preparations from WT mice probably because a single receptor is involved (Neumann et al. 1999). For these experiments, only WT, PP2A-TG, and I2-TG mice were available. First, R-PIA was cumulatively applied (1 nM–1 µM) alone (that means without any pre-stimulation). The potency and efficiency of R-PIA for the negative inotropic effect in left atrial preparations or the negative chronotropic effect in right atrial preparations were not different between genotypes (Fig. 5). Next, atrial preparations were pre-stimulated with 1 µM isoprenaline before R-PIA was cumulatively applied. Now, in PP2A-TG left atrial preparations, the negative inotropic effect of R-PIA was more pronounced compared to WT and I2-TG (Fig. 6A, B). In isoprenaline-stimulated right atrial preparations, the negative chronotropic effect of R-PIA was not different between the genotypes (Fig. 6C, D).
Summarized concentration–response curves for the negative inotropic and chronotropic effect of the adenosine receptor agonist R-PIA in electrically driven (1 Hz) left atrial preparations (A, B) and in right atrial preparations (C), respectively, from PP2A-TG, I2-TG, and WT. Numbers in brackets give the number of experiments. Ctr is the value before R-PIA application. A Force of contraction in % of control (Ctr). B The logarithm of the EC50 values demonstrates that the negative inotropic effect of R-PIA alone was not different between the mouse models. C Beating rate in beats per minute (bpm). *First p < 0.05 vs. Ctr
Summarized concentration–response curves for the negative inotropic and chronotropic effect of the adenosine receptor agonist R-PIA after pre-stimulation with 1 µM isoprenaline (Iso) in electrically driven (1 Hz) left atrial preparations (A, B) and in right atrial preparations (C, D), respectively, from PP2A-TG, I2-TG, and WT. Numbers in brackets give the number of experiments. Iso indicates the maximum response to isoprenaline and was used here as control for the R-PIA application. A Force of contraction in % of Iso. B The logarithm of the EC50 values demonstrates that the anti-adrenergic effect of R-PIA is enhanced in left atrial preparations from PP2A-TG compared to WT and I2-TG. Significant differences (p < 0.05) are indicated by brackets. C Beating rate in beats per minute (bpm). D The logarithm of the EC50 values demonstrates that the negative chronotropic effect of R-PIA after pre-stimulation with Iso was not different in right atrial preparations. *First p < 0.05 vs. Iso; #p < 0.05 vs. PP2A-TG
Protein phosphatase activity
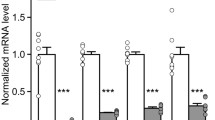
The activity of protein phosphatases was measured in whole heart homogenates of each genotype, using [32P]-phosphorylase a as substrate. By this substrate, mainly the activities of PP1 and PP2A are measured. To differentiate between PP1 and PP2A activity, 10 nM of the protein phosphatase inhibitor okadaic acid was used, because at the given low concentration of okadaic acid, PP2A activity is completely blocked whereas PP1 is still active (Gergs et al. 2004). Here, the relation of PP1 activity to PP2A activity was 2 to 1 in WT samples and nearly 1 to 1 in PP2A-TG hearts. In I2-TG and DT, PP1 activity was almost completely blocked, whereas the PP2A activity in I2-TG and DT was in the range of WT and PP2A-TG, respectively (Fig. 7).
Protein phosphatase activity in whole heart homogenates. [32P]-phosphorylase a was used as a substrate, mainly metabolized by PP2A and PP1. The release of [32P]-Pi was measured as counts per microgram protein (cpm/µg protein). Of the protein phosphatase inhibitor okadaic acid, 10 nM was used to differentiate between PP1 and PP2A activity. Significant differences (p < 0.05) are indicated by brackets. N = 4–8
Discussion
All regions of the mammalian heart are parasympathetically innervated and the supraventricular tissues are more densely innervated than the ventricles. Vagal activation leads to stimulation of cardiac muscarinic receptors that modulate the activity of the sinus node, the atrioventricular conduction, and also the force of contraction (Dhein et al. 2001). The M2 muscarinic receptor is the predominant muscarinic receptor in the mammalian heart and its M2 receptors are abundantly expressed in the atrium (Lymperopoulos et al. 2021; Osipov et al. 2023). The M2 receptor signaling involves at least Gi/o-mediated inhibition (or stimulation) of ACs, indirect (cAMP-dependent) or direct (cAMP-independent mediated by the α-subunit of Go) inhibition of If, and activation of IK.ACh (Dhein et al. 2001; Yatani et al. 1990). Moreover, there is a vast literature that cGMP concentrations are increased by acetylcholine (Dawson et al. 2008; Lang et al. 2007; Vente 2004). It was proposed that M2 receptors can inhibit as well as stimulate ACs depending on the AC isoform. AC isoforms 5 and 6 can be inhibited by M2 receptors via the αi/o subunit of Gi/o and AC isoforms 4 and 7 can be stimulated by M2 receptors via the βγ subunit of Gi/o (Harvey and Belevych 2003).
Already more than 20 years ago, it was clear that other muscarinic receptors, different from the M2 receptor, exist in the mouse and human heart (overview in (Brodde and Michel 1999)). For instance, the presence of cardiac M3 muscarinic receptors has been demonstrated by functional and molecular biological studies, for example, in humans (Hellgren et al. 2000; Oberhauser et al. 2001), in rats (Bognar et al. 1990; Pönicke et al. 2003), or in mice (Hara et al. 2009; Kitazawa et al. 2009). Originally, no M1 receptor could be detected in the human heart (Hellgren et al. 2000), although the presence of the M1 receptor had been suggested based on functional data (Du et al. 1995). Meanwhile, the presence of Gq-coupled M1 receptors that regulate the atrial IK,ACh has been described in the human atrium (Heijman et al. 2018). While it is accepted that the M2 receptor exists in cardiomyocytes, the precise cellular localization of the M3 receptors, however, is not completely clear (Brodde and Michel 1999; Dhein et al. 2001; Kitazawa et al. 2009). Pönicke et al. (2003) found functional evidence for the presence of M3 receptors in isolated rat ventricular myocytes. In contrast, in mouse atria, the presence of M3 receptors was located in the endocardial endothelium (Hara et al. 2009). To summarize the current data, M1 and M3 receptors seem to be expressed in cardiomyocytes, but less abundant than M2 receptors and with species differences (M1 more in human hearts, M3 more in rodent hearts) (Lymperopoulos et al. 2021; Osipov et al. 2023). While many questions remain regarding the expression of muscarinic receptors in the heart, the expression of numerous protein phosphatases, including PP2A and PP1, in cardiomyocytes has been widely described (Gergs et al. 2019a; Heijman et al. 2013, 2017; Herzig and Neumann 2000; Neumann et al. 2021).
Nonetheless, muscarinic receptor signaling pathways are complex and there is still debate as to which receptor and which signaling pathway is associated with which function. Briefly summarized, the negative chronotropic and inotropic effects are commonly associated with the M2 receptor, and the positive inotropic effects in the mouse atrium are associated with the M3 receptor. Relatively little attention has been paid to date to the protein phosphatases as the regulator of muscarinic receptor signaling. But there is some evidence for the involvement of protein phosphatases. As mentioned in “Introduction,” in guinea pig perfused hearts and ventricular cardiomyocytes, ACh reduced via M2 receptors the isoprenaline-induced phosphorylation of PLB and TnI. These effects were independent of cAMP and PKA and were blocked by the protein phosphatase inhibitor okadaic acid (Gupta et al. 1994). In mouse and canine cardiomyocytes, M2 receptor stimulation led to an increase in the phosphorylation status of the ryanodine receptor 2 (RyR2) at serine-2808, while dephosphorylation of serine-2814 has been associated with activation of M3 receptors (Ho et al. 2016). The authors concluded that muscarinic receptor stimulation enhances the efficiency of cardiac sarcoplasmic reticulum calcium cycling by changes in the phosphorylation status of RyR2 at serine-2808 and serine-2814 (Ho et al. 2016). This mechanism may be influenced by protein phosphatases because, for example, PP2A decreases the phosphorylation status of RyR2 at serine-2808 (Hoehn et al. 2015). The phosphatase inhibitor sodium fluoride attenuated the negative inotropic effect of CCh in isoprenaline-stimulated guinea pig papillary muscles and these effects were reversed by the addition of deferoxamine that complexes and thus inactivates fluoride (Neumann et al. 1995; Neumann and Scholz 1998). In the canine ventricular myocardium, activation of a cantharidin-sensitive phosphatase was involved in the negative inotropic effects of CCh (Chu et al. 2003). A limitation of the study from Chu et al. (2003) was that only with higher concentrations of cantharidin (30 µM), an effect was notable. Based on the fact that the IC50 values of cantharidin for PP1 (IC50 = 1.7 µM) and PP2A (IC50 = 0.16 µM) are much lower, other protein phosphatases than PP1 and PP2A may be involved, for example, PP2B that is inhibited by a more than 500-fold higher concentration of cantharidin than PP1 (Herzig and Neumann 2000; Honkanen 1993; Neumann et al. 2021).
While the regulation of signal transduction through phosphorylation has been widely studied, little attention has been paid to the phosphorylation of the receptor itself. It is known that the activated M2 receptor is phosphorylated by G protein-coupled receptor kinases (GRK2/3) and that this phosphorylation regulates the formation of receptor-arrestin complexes initiating G protein–independent signaling (Drube et al. 2022; Li et al. 2015). Moreover, also the inactive receptor can be phosphorylated by GRK5/6. It is assumed that this phosphorylation in the absence of agonists mediates the basal receptor cycling and arrestin-mediated signaling (Li et al. 2015). As good as nothing is known about the involvement of specific protein phosphatases, for example, to reverse the GRK effects. If PP2A or PP1 are involved in GRK-mediated effects, we should see differences in our transgenic mouse models.
Motivated by these previous studies, we examined in the present work the atrial effects of muscarinic receptor stimulation in mice with either increased PP2A activity (Gergs et al. 2004) or with reduced PP1 activity (Brüchert et al. 2008; Dörner et al. 2021; Grote-Wessels et al. 2008; Krause et al. 2018) in the heart. Here, we have not measured the atrial protein phosphatase activity, but from our whole heart data presented here and from previous studies we know that in I2-TG hearts, not only PP1 activity is reduced but also, presumably due to counter-regulatory effects, the PP2A activity (Brüchert et al. 2008; Kirchhefer et al. 2005; Krause et al. 2018). Therefore, we crossbred the PP2A-TG with I2-TG mice, and in these double-transgenic animals, the cardiac activity of PP2A was shifted towards the activity found in monotransgenic PP2A-TG, whereas the PP1 activity remained as low as in the monotransgenic I2-TG. On the functional level, there seems to be no obvious interaction between PP2A and I2PP1, as the PP2A-induced cardiac hypertrophy was not affected by co-expression of I2PP1 (Brüchert et al. 2008). In contrast, in double transgenic PP1xI2 mice, the PP1-induced heart failure could be completely abolished by co-expression of I2PP1 (Brüchert et al. 2008). A more general inhibition of protein phosphatases in the heart, for example, with sodium fluoride or cantharidin, attenuated the negative inotropic effects of CCh or R-PIA (Chu et al. 2003; Neumann et al. 1995; Neumann and Scholz 1998). Therefore, we initially assumed that, if PP1 is involved, in I2-TG hearts, the effect of protein phosphatase inhibitors may be mimicked, at least in part, by the transgene. That is, the negative inotropic/chronotropic effect of CCh or R-PIA should be attenuated in I2-TG. On the other hand, if PP2A is involved, the effects of CCh and R-PIA may be potentiated in PP2A-TG or in DT. Taken together, our data suggest that neither PP2A nor PP1 are involved in the cardiac carbachol effects.
The negative inotropic effect of R-PIA seems to be potentiated in PP2A-TG, leading to the assumption that PP2A, at least in part, is involved in adenosine receptor signaling.
In CHO cells, it has been demonstrated that PP2A is involved in M3 receptor signaling. Via SET, an inhibitory subunit of PP2A, the M3 receptor dephosphorylation was decreased followed by a decreased G protein coupling (Simon et al. 2012). From these data, it could be concluded that a decreased activity of PP2A contributes to the inhibition of M3 receptor calcium signaling (Simon et al. 2012). In reverse, it could be assumed that an increased PP2A activity may positively contribute to M3 receptor signaling. Here, the missing effects of PP2A overexpression on the apparently M3 receptor–mediated positive inotropic effects led to the assumption that the PP2A is either not involved or the overexpressed catalytic subunit is not correctly targeted in PP2A-TG or the M3 receptor signaling in CHO cells is completely different compared to cardiomyocytes. On the other hand, if the M3 receptor is only located in the endocardial endothelium, as suspected by the authors, and the effects of the M3 receptor are mediated indirectly through the release of prostaglandins (Hara et al. 2009), the overexpressed PP2A may be ineffective because in our transgenic model, overexpression is restricted to the cardiomyocytes and does not occur in cardiac endothelial cells (Gergs et al. 2004).
Our current study has several limitations: firstly, in this work, we have not generated biochemical data like the phosphorylation level of regulatory proteins in the context of muscarinic receptor stimulation. In a future repetition of the experiments, it would be necessary to freeze clamp the sample time matched at the maximum negative inotropic effect as well as at the maximum positive inotropic effect. Secondly, we do not know exactly how the overexpressed catalytic subunit of PP2A is targeted in the transgenic mice because of missing data concerning the regulatory PP2A subunits also if the expression of important regulatory subunits seems to be unchanged in PP2A-TG compared to WT (Gergs et al. 2004). Thirdly, experiments with selective receptor antagonists to verify the involved receptor subtype are currently missing also because the development of subtype-selective small molecules has been challenging (Pham et al. 2023). However, experiments with supposedly M1 or M3 receptor–selective antagonists (Heijman et al. 2018; Liu et al. 2018) should be performed in a follow-up project. Moreover, the study is restricted to only one experimental method (measurement of the force of contraction of atrial preparations) and, therefore, a complementary method like isolated cardiomyocytes would be interesting to study in a follow-up project. Finally, other protein phosphatases like PP2B should be taken into account (Honkanen 1993).
In summary, we nonetheless speculate that protein phosphatases, perhaps different from PP1 or PP2A, are involved in the muscarinic receptor signaling. Therefore, further investigations should be carried out on this issue. Indeed, we have started to establish a transgenic model with overexpression of the PP2A inhibitor SET that may be helpful in future studies, but this is beyond the scope of the present work.
Data availability
The data of this study are available from the corresponding author upon reasonable request.
References
Bognar IT, Beinhauer B, Kann P, Fuder H (1990) Different muscarinic receptors mediate autoinhibition of acetylcholine release and vagally-induced vasoconstriction in the rat isolated perfused heart. Naunyn Schmiedebergs Arch Pharmacol 341:279–287. https://doi.org/10.1007/BF00180652
Boknik P, Grote-Wessels S, Barteska G, Jiang M, Müller FU, Schmitz W, Neumann J, Birnbaumer L (2009) Genetic disruption of G proteins, G(i2)alpha or G(o)alpha, does not abolish inotropic and chronotropic effects of stimulating muscarinic cholinoceptors in atrium. Br J Pharmacol 158:1557–1564. https://doi.org/10.1111/j.1476-5381.2009.00441.x
Brodde OE, Michel MC (1999) Adrenergic and muscarinic receptors in the human heart. Pharmacol Rev 51:651–690
Brüchert N, Mavila N, Boknik P, Baba HA, Fabritz L, Gergs U, Kirchhefer U, Kirchhof P, Matus M, Schmitz W, Depaoli-Roach AA, Neumann J (2008) Inhibitor-2 prevents protein phosphatase 1-induced cardiac hypertrophy and mortality. Am J Physiol Heart Circ Physiol 295:H1539–H1546. https://doi.org/10.1152/ajpheart.00515.2008
Cheng G, Takahashi M, Shunmugavel A, Wallenborn JG, Depaoli-Roach AA, Gergs U, Neumann J, Kuppuswamy D, Menick DR, Cooper G (2010) Basis for MAP4 dephosphorylation-related microtubule network densification in pressure overload cardiac hypertrophy. J Biol Chem 285:38125–38140. https://doi.org/10.1074/jbc.M110.148650
Chu L, Norota I, Ishii K, Endoh M (2003) Inhibitory action of the phosphatase inhibitor cantharidin on the endothelin-1-induced and the carbachol-induced negative inotropic effect in the canine ventricular myocardium. J Cardiovasc Pharmacol 41(Suppl 1):S89-92
Dawson TA, Li D, Woodward T, Barber Z, Wang L, Paterson DJ (2008) Cardiac cholinergic NO-cGMP signaling following acute myocardial infarction and nNOS gene transfer. Am J Physiol Heart Circ Physiol 295:H990–H998. https://doi.org/10.1152/ajpheart.00492.2008
de Vente J (2004) cGMP: a second messenger for acetylcholine in the brain? Neurochem Int 45:799–812. https://doi.org/10.1016/j.neuint.2004.03.010
Dhein S, van Koppen CJ, Brodde OE (2001) Muscarinic receptors in the mammalian heart. Pharmacol Res 44:161–182. https://doi.org/10.1006/phrs.2001.0835
Dörner M-F, Boknik P, Köpp F, Buchwalow IB, Neumann J, Gergs U (2021) Mechanisms of systolic cardiac dysfunction in PP2A, PP5 and PP2AxPP5 double transgenic mice. Int J Mol Sci 22. https://doi.org/10.3390/ijms22179448
Drube J, Haider RS, Matthees ESF, Reichel M, Zeiner J, Fritzwanker S, Ziegler C, Barz S, Klement L, Filor J, Weitzel V, Kliewer A, Miess-Tanneberg E, Kostenis E, Schulz S, Hoffmann C (2022) GPCR kinase knockout cells reveal the impact of individual GRKs on arrestin binding and GPCR regulation. Nat Commun 13:540. https://doi.org/10.1038/s41467-022-28152-8
Du XY, Schoemaker RG, Bos E, Saxena PR (1995) Characterization of the positive and negative inotropic effects of acetylcholine in the human myocardium. Eur J Pharmacol 284:119–127. https://doi.org/10.1016/0014-2999(95)00384-w
Froldi G, Pandolfo L, Chinellato A, Ragazzi E, Caparrotta L, Fassina G (1994) Dual effect of ATP and UTP on rat atria: which types of receptors are involved? Naunyn Schmiedebergs Arch Pharmacol 349:381–386. https://doi.org/10.1007/BF00170884
Gergs U, Boknik P, Buchwalow I, Fabritz L, Matus M, Justus I, Hanske G, Schmitz W, Neumann J (2004) Overexpression of the catalytic subunit of protein phosphatase 2A impairs cardiac function. J Biol Chem 279:40827–40834. https://doi.org/10.1074/jbc.M405770200
Gergs U, Boknik P, Schmitz W, Simm A, Silber R-E, Neumann J (2008) A positive inotropic effect of ATP in the human cardiac atrium. Am J Physiol Heart Circ Physiol 294:H1716–H1723. https://doi.org/10.1152/ajpheart.00945.2007
Gergs U, Böckler A, Ebelt H, Hauptmann S, Keller N, Otto V, Pönicke K, Schmitz W, Neumann J (2013) Human 5-HT4receptor stimulation in atria of transgenic mice. Naunyn Schmiedebergs Arch Pharmacol 386:357–367. https://doi.org/10.1007/s00210-013-0831-x
Gergs U, Fahrion CM, Bock P, Fischer M, Wache H, Hauptmann S, Schmitz W, Neumann J (2017) Evidence for a functional role of calsequestrin 2 in mouse atrium. Acta Physiol (Oxf) 219:669–682. https://doi.org/10.1111/apha.12766
Gergs U, Trapp T, Bushnaq H, Simm A, Silber R-E, Neumann J (2019a) Age-dependent protein expression of serine/threonine phosphatases and their inhibitors in the human cardiac atrium. Adv Med 2019:2675972. https://doi.org/10.1155/2019/2675972
Gergs U, Bernhardt G, Buchwalow IB, Edler H, Fröba J, Keller M, Kirchhefer U, Köhler F, Mißlinger N, Wache H, Neumann J (2019b) Initial characterization of transgenic mice overexpressing human histamine H2 receptors. J Pharmacol Exp Ther 369:129–141. https://doi.org/10.1124/jpet.118.255711
Gergs U, Weisgut J, Griethe K, Mißlinger N, Kirchhefer U, Neumann J (2021) Human histamine H2 receptors can initiate cardiac arrhythmias in a transgenic mouse. Naunyn Schmiedebergs Arch Pharmacol 394:1963–1973. https://doi.org/10.1007/s00210-021-02098-y
Gergs U, Jahn T, Schulz N, Großmann C, Rueckschloss U, Demus U, Buchwalow IB, Neumann J (2022) Protein phosphatase 2A improves cardiac functional response to ischemia and sepsis. Int J Mol Sci 23. https://doi.org/10.3390/ijms23094688
Grote-Wessels S, Baba HA, Boknik P, El-Armouche A, Fabritz L, Gillmann H-J, Kucerova D, Matus M, Müller FU, Neumann J, Schmitz M, Stümpel F, Theilmeier G, Wohlschlaeger J, Schmitz W, Kirchhefer U (2008) Inhibition of protein phosphatase 1 by inhibitor-2 exacerbates progression of cardiac failure in a model with pressure overload. Cardiovasc Res 79:464–471. https://doi.org/10.1093/cvr/cvn113
Gupta RC, Neumann J, Boknik P, Watanabe AM (1994) M2-specific muscarinic cholinergic receptor-mediated inhibition of cardiac regulatory protein phosphorylation. Am J Physiol 266:H1138–H1144. https://doi.org/10.1152/ajpheart.1994.266.3.H1138
Hara Y, Ike A, Tanida R, Okada M, Yamawaki H (2009) Involvement of cyclooxygenase-2 in carbachol-induced positive inotropic response in mouse isolated left atrium. J Pharmacol Exp Ther 331:808–815. https://doi.org/10.1124/jpet.109.156992
Harvey RD, Belevych AE (2003) Muscarinic regulation of cardiac ion channels. Br J Pharmacol 139:1074–1084. https://doi.org/10.1038/sj.bjp.0705338
Heijman J, Dewenter M, El-Armouche A, Dobrev D (2013) Function and regulation of serine/threonine phosphatases in the healthy and diseased heart. J Mol Cell Cardiol 64:90–98. https://doi.org/10.1016/j.yjmcc.2013.09.006
Heijman J, Ghezelbash S, Wehrens XHT, Dobrev D (2017) Serine/threonine phosphatases in atrial fibrillation. J Mol Cell Cardiol 103:110–120. https://doi.org/10.1016/j.yjmcc.2016.12.009
Heijman J, Kirchner D, Kunze F, Chrétien EM, Michel-Reher MB, Voigt N, Knaut M, Michel MC, Ravens U, Dobrev D (2018) Muscarinic type-1 receptors contribute to IK, ACh in human atrial cardiomyocytes and are upregulated in patients with chronic atrial fibrillation. Int J Cardiol 255:61–68. https://doi.org/10.1016/j.ijcard.2017.12.050
Hellgren I, Mustafa A, Riazi M, Suliman I, Sylvén C, Adem A (2000) Muscarinic M3 receptor subtype gene expression in the human heart. Cell Mol Life Sci 57:175–180. https://doi.org/10.1007/s000180050507
Herzig S, Neumann J (2000) Effects of serine/threonine protein phosphatases on ion channels in excitable membranes. Physiol Rev 80:173–210. https://doi.org/10.1152/physrev.2000.80.1.173
Ho H-T, Belevych AE, Liu B, Bonilla IM, Radwański PB, Kubasov IV, Valdivia HH, Schober K, Carnes CA, Györke S (2016) Muscarinic stimulation facilitates sarcoplasmic reticulum Ca release by modulating ryanodine receptor 2 phosphorylation through protein kinase G and Ca/calmodulin-dependent protein kinase II. Hypertension 68:1171–1178. https://doi.org/10.1161/HYPERTENSIONAHA.116.07666
Hoehn M, Zhang Y, Xu J, Gergs U, Boknik P, Werdan K, Neumann J, Ebelt H (2015) Overexpression of protein phosphatase 2A in a murine model of chronic myocardial infarction leads to increased adverse remodeling but restores the regulation of β-catenin by glycogen synthase kinase 3β. Int J Cardiol 183:39–46. https://doi.org/10.1016/j.ijcard.2015.01.087
Honkanen RE (1993) Cantharidin, another natural toxin that inhibits the activity of serine/threonine protein phosphatases types 1 and 2A. FEBS Lett 330:283–286. https://doi.org/10.1016/0014-5793(93)80889-3
Kirchhefer U, Baba HA, Bokník P, Breeden KM, Mavila N, Brüchert N, Justus I, Matus M, Schmitz W, Depaoli-Roach AA, Neumann J (2005) Enhanced cardiac function in mice overexpressing protein phosphatase inhibitor-2. Cardiovasc Res 68:98–108. https://doi.org/10.1016/j.cardiores.2005.05.019
Kitazawa T, Asakawa K, Nakamura T, Teraoka H, Unno T, Komori S-I, Yamada M, Wess J (2009) M3 muscarinic receptors mediate positive inotropic responses in mouse atria: a study with muscarinic receptor knockout mice. J Pharmacol Exp Ther 330:487–493. https://doi.org/10.1124/jpet.109.153304
Krause T, Grote-Wessels S, Balzer F, Boknik P, Gergs U, Kirchhefer U, Buchwalow IB, Müller FU, Schmitz W, Neumann J (2018) Successful overexpression of wild-type inhibitor-2 of PP1 in cardiovascular cells. Naunyn Schmiedebergs Arch Pharmacol 391:859–873. https://doi.org/10.1007/s00210-018-1515-3
Lang N, Reppel M, Hescheler J, Fleischmann BK (2007) NO underlies the muscarinic receptor-mediated inhibition of If in early embryonic heart cells. Cell Physiol Biochem 20:293–302. https://doi.org/10.1159/000107515
Li L, Homan KT, Vishnivetskiy SA, Manglik A, Tesmer JJG, Gurevich VV, Gurevich EV (2015) G protein-coupled receptor kinases of the GRK4 protein subfamily phosphorylate inactive G protein-coupled receptors (GPCRs). J Biol Chem 290:10775–10790. https://doi.org/10.1074/jbc.M115.644773
Liu H, Hofmann J, Fish I, Schaake B, Eitel K, Bartuschat A, Kaindl J, Rampp H, Banerjee A, Hübner H, Clark MJ, Vincent SG, Fisher JT, Heinrich MR, Hirata K, Liu X, Sunahara RK, Shoichet BK, Kobilka BK, Gmeiner P (2018) Structure-guided development of selective M3 muscarinic acetylcholine receptor antagonists. Proc Natl Acad Sci U S A 115:12046–12050. https://doi.org/10.1073/pnas.1813988115
Lyashkov AE, Vinogradova TM, Zahanich I, Li Y, Younes A, Nuss HB, Spurgeon HA, Maltsev VA, Lakatta EG (2009) Cholinergic receptor signaling modulates spontaneous firing of sinoatrial nodal cells via integrated effects on PKA-dependent Ca(2+) cycling and I(KACh). Am J Physiol Heart Circ Physiol 297:H949–H959. https://doi.org/10.1152/ajpheart.01340.2008
Lymperopoulos A, Cora N, Maning J, Brill AR, Sizova A (2021) Signaling and function of cardiac autonomic nervous system receptors: insights from the GPCR signalling universe. FEBS J 288:2645–2659. https://doi.org/10.1111/febs.15771
National Academies Press (US) (2011) Guide for the Care and Use of Laboratory Animals. 8th edn. Washington, DC
Neumann J, Scholz H (1998) Deferoxamine blocks interactions of fluoride and carbachol in isolated mammalian cardiac preparations. Eur J Pharmacol 350:189–194. https://doi.org/10.1016/s0014-2999(98)00235-0
Neumann J, Kaspareit G, Kirchhefer U, Scholz H (1995) Sodium fluoride attenuates the negative inotropic effects of muscarinic M2 and adenosine receptor agonists. Eur J Pharmacol 294:451–457. https://doi.org/10.1016/0014-2999(95)00569-2
Neumann J, Vahlensieck U, Boknik P, Linck B, Lüss H, Müller FU, Matherne GP, Schmitz W (1999) Functional studies in atrium overexpressing A1-adenosine receptors. Br J Pharmacol 128:1623–1629. https://doi.org/10.1038/sj.bjp.0702963
Neumann J, Boknik P, Matherne GP, Lankford A, Schmitz W (2003) Pertussis toxin sensitive and insensitive effects of adenosine and carbachol in murine atria overexpressing A(1)-adenosine receptors. Br J Pharmacol 138:209–217. https://doi.org/10.1038/sj.bjp.0705012
Neumann J, Boknik P, Kirchhefer U, Gergs U (2021) The role of PP5 and PP2C in cardiac health and disease. Cell Signal 85:110035. https://doi.org/10.1016/j.cellsig.2021.110035
Oberhauser V, Schwertfeger E, Rutz T, Beyersdorf F, Rump LC (2001) Acetylcholine release in human heart atrium: influence of muscarinic autoreceptors, diabetes, and age. Circulation 103:1638–1643. https://doi.org/10.1161/01.cir.103.12.1638
Osipov AV, Averin AS, Shaykhutdinova ER, Dyachenko IA, Tsetlin VI, Utkin YN (2023) Muscarinic and nicotinic acetylcholine receptors in the regulation of the cardiovascular system. Russ J Bioorg Chem 49:1–18. https://doi.org/10.1134/S1068162023010211
Pham V, Habben Jansen MCC, Thompson G, Heitman LH, Christopoulos A, Thal DM, Valant C (2023) Role of conserved tyrosine lid residues in the activation of the M2 muscarinic acetylcholine receptor. Mol Pharmacol 104:92–104. https://doi.org/10.1124/molpharm.122.000661
Pönicke K, Heinroth-Hoffmann I, Brodde O-E (2003) Demonstration of functional M3-muscarinic receptors in ventricular cardiomyocytes of adult rats. Br J Pharmacol 138:156–160. https://doi.org/10.1038/sj.bjp.0704997
Saw EL, Kakinuma Y, Fronius M, Katare R (2018) The non-neuronal cholinergic system in the heart: a comprehensive review. J Mol Cell Cardiol 125:129–139. https://doi.org/10.1016/j.yjmcc.2018.10.013
Simon V, Oner SS, Cohen-Tannoudji J, Tobin AB, Lanier SM (2012) Influence of the accessory protein SET on M3 muscarinic receptor phosphorylation and G protein coupling. Mol Pharmacol 82:17–26. https://doi.org/10.1124/mol.111.075523
Wijnker PJM, Boknik P, Gergs U, Müller FU, Neumann J, dos Remedios C, Schmitz W, Sindermann JR, Stienen GJM, van der Velden J, Kirchhefer U (2011) Protein phosphatase 2A affects myofilament contractility in non-failing but not in failing human myocardium. J Muscle Res Cell Motil 32:221–233. https://doi.org/10.1007/s10974-011-9261-x
Yatani A, Okabe K, Codina J, Birnbaumer L, Brown AM (1990) Heart rate regulation by G proteins acting on the cardiac pacemaker channel. Science 249:1163–1166. https://doi.org/10.1126/science.1697697
Acknowledgements
This work contains parts of the MD thesis of Tobias Fuhrmann, Silke Wackerhagen, and Inka Schäfer. The technical assistance of S. Reber and P. Willmy is greatly appreciated.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conceptualization, J.N. and U.G.; methodology, T.F., S.W. and I.S.; formal analysis, T.F., S.W., I.S. and U.G.; project administration, J.N.; resources, J.N.; writing - original draft preparation, U.G.; writing - review and editing, U.G. and J.N.; All authors read and approved the final manuscript. The authors declare that all data were generated in-house and that no paper mill was used.
Corresponding author
Ethics declarations
Ethics approval
The investigation conformed to the Guide for the Care and Use of Laboratory Animals as published by the National Research Council (2011). The animals were handled and maintained according to the approved protocols of the Animal Welfare Committee of the University of Halle-Wittenberg, Halle, Germany.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gergs, U., Wackerhagen, S., Fuhrmann, T. et al. Further investigations on the influence of protein phosphatases on the signaling of muscarinic receptors in the atria of mouse hearts. Naunyn-Schmiedeberg's Arch Pharmacol 397, 5731–5743 (2024). https://doi.org/10.1007/s00210-024-02973-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-024-02973-4