Abstract
Summary
The novel metaPGS, integrating multiple fracture–related genetic traits, surpasses traditional polygenic scores in predicting fracture risk. Demonstrating a robust association with incident fractures, this metaPGS offers significant potential for enhancing clinical fracture risk assessment and tailoring prevention strategies.
Introduction
Current polygenic scores (PGS) have limited predictive power for fracture risk. To improve genetic prediction, we developed and evaluated a novel metaPGS combining genetic information from multiple fracture–related traits.
Methods
We derived individual PGS from genome-wide association studies of 16 fracture-related traits and employed an elastic-net logistic regression model to examine the association between the 16 PGSs and fractures. An optimal metaPGS was constructed by combining 11 significant individual PGSs selected by the elastic regularized regression model. We evaluated the predictive power of the metaPGS alone and in combination with clinical risk factors recommended by guidelines. The discrimination ability of metaPGS was assessed using the concordance index. Reclassification was assessed using net reclassification improvement (NRI) and integrated discrimination improvement (IDI).
Results
The metaPGS had a significant association with incident fractures (HR 1.21, 95% CI 1.18–1.25 per standard deviation of metaPGS), which was stronger than previously developed bone mineral density (BMD)-related individual PGSs. Models with PGS_FNBMD, PGS_TBBMD, and metaPGS had slightly higher but statistically non-significant c-index than the base model (0.640, 0.644, 0.644 vs. 0.638). However, the reclassification analysis showed that compared to the base model, the model with metaPGS improves the reclassification of fracture.
Conclusions
The metaPGS is a promising approach for stratifying fracture risk in the European population, improving fracture risk prediction by combining genetic information from multiple fracture–related traits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a bone disease that develops when bone mineral density (BMD) and bone mass decrease or when the structure and strength of bone change. This can increase susceptibility to fractures, especially in the hip, spine, and wrist [1]. Osteoporotic fractures can lead to significant morbidity, mortality, and healthcare expenses [2], with an estimated 2 million cases and $19 billion in costs annually in the United States alone [3, 4]. Given the global aging population, the incidence of osteoporosis is projected to increase [5], underscoring the importance of early identification of individuals at high risk of primary fractures.
The risk of osteoporotic fracture has a high heritability, with genetic liability up to 46% [6]. Genetic factors substantially contribute to fracture risk [7]. Genome-wide association studies (GWAS) over the past decade have identified single nucleotide polymorphisms (SNPs) associated with bone strength-related traits [7]. Around 43 genomic loci and thousands of SNPs are robustly associated with fractures [8], and many more genetic associations have been reported for fracture-related traits/risk factors [9,10,11].
Bone mineral density (BMD) is the most critical predictor of osteoporosis and fracture [12]. Polygenic score (PGS) derived from GWAS summary statistics for BMD has been used to quantify an individual’s genetic liability to fractures [13,14,15,16,17]. Previous studies have highlighted the potential of BMD-related PGS for risk prediction of fracture [13, 14]. Nevertheless, the clinical utility of PGS in fracture prediction is limited, with a marginal additive effect of PGS on clinical factors.
A multi-PGS extension, metaPGS, has been developed to improve predictive performance by combining multiple PGSs into one score [18]. It has been applied to many other complex diseases and was proven to significantly increase the predictive accuracy of coronary artery disease [18], ischemic stroke [19], type 2 diabetes [20], and breast cancer [21]. In fracture prediction, an individual’s estimated genetic propensity was typically derived based on the GWAS summary statistics of a single trait, BMD. Considering that fragility fracture is a multifactorial disease influenced by various physiological factors beyond BMD [22], PGS depending on only one trait may not be sufficient to capture the genetic components of fracture. If a particular disease/trait is causally involved in the etiology of fracture, the PGS for that disease/trait as a genetic proxy should predict fracture occurrence, and a metaPGS may be particularly useful in fracture prediction. Integrating genetic information of multiple fracture–related traits into metaPGS can improve predictive accuracy.
Therefore, this study aimed to develop and validate a multi-trait metaPGS to integrate genetic information of multiple fracture–related traits to improve predictive accuracy. To evaluate the predictive value of metaPGS beyond the currently available fracture prediction tool, we examined the potential clinical use of metaPGS beyond the existing fracture risk assessment tool (FRAX), an algorithm predicting 10-year probabilities of major osteoporotic fracture (MOF) and hip fracture (HF) based on 12 clinical risk factors [23]. By improving the accuracy of genetic risk prediction for osteoporotic fractures, metaPGS could aid in identifying high-risk individuals and implementing preventive measures.
Methods
Study cohort
The UK Biobank (UKB) is a large-scale population-based observational study comprising 502,617 individuals aged between 40 and 69 years who were recruited from the UK between 2006 and 2010 [24]. A standardized socio-demographic questionnaire, medical history, and other lifestyle factors were collected at recruitment. Individual records were linked to the Hospital Episode Statistics (HES) records and the national death and cancer registries as the underlying genetic models were developed and trained primarily using European ancestry samples, including individuals of white British ancestry in the current study, allowed for a better representation of the genetic architecture in that population, and resulted in more accurate predictions. Thus, the current study only included individuals of white British ancestry to examine a relatively homogeneous group.
Fracture events ascertaining
Fracture cases were identified using the baseline questionnaire of self-reported fracture incidents fractures within the past 5 years. Hospital Episode Statistics are linked through NHS Digital with a hospital-based fracture diagnosis irrespective of mechanism within the primary or secondary diagnosis field (Supplementary Table 1). All the incident fracture cases were identified through the hospital episode statistics. Fractures of the skull, face, hands, and feet, pathological fractures due to malignancy, atypical femoral fractures, and periprosthetic and healed fractures were excluded from the analysis. Based on the date of the ICD-10 record, fractures sustained after the initial assessment visit were defined as incident cases (n = 13,623).
Data processing and quality control
A total of 488,251 participants were genotyped using Affymetrix arrays [25]. The genotype data were quality controlled and additionally imputed using the Haplotype Reference Consortium (HRC) [26] and the UK10K haplotype resources, yielding a total of 96 million imputed variants. SNPs with minor allele frequency less than 0.1% and SNPs that are missing in a high fraction of subjects (> 0.01), Hardy–Weinberg equilibrium p value > 1 × \({10}^{-6}\). Individuals with a high rate of genotype missingness (> 0.01) were excluded from PGS construction. A total of 450,395 individuals and 11.5 million variants passed the quality control standards and remained for subsequent analysis.
Individual PGS tuning
GWAS summary statistics were available for 16 complex traits/diseases related to fracture risk. PGSs were generated with the estimated effect sizes from the most recent literature on large GWAS (Supplementary Table 2). To minimize the risk of over-fitting due to overlapping samples between the GWAS discovery set and the UKB validation set, the selected GWAS did not include UKB samples. GWASs for femoral neck BMD [27], total body BMD [28], hand grip strength (HGS) [9], appendicular lean mass (ALM) [10], whole body lean mass (WBLM) [10], vitamin D (VD) [11], serum calcium concentration (SCC) [29], homocysteine (HC) [30], thyroid stimulating hormone level (TSH) [31], fasting glucose (FG) [32], fasting insulin (FI) [32], type 1 diabetes (T1D) [33], type 2 diabetes (T2D) [34], rheumatoid arthritis (RA) [35], inflammatory bowel disease (IBD) [36], hip bone size (HBS) [37], and coronary artery disease (CAD) [38] were selected for individual PGS derivation.
We randomly selected 1000 fracture cases and 2000 non-fracture cases for individual PGS tuning. Based on GWAS summary statistics of 16 fracture-related phenotypes and a linkage disequilibrium reference panel of 503 European samples from 1000 Genomes (phase 3, version 5), a set of candidate PGSs was derived for each phenotype/trait using the Pruning and Thresholding (P + T) method and the LDPred2 computational algorithm [39].
Using the P + T method, 24 candidate PGSs were calculated with combinations of p value (1.0, 0.5, 0.05, 5 × 10−4, 5 × 10−6, and 5 × 10−8) and \({r}^{2}\) (0.2, 0.4, 0.6, and 0.8) thresholds for each trait. The LDPred2 computational algorithm grid mode was used to generate seven candidate PGSs based on seven hyper-parameter values of ρ (1, 0.3, 0.1, 0.03, 0.01, 0.003, and 0.001). The PGS construction was restricted to the HapMap3 variants only, as LDpred2 suggested [29].
For each of the 16 phenotypes, 31 candidate PGS were derived for each individual in the UKB tuning set. The risk of fractures increases with age due to the weakening of bones. Women are at higher risk for osteoporosis-related fractures than men; the association between each PGS and the fracture was further evaluated in terms of odds ratios (OR) per standard deviation of PGS using logistic regression adjusted for age, sex, and BiLEVE/UKB genotyping array and the first four principal components (PCs). The most optimal model for the largest magnitude odds ratio was selected as the one representative PGS for each trait and carried forward into subsequent analyses.
Derivation of the metaPGS
Each representative PGS determined from the previous step was standardized to have a zero mean and unit standard deviation. We then split the remaining UKB European ancestry dataset into a training set (n = 135, 119) and a testing set (n = 315,276). Using the UKB training set, we employed elastic-net logistic regression [40] to model the association between the 16 PGSs and fracture, adjusting for age, sex, and the first four PCs. A range of models with different penalties was evaluated using tenfold cross-validation. Regarding the highest area under the receiving-operating characteristic curve (AUC), the best model was selected as the final model to generate metaPGS and held fixed for validation in the UKB testing set. The metaPGS was calculated using a weighted average of the standardized individual PGSs:
where \({{\text{PGS}}}_{{\text{i}}1}\),…,\({{\text{PGS}}}_{{\text{i}}16}\) are the 16 zero mean and unit variance standardized PGSs for the \(i\) th individual; \({\alpha }_{1}\),…,\({\alpha }_{19}\) are the coefficients (log odds ratio) for each of the 16 PGSs (Fig. 1).
Study design and workflow. a Derivation of individual PRSs in the UKB training set (n = 135,119) using GWAS summary statistics for individual traits. b The metaPGS for fracture was then derived by integrating individual PGSs using the elastic-net cross-validation. c Validation of the metaPGS for fracture will be performed in the UKB validation set (n = 315,276). PGS, polygenic score; FNBMD, femoral neck bone mineral density; TBBMD, total body bone mineral density; HGS, hand grip strength; ALM, appendicular lean mass; WBLM, whole body lean mass; VD, vitamin D; SCC, serum calcium concentration; HC, homocysteine; TSH, thyroid stimulating hormone level; FG, fasting glucose; FI, fasting insulin; T1D, type 1 diabetes; T2D, type 2 diabetes; RA, rheumatoid arthritis; IBD, inflammatory bowel disease; HBS, hip bone size; CAD, coronary artery disease
Statistical analyses
The demographic and clinical characteristics of the UKB testing set were described using mean and standard deviation (SD) for continuous variables and the frequency and percent for categorical variables. The primary outcome of this study was incident fractures. All PGSs in the UKB testing set were standardized to facilitate interpretability to have unit variance. To illustrate the different cumulative incidences of fracture in individuals with distinct genetic predispositions, we grouped individuals according to different quantile ranges of metaPGS: ≤ 1%, 1–5%, 5–20%, 20–40%, 40–60%, 60–80%, 80–95%, 95–99%, and > 99%. The cumulative incidence of fracture by metaPGS groups was then derived using the cumulative incidence function (CIF), with the competing mortality risk accounted for.
The separate prediction of each of the 16 trait-specific PGSs was examined by fitting a series of simple logistic regression models. To account for multiple testing across the individual PGSs tested in separate logistic regression models (single-PGS models), we used 10,000 permutations to find the significance threshold to control the false discovery rate p values. Using the UKB training set, we employed elastic-net logistic regression [40] to model the association between the 16 PGSs and fracture, adjusting for age, sex, and the first four PCs. Based on significant individual PGSs selected from the elastic regularized regression model, metaPGS was derived for each individual in the UKB testing set. Two previously developed BMD-related PGSs (PGS_FNBMD [13] and PGS_TBBMD [16]) were also included in the subsequent analysis for comparison purposes.
All scores (PGS_FNBMD, PGS_TBBMD, and metaPGS) were evaluated using logistic regression and Cox proportional hazard regression. The performance of models with and without PGSs in identifying individuals at risk of sustaining a fracture was evaluated using the AUC and tested for statistical significance using the Delong test. Additionally, we examined the fracture incidence according to the PGS category in the UKB testing set. We compared the effect of top percentiles (1%, 5%, 10%, and 20%) with the remaining percentiles (99%, 95%, 90%, and 80%) of each PGS using Cox proportional hazard models. All regression models were controlled for age, sex, and the first four PCs.
We also investigated the predictive value of metaPGS beyond the existing fracture assessment tool and compared its performance with two previously developed BMD-related PGSs (PGS_FNBMD [13] and PGS_TBBMD [16]). The association between each PGS with fracture risk, adjusted for the FRAX risk factors, including age, BMI, previous fracture, current smoking, glucocorticoids, and rheumatoid arthritis, was assessed using Cox proportional hazard models. The model with only FRAX risk factors was set as the base model. Four models were formulated: (1) Model 1—base model; (2) Model 2—base model + \(PGS\_FNBMD\); (3) Model 3—base model + \(PGS\_TBBMD\); and (4) Model 4—base model + \(metaPGS\). The magnitude of the association between each PGS and fracture risk was assessed by the hazard ratio and its corresponding 95% confidence intervals. Model comparison was performed using the bootstraps.
In addition, net reclassification improvement (NRI) was adopted to compare the reclassification ability of the models with PGSs to those without PGS. We designated “high risk” as the predicted MOF risk ≥ 20% and “low risk” as the predicted MOF risk < 20%, based on the National Osteoporosis Foundation’s recommended fixed intervention cutoff [41]. The integrated discrimination improvement (IDI) was also calculated to incorporate both the direction of change in the calculated risk and the extent of change.
The estimated BMD (eBMD) calculated based on the quantitative ultrasound index through the calcaneus is available for the majority of the subjects in the UKB. Given that eBMD is recognized as a predictor of fracture risk, we sought to enhance our analysis by conducting a sensitivity analysis. This additional investigation aimed to provide a more comprehensive understanding of the impact of PGSs in a model that incorporates both FRAX risk factors and eBMD. Furthermore, we extended our sensitivity analysis to evaluate the predictive ability of the developed metaPGS in the context of non-vertebral fractures. All statistical analyses were conducted using R version 4.0.3 software and SAS 9.4 (SAS Institute, Inc., Cary, NC, USA).
Results
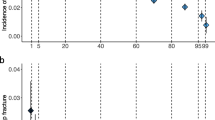
The characteristics of the UKB testing set are shown in Supplementary Table 3. The overall UKB testing set consists of 315,276 individuals, of which 8787 were incident fracture cases and 306,489 were non-fracture cases. Supplementary Fig. 1 shows correlations between 16 individual PGSs, with strong correlations observed between HC and SCC, SCC and CAD, CAD and IBD, ALM and WBLM, T1D and TSH, TSH and TBBMD, TBBMD, and RA. The metaPGS was derived based on 11 significant individual PGSs selected from the elastic regularized regression model (model weights are shown in Fig. 2).
Associations of 16 trait-specific PGSs with the fracture outcome in the UKB derivation set. Estimates per standard deviation increase of each individual PRS evaluated in logistic regression (univariate) and elastic-net logistic regression adjusted for age and sex. “inactive” indicates that the elastic-net estimated odds ratio was negligible (between 0.999 and 1.001, shown as a blue dot). CI, confidence interval
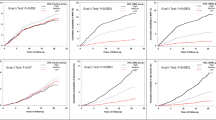
We assessed the crude 10-year cumulative fracture incidence by nine PGS groups (Fig. 3). With competing mortality risk accounted for, significant differences in the 10-year fracture risk were observed across metaPGS deciles (p < 0.0001). The top and bottom 1% of the metaPGS showed a substantial difference in the cumulative fracture incidence. A comparison of the metaPGS with its individual components (PGS_FNBMD and PGS_TBBMD) is shown in Fig. 4. Results show that metaPGS had a greater association with fracture risk than the two individual PGSs. All three PGSs were strongly associated with incident fracture (p < 0.0001), with an odds ratio (OR) ranging from 1.15 to 1.35. In comparison to the baseline model, which incorporated only age and sex, models augmented with PGS_FNBMD, PGS_TBBMD, and metaPGS demonstrated marginal improvements in the AUC from 0.643 to 0.647, 0.654, and 0.654, respectively. However, these improvements were not deemed statistically significant. The metaPGS was associated with an incident fracture with a hazard ratio (HR) of 1.22 (95% CI 1.19–1.27) per standard deviation of metaPGS, which was stronger than PGS_FNBMD (HR = 1.10, 95% CI 1.08–1.12) and PGS_TBBMD (HR = 1.15, 95% CI 1.12–1.18) (Fig. 4). Using Cox proportional hazard models, we also assessed the HRs for the top 1%, 5%, 10%, and 20% decile vs. the remaining percentiles of the PGSs. The results showed that the bottom 1% of the population had a 1.36-fold (95% CI 1.15–1.61) increased fracture risk than the remaining population (Supplementary Table 4).
Relative performance of PGS_FNBMD, PGS_TBBMD, and metaPGS for fracture. A Cox proportional hazard models; B multivariate logistic regression models. Separated logistic/Cox proportional hazard regression was conducted for each PGS; each estimate was adjusted for age, sex, and the first four principal components
The clinical utility of a PGS depends on its performance in combination with established risk factors and genetic risk models. Next, we evaluated the predictive value of metaPGS while adjusting for established risk factors. We examined seven FRAX risk factors available in the UKB data. As expected, established risk factors were positively associated with incident fracture, current smoking, and sex being the strongest risk factors (Table 1). Adjusting for these risk factors only modestly attenuated the association of the metaPGS with incident fracture. The metaPGS had the strongest association with incident fracture. The HRs of PGS_FNBMD, PGS_TBBMD, and metaPGS for incident fracture were 1.09 (95% CI, 1.07–1.12), 1.15 (95% CI, 1.12–1.18), and 1.21 (95% CI, 1.18–1.25), respectively. Models with PGS_FNBMD, PGS_TBBMD, and metaPGS had slightly higher but statistically non-significant c-index than the base model (0.640, 0.644, 0.644 vs. 0.638) (Supplementary Table 5). Compared to the base model, the association between clinical risk factors and incident fracture risk did not attenuate in all four PGS models. The sensitivity analysis showed similar but attenuated results. The effect size of PGSs was attenuated in the sensitivity analysis but remained statistically significant. PGS_FNBMD (HR 1.06; 95% CI 1.03–1.09, p < 0.0001), PGS_TBBMD (HR 1.09; 95% CI 1.05–1.11, p < 0.0001), and metaPGS (HR 1.13, 95% CI 1.09–1.18, p < 0.0001) were significantly associated with an incident fracture, with FRAX risk factors and estimated BMD adjusted for (Supplementary Table 6). When further limited to non-vertebral incident fractures, the HR of PRS_FNBMD, PRS_TBBMD, and metaPGS were 1.05 (95% CI, 1.01–1.09), 1.08 (95% CI, 1.04–1.12), and 1.12 (95% CI, 1.06–1.16), respectively (Supplementary Table 7).
In the reclassification analysis, compared to the base model, the models with PGS_FNBMD, PGS_TBBMD, and metaPGS improved the reclassification of fracture by 0.9% (95% CI, 0.04 to 1.58%), 1.36% (95% CI, 0.52 to 2.19%), and 1.41% (95% CI, 0.58 to 2.24%), respectively (Table 2). Moreover, the metaPGS showed the most remarkable improvement in terms of reclassification. For the model that included metaPGS, 13,799 (6.9%) individuals were correctly reclassified up to the high-risk group, and 13,530 (4.3%) individuals who did not experience a fracture were correctly reclassified from the high-risk group to the low-risk group. The continuous NRI showed that improvement in fracture reclassification contributed by PGS_FNBMD, PGS_TBBMD, and metaPGS were 10.1%, 15.9%, and 16.8%, respectively.
Discussion
The present study developed and evaluated a novel metaPGS for fracture risk prediction by combining genetic information from multiple fracture–related traits. The ability of the metaPGS to predict fracture risk was evaluated alone and in combination with the clinical risk score recommended by guidelines. The metaPGS demonstrated a significant association with incident fractures, with a hazard ratio of 1.22 per standard deviation of metaPGS, which was significantly more potent than previously established BMD-related individual PGSs. The predictive power of the metaPGS was comparable to established risk factors such as age, body weight, and early menopause. Adding the metaPGS to the existing FRAX clinical risk factors improved the discrimination of fractures from non-fracture cases, suggesting that the metaPGS can help stratify fracture risk in the European population and develop personalized prevention strategies.
Our study contributes to using genomic information to stratify individuals for fracture risk. Pleiotropy, a phenomenon in which a single gene or genetic variant influences multiple traits or diseases, has been well-documented in previous research [42]. Since genetic variants can affect multiple traits simultaneously, independent PGSs for fracture risk are expected to overlap significantly. To overcome this challenge, we employed elastic net regularized regression to combine multiple PGSs and estimate their contributions to fracture risk prediction while minimizing collinearity. The resulting metaPGS combines genetic information from 11 of 16 bone-related traits and disorders, resulting in a robust and strongly associated predictor of fracture risk.
Compared to existing individual PGSs, the new metaPGS showed a more significant association with fracture and a more remarkable risk discrimination ability. Moreover, the metaPGS has comparable predictive power to some established risk factors. By combining metaPGS with the current fracture risk assessment tool, our findings suggested the added value of metaPGS beyond established clinical risk factors. The predictive ability of metaPGS was largely independent of established risk factors for fracture, implying that the metaPGS captured residual risk that was not quantified by the established risk factors. In addition, the results of reclassification analyses indicated that combining metaPGS with the FRAX risk factors improved discriminating fractures and non-fracture cases. Its fracture risk reclassification is better than the two previously developed BMD-related PGSs [43].
There are several limitations worth mentioning. Notably, the predictive performance of the metaPGS for fracture is limited when compared with certain diseases, such as CAD [18]. The reasons could be that fragility fracture is more heterogeneous than other diseases and that the GWAS sample size for mechanistically defined fracture is also limited. Also, our investigation focused on fractures reported by participants and the electronic health records, potentially leading to an underrepresentation of asymptomatic vertebral fractures. This limitation is noteworthy and likely plays a role in the comparatively lower predictive performance of the metaPGS for fractures. Furthermore, the sample size of older individuals (> 75 years) in the UKB is relatively small, limiting our ability to model fracture risk in the age strata where most events occur. Furthermore, the duration of follow-up in UKB is relatively limited. Because of the limited covariates available in the UKB, we could not assess the predictive value of the metaPGS beyond the full FRAX model. Moreover, as the metaPGS was derived and tested primarily in individuals of European ancestry, it may not have equivalent predictive power for other ethnic groups due to variations in allele frequencies, linkage disequilibrium patterns, and effect sizes of common polymorphisms across different ancestries. The absence of a family history of fracture in the UKB precluded an examination of whether the association of the metaPGS with fracture risk is influenced by familial factors. Finally, we only used a partial of the risk factors included in FRAX and did not calculate the FRAX estimate. Therefore, the effect of metaPGS beyond the FRAX may not be sufficiently adjusted.
Our study developed and evaluated a novel approach for fracture risk prediction, the metaPGS, which combines genetic information from multiple fracture–related traits. Despite challenges in phenotypic heterogeneity and GWAS power, our study presents a powerful fracture genomic risk score to date. It assesses its potential for risk stratification in the context of established risk factors and clinical guidelines. The metaPGS provides added value to established clinical risk factors and has potential clinical utility for personalized prevention strategies. However, it is imperative to acknowledge the possibility of cases falling outside the predictive scope of our model. Predictive models, including the metaPGS, inherently have limitations, and our findings suggest that not all fracture cases were accurately predicted. Future research endeavors could focus on incorporating additional variables, refining genetic markers, or exploring alternative methodologies to address these limitations. Future studies should also validate the metaPGS in other populations and evaluate its clinical utility. The metaPGS is a promising approach for fracture risk prediction that overcomes the limitations of single PGSs and represents a significant step towards using genomic information to help stratify individuals for fracture risk.
Data availability
Data sharing does not apply to this article as no datasets were generated during the current study.
References
Sözen T, Özışık L, Başaran NÇ (2017) An overview and management of osteoporosis. Eur J Rheumatol 4:46–56. https://doi.org/10.5152/eurjrheum.2016.048
Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN (2014) A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag 10:937–948. https://doi.org/10.2147/TCRM.S72456
Wright NC, Looker AC, Saag KG, Curtis JR, Delzell ES, Randall S, Dawson-Hughes B (2014) The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res 29:2520–2526. https://doi.org/10.1002/jbmr.2269
Singer A, Exuzides A, Spangler L, O’Malley C, Colby C, Johnston K, Agodoa I, Baker J, Kagan R (2015) Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc 90:53–62. https://doi.org/10.1016/j.mayocp.2014.09.011
Reginster JY, Burlet N (2006) Osteoporosis: a still increasing prevalence. Bone 38:4. https://doi.org/10.1016/j.bone.2005.11.024
Sigurdsson G, Halldorsson BV, Styrkarsdottir U, Kristjansson K, Stefansson K (2008) Impact of genetics on low bone mass in adults. J Bone Miner Res 23:1584–1590. https://doi.org/10.1359/jbmr.080507
Zhu X, Bai W, Zheng H (2021) Twelve years of GWAS discoveries for osteoporosis and related traits: advances, challenges and applications. Bone Research 9:23. https://doi.org/10.1038/s41413-021-00143-3
Nethander M, Movérare-Skrtic S, Kämpe A, Coward E, Reimann E, Grahnemo L, Borbély É, Helyes Z, Funck-Brentano T, Cohen-Solal M, Tuukkanen J, Koskela A, Wu J, Li L, Lu T, Gabrielsen ME, Estonian Biobank Research Team, Mägi R, Hoff M, Lerner UH, Henning P, Ullum H, Erikstrup C, Brunak S, Genomic Consortium DBDS, Langhammer A, Tuomi T, Oddsson A, Stefansson K, Pettersson-Kymmer U, Ostrowski SR, Pedersen OBV, Styrkarsdottir U, Mäkitie O, Hveem K, Richards JB, Ohlsson C (2023) An atlas of genetic determinants of forearm fracture. Nat Genet 55:1820-30. https://doi.org/10.1038/s41588-023-01527-3
Matteini AM, Tanaka T, Karasik D, Atzmon G, Chou WC, Eicher JD, Johnson AD, Arnold AM, Callisaya ML, Davies G, Evans DS, Holtfreter B, Lohman K, Lunetta KL, Mangino M, Smith AV, Smith JA, Teumer A, Yu L, Arking DE, Buchman AS, Chibinik LB, De Jager PL, Evans DA, Faul JD, Garcia ME, Gillham-Nasenya I, Gudnason V, Hofman A, Hsu YH, Ittermann T, Lahousse L, Liewald DC, Liu Y, Lopez L, Rivadeneira F, Rotter JI, Siggeirsdottir K, Starr JM, Thomson R, Tranah GJ, Uitterlinden AG, Völker U, Völzke H, Weir DR, Yaffe K, Zhao W, Zhuang WV, Zmuda JM, Bennett DA, Cummings SR, Deary IJ, Ferrucci L, Harris TB, Kardia SL, Kocher T, Kritchevsky SB, Psaty BM, Seshadri S, Spector TD, Srikanth VK, Windham BG, Zillikens MC, Newman AB, Walston JD, Kiel DP, Murabito JM (2016) GWAS analysis of handgrip and lower body strength in older adults in the CHARGE consortium. Aging Cell 15:792–800. https://doi.org/10.1111/acel.12468
Zillikens MC, Demissie S, Hsu Y, Yerges-Armstrong L, Chou W, Stolk L, Livshits G, Broer L, Johnson T, Koller DL, Kutalik Z, Luan J, Malkin I, Ried JS, Smith AV, Thorleifsson G, Vandenput L, Hua Zhao J, Zhang W, Aghdassi A, Åkesson K, Amin N, Baier LJ, Barroso I, Bennett DA, Bertram L, Biffar R, Bochud M, Boehnke M, Borecki IB, Buchman AS, Byberg L, Campbell H, Campos Obanda N, Cauley JA, Cawthon PM, Cederberg H, Chen Z, Cho NH, Jin Choi H, Claussnitzer M, Collins F, Cummings SR, De Jager PL, Demuth I, Dhonukshe-Rutten R, Diatchenko L, Eiriksdottir G, Enneman AW, Erdos M, Eriksson JG, Eriksson J, Estrada K, Evans DS, Feitosa MF, Fu M, Garcia M, Gieger C, Girke T, Glazer NL, Grallert H, Grewal J, Han B, Hanson RL, Hayward C, Hofman A, Hoffman EP, Homuth G, Hsueh W, Hubal MJ, Hubbard A, Huffman KM, Husted LB, Illig T, Ingelsson E, Ittermann T, Jansson J, Jordan JM, Jula A, Karlsson M, Khaw K, Kilpeläinen TO, Klopp N, Kloth JSL, Koistinen HA, Kraus WE, Kritchevsky S, Kuulasmaa T, Kuusisto J, Laakso M, Lahti J, Lang T, Langdahl BL, Launer LJ, Lee J, Lerch MM, Lewis JR, Lind L, Lindgren C, Liu Y, Liu T, Liu Y, Ljunggren Ö, Lorentzon M, Luben RN, Maixner W, McGuigan FE, Medina-Gomez C, Meitinger T, Melhus H, Mellström D, Melov S, Michaëlsson K, Mitchell BD, Morris AP, Mosekilde L, Newman A, Nielson CM, O’Connell JR, Oostra BA, Orwoll ES, Palotie A, Parker SCJ, Peacock M, Perola M, Peters A, Polasek O, Prince RL, Räikkönen K, Ralston SH, Ripatti S, Robbins JA, Rotter JI, Rudan I, Salomaa V, Satterfield S, Schadt EE, Schipf S, Scott L, Sehmi J, Shen J, Soo Shin C, Sigurdsson G, Smith S, Soranzo N, Stančáková A, Steinhagen-Thiessen E, Streeten EA, Styrkarsdottir U, Swart KMA, Tan S, Tarnopolsky MA, Thompson P, Thomson CA, Thorsteinsdottir U, Tikkanen E, Tranah GJ, Tuomilehto J, van Schoor NM, Verma A, Vollenweider P, Völzke H, Wactawski-Wende J, Walker M, Weedon MN, Welch R, Wichmann H, Widen E, Williams FMK, Wilson JF, Wright NC, Xie W, Yu L, Zhou Y, Chambers JC, Döring A, van Duijn CM, Econs MJ, Gudnason V, Kooner JS, Psaty BM, Spector TD, Stefansson K, Rivadeneira F, Uitterlinden AG, Wareham NJ, Ossowski V, Waterworth D, Loos RJF, Karasik D, Harris TB, Ohlsson C, Kiel DP (2017) Large meta-analysis of genome-wide association studies identifies five loci for lean body mass. Nat Commun 8:80. https://doi.org/10.1038/s41467-017-00031-7
Jiang X, O’Reilly PF, Aschard H, Hsu YH, Richards JB, Dupuis J, Ingelsson E, Karasik D, Pilz S, Berry D, Kestenbaum B, Zheng J, Luan J, Sofianopoulou E, Streeten EA, Albanes D, Lutsey PL, Yao L, Tang W, Econs MJ, Wallaschofski H, Völzke H, Zhou A, Power C, McCarthy MI, Michos ED, Boerwinkle E, Weinstein SJ, Freedman ND, Huang WY, Van Schoor NM, van der Velde N, Groot LCPGM, Enneman A, Cupples LA, Booth SL, Vasan RS, Liu CT, Zhou Y, Ripatti S, Ohlsson C, Vandenput L, Lorentzon M, Eriksson JG, Shea MK, Houston DK, Kritchevsky SB, Liu Y, Lohman KK, Ferrucci L, Peacock M, Gieger C, Beekman M, Slagboom E, Deelen J, Heemst DV, Kleber ME, März W, de Boer IH, Wood AC, Rotter JI, Rich SS, Robinson-Cohen C, den Heijer M, Jarvelin MR, Cavadino A, Joshi PK, Wilson JF, Hayward C, Lind L, Michaëlsson K, Trompet S, Zillikens MC, Uitterlinden AG, Rivadeneira F, Broer L, Zgaga L, Campbell H, Theodoratou E, Farrington SM, Timofeeva M, Dunlop MG, Valdes AM, Tikkanen E, Lehtimäki T, Lyytikäinen LP, Kähönen M, Raitakari OT, Mikkilä V, Ikram MA, Sattar N, Jukema JW, Wareham NJ, Langenberg C, Forouhi NG, Gundersen TE, Khaw KT, Butterworth AS, Danesh J, Spector T, Wang TJ, Hyppönen E, Kraft P, Kiel DP (2018) Genome-wide association study in 79,366 European-ancestry individuals informs the genetic architecture of 25-hydroxyvitamin D levels. Nat Commun 9:260–262. https://doi.org/10.1038/s41467-017-02662-2
Kanis JA (1994) Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: synopsis of a WHO report. WHO Study Group Osteoporos Int 4:368–381. https://doi.org/10.1007/BF01622200
Ho-Le TP, Center JR, Eisman JA, Nguyen HT, Nguyen TV (2017) Prediction of bone mineral density and fragility fracture by genetic profiling. J Bone Miner Res 32:285–293. https://doi.org/10.1002/jbmr.2998
Mitchell JA, Chesi A, Elci O, McCormack SE, Roy SM, Kalkwarf HJ, Lappe JM, Gilsanz V, Oberfield SE, Shepherd JA, Kelly A, Grant SF, Zemel BS (2016) Genetic risk scores implicated in adult bone fragility associate with pediatric bone density. J Bone Miner Res 31:789–795. https://doi.org/10.1002/jbmr.2744
Lu T, Forgetta V, Keller-Baruch J, Nethander M, Bennett D, Forest M, Bhatnagar S, Walters RG, Lin K, Chen Z, Li L, Karlsson M, Mellström D, Orwoll E, McCloskey EV, Kanis JA, Leslie WD, Clarke RJ, Ohlsson C, Greenwood CMT, Richards JB (2021) Improved prediction of fracture risk leveraging a genome-wide polygenic risk score. Genome Medicine 13:16. https://doi.org/10.1186/s13073-021-00838-6
Xiao X, Wu Q (2021) The utility of genetic risk score to improve performance of FRAX for fracture prediction in US postmenopausal women. Calcif Tissue Int 108:746–756. https://doi.org/10.1007/s00223-021-00809-4
Lee SH, Lee SW, Ahn SH, Kim T, Lim KH, Kim BJ, Cho EH, Kim SW, Kim TH, Kim GS, Kim SY, Koh JM, Kang C (2013) Multiple gene polymorphisms can improve prediction of nonvertebral fracture in postmenopausal women. J Bone Miner Res 28:2156–2164. https://doi.org/10.1002/jbmr.1955
Inouye M, Abraham G, Nelson CP, Wood AM, Sweeting MJ, Dudbridge F, Lai FY, Kaptoge S, Brozynska M, Wang T, Ye S, Webb TR, Rutter MK, Tzoulaki I, Patel RS, Loos RJF, Keavney B, Hemingway H, Thompson J, Watkins H, Deloukas P, Di Angelantonio E, Butterworth AS, Danesh J, Samani NJ (2018) Genomic risk prediction of coronary artery disease in 480,000 adults: implications for primary prevention. J Am Coll Cardiol 72:1883–1893. https://doi.org/10.1016/j.jacc.2018.07.079
Abraham G, Malik R, Yonova-Doing E, Salim A, Wang T, Danesh J, Butterworth AS, Howson JMM, Inouye M, Dichgans M (2019) Genomic risk score offers predictive performance comparable to clinical risk factors for ischaemic stroke. Nat Commun 10:5819. https://doi.org/10.1038/s41467-019-13848-1
Chen X, Liu C, Si S, Li Y, Li W, Yuan T, Xue F (2021) Genomic risk score provides predictive performance for type 2 diabetes in the UK biobank. Acta Diabetol 58:467–474. https://doi.org/10.1007/s00592-020-01650-1
Läll K, Lepamets M, Palover M, Esko T, Metspalu A, Tõnisson N, Padrik P, Mägi R, Fischer K (2019) Polygenic prediction of breast cancer: comparison of genetic predictors and implications for risk stratification. BMC Cancer 19:557–561. https://doi.org/10.1186/s12885-019-5783-1
Clifford J. Rosen The epidemiology and pathogenesis of osteoporosis
Kanis JA, Johnell O, Oden A, Johansson H, McCloskey E (2008) FRAX and the assessment of fracture probability in men and women from the UK. Osteoporos Int 19:385–397. https://doi.org/10.1007/s00198-007-0543-5
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R (2015) UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med 12:e1001779. https://doi.org/10.1371/journal.pmed.1001779
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, Motyer A, Vukcevic D, Delaneau O, O’Connell J, Cortes A, Welsh S, Young A, Effingham M, McVean G, Leslie S, Allen N, Donnelly P, Marchini J (2018) The UK Biobank resource with deep phenotyping and genomic data. Nature 562:203–209. https://doi.org/10.1038/s41586-018-0579-z
McCarthy S, Das S, Kretzschmar W, Delaneau O, Wood AR, Teumer A, Kang HM, Fuchsberger C, Danecek P, Sharp K, Luo Y, Sidore C, Kwong A, Timpson N, Koskinen S, Vrieze S, Scott LJ, Zhang H, Mahajan A, Veldink J, Peters U, Pato C, van Duijn CM, Gillies CE, Gandin I, Mezzavilla M, Gilly A, Cocca M, Traglia M, Angius A, Barrett JC, Boomsma D, Branham K, Breen G, Brummett CM, Busonero F, Campbell H, Chan A, Chen S, Chew E, Collins FS, Corbin LJ, Smith GD, Dedoussis G, Dorr M, Farmaki AE, Ferrucci L, Forer L, Fraser RM, Gabriel S, Levy S, Groop L, Harrison T, Hattersley A, Holmen OL, Hveem K, Kretzler M, Lee JC, McGue M, Meitinger T, Melzer D, Min JL, Mohlke KL, Vincent JB, Nauck M, Nickerson D, Palotie A, Pato M, Pirastu N, McInnis M, Richards JB, Sala C, Salomaa V, Schlessinger D, Schoenherr S, Slagboom PE, Small K, Spector T, Stambolian D, Tuke M, Tuomilehto J, Van den Berg LH, Van Rheenen W, Volker U, Wijmenga C, Toniolo D, Zeggini E, Gasparini P, Sampson MG, Wilson JF, Frayling T, de Bakker PI, Swertz MA, McCarroll S, Kooperberg C, Dekker A, Altshuler D, Willer C, Iacono W, Ripatti S, Soranzo N, Walter K, Swaroop A, Cucca F, Anderson CA, Myers RM, Boehnke M, McCarthy MI, Durbin R, Haplotype Reference Consortium (2016) A reference panel of 64,976 haplotypes for genotype imputation. Nat Genet 48:1279-83. https://doi.org/10.1038/ng.3643
Estrada K, Styrkarsdottir U, Evangelou E, Hsu YH, Duncan EL, Ntzani EE, Oei L, Albagha OM, Amin N, Kemp JP, Koller DL, Li G, Liu CT, Minster RL, Moayyeri A, Vandenput L, Willner D, Xiao SM, Yerges-Armstrong LM, Zheng HF, Alonso N, Eriksson J, Kammerer CM, Kaptoge SK, Leo PJ, Thorleifsson G, Wilson SG, Wilson JF, Aalto V, Alen M, Aragaki AK, Aspelund T, Center JR, Dailiana Z, Duggan DJ, Garcia M, Garcia-Giralt N, Giroux S, Hallmans G, Hocking LJ, Husted LB, Jameson KA, Khusainova R, Kim GS, Kooperberg C, Koromila T, Kruk M, Laaksonen M, Lacroix AZ, Lee SH, Leung PC, Lewis JR, Masi L, Mencej-Bedrac S, Nguyen TV, Nogues X, Patel MS, Prezelj J, Rose LM, Scollen S, Siggeirsdottir K, Smith AV, Svensson O, Trompet S, Trummer O, van Schoor NM, Woo J, Zhu K, Balcells S, Brandi ML, Buckley BM, Cheng S, Christiansen C, Cooper C, Dedoussis G, Ford I, Frost M, Goltzman D, González-Macías J, Kähönen M, Karlsson M, Khusnutdinova E, Koh JM, Kollia P, Langdahl BL, Leslie WD, Lips P, Ljunggren Ö, Lorenc RS, Marc J, Mellström D, Obermayer-Pietsch B, Olmos JM, Pettersson-Kymmer U, Reid DM, Riancho JA, Ridker PM, Rousseau F, Slagboom PE, Tang NL, Urreizti R, Van Hul W, Viikari J, Zarrabeitia MT, Aulchenko YS, Castano-Betancourt M, Grundberg E, Herrera L, Ingvarsson T, Johannsdottir H, Kwan T, Li R, Luben R, Medina-Gómez C, Palsson ST, Reppe S, Rotter JI, Sigurdsson G, van Meurs JB, Verlaan D, Williams FM, Wood AR, Zhou Y, Gautvik KM, Pastinen T, Raychaudhuri S, Cauley JA, Chasman DI, Clark GR, Cummings SR, Danoy P, Dennison EM, Eastell R, Eisman JA, Gudnason V, Hofman A, Jackson RD, Jones G, Jukema JW, Khaw KT, Lehtimäki T, Liu Y, Lorentzon M, McCloskey E, Mitchell BD, Nandakumar K, Nicholson GC, Oostra BA, Peacock M, Pols HA, Prince RL, Raitakari O, Reid IR, Robbins J, Sambrook PN, Sham PC, Shuldiner AR, Tylavsky FA, van Duijn CM, Wareham NJ, Cupples LA, Econs MJ, Evans DM, Harris TB, Kung AW, Psaty BM, Reeve J, Spector TD, Streeten EA, Zillikens MC, Thorsteinsdottir U, Ohlsson C, Karasik D, Richards JB, Brown MA, Stefansson K, Uitterlinden AG, Ralston SH, Ioannidis JP, Kiel DP, Rivadeneira F (2012) Genome-wide meta-analysis identifies 56 bone mineral density loci and reveals 14 loci associated with risk of fracture. Nat Genet 44:491–501. https://doi.org/10.1038/ng.2249
Medina-Gomez C, Kemp JP, Trajanoska K, Luan J, Chesi A, Ahluwalia TS, Mook-Kanamori DO, Ham A, Hartwig FP, Evans DS, Joro R, Nedeljkovic I, Zheng HF, Zhu K, Atalay M, Liu CT, Nethander M, Broer L, Porleifsson G, Mullin BH, Handelman SK, Nalls MA, Jessen LE, Heppe DHM, Richards JB, Wang C, Chawes B, Schraut KE, Amin N, Wareham N, Karasik D, Van der Velde N, Ikram MA, Zemel BS, Zhou Y, Carlsson CJ, Liu Y, McGuigan FE, Boer CG, Bønnelykke K, Ralston SH, Robbins JA, Walsh JP, Zillikens MC, Langenberg C, Li-Gao R, Williams FMK, Harris TB, Akesson K, Jackson RD, Sigurdsson G, den Heijer M, van der Eerden BCJ, van de Peppel J, Spector TD, Pennell C, Horta BL, Felix JF, Zhao JH, Wilson SG, de Mutsert R, Bisgaard H, Styrkársdóttir U, Jaddoe VW, Orwoll E, Lakka TA, Scott R, Grant SFA, Lorentzon M, van Duijn CM, Wilson JF, Stefansson K, Psaty BM, Kiel DP, Ohlsson C, Ntzani E, van Wijnen AJ, Forgetta V, Ghanbari M, Logan JG, Williams GR, Bassett JHD, Croucher PI, Evangelou E, Uitterlinden AG, Ackert-Bicknell CL, Tobias JH, Evans DM, Rivadeneira F (2018) Life-course genome-wide association study meta-analysis of total body BMD and assessment of age-specific effects. Am J Hum Genet 102:88–102. https://doi.org/10.1016/j.ajhg.2017.12.005
O'Seaghdha CM, Wu H, Yang Q, Kapur K, Guessous I, Zuber AM, Köttgen A, Stoudmann C, Teumer A, Kutalik Z, Mangino M, Dehghan A, Zhang W, Eiriksdottir G, Li G, Tanaka T, Portas L, Lopez LM, Hayward C, Lohman K, Matsuda K, Padmanabhan S, Firsov D, Sorice R, Ulivi S, Brockhaus AC, Kleber ME, Mahajan A, Ernst FD, Gudnason V, Launer LJ, Mace A, Boerwinckle E, Arking DE, Tanikawa C, Nakamura Y, Brown MJ, Gaspoz JM, Theler JM, Siscovick DS, Psaty BM, Bergmann S, Vollenweider P, Vitart V, Wright AF, Zemunik T, Boban M, Kolcic I, Navarro P, Brown EM, Estrada K, Ding J, Harris TB, Bandinelli S, Hernandez D, Singleton AB, Girotto G, Ruggiero D, d'Adamo AP, Robino A, Meitinger T, Meisinger C, Davies G, Starr JM, Chambers JC, Boehm BO, Winkelmann BR, Huang J, Murgia F, Wild SH, Campbell H, Morris AP, Franco OH, Hofman A, Uitterlinden AG, Rivadeneira F, Völker U, Hannemann A, Biffar R, Hoffmann W, Shin SY, Lescuyer P, Henry H, Schurmann C, SUNLIGHT Consortium, GEFOS Consortium, Munroe PB, Gasparini P, Pirastu N, Ciullo M, Gieger C, März W, Lind L, Spector TD, Smith AV, Rudan I, Wilson JF, Polasek O, Deary IJ, Pirastu M, Ferrucci L, Liu Y, Kestenbaum B, Kooner JS, Witteman JC, Nauck M, Kao WH, Wallaschofski H, Bonny O, Fox CS, Bochud M (2013) Meta-analysis of genome-wide association studies identifies six new loci for serum calcium concentrations. PLoS Genet 9:e1003796. https://doi.org/10.1371/journal.pgen.1003796
van Meurs JB, Pare G, Schwartz SM, Hazra A, Tanaka T, Vermeulen SH, Cotlarciuc I, Yuan X, Mälarstig A, Bandinelli S, Bis JC, Blom H, Brown MJ, Chen C, Chen YD, Clarke RJ, Dehghan A, Erdmann J, Ferrucci L, Hamsten A, Hofman A, Hunter DJ, Goel A, Johnson AD, Kathiresan S, Kampman E, Kiel DP, Kiemeney LA, Chambers JC, Kraft P, Lindemans J, McKnight B, Nelson CP, O’Donnell CJ, Psaty BM, Ridker PM, Rivadeneira F, Rose LM, Seedorf U, Siscovick DS, Schunkert H, Selhub J, Ueland PM, Vollenweider P, Waeber G, Waterworth DM, Watkins H, Witteman JC, den Heijer M, Jacques P, Uitterlinden AG, Kooner JS, Rader DJ, Reilly MP, Mooser V, Chasman DI, Samani NJ, Ahmadi KR (2013) Common genetic loci influencing plasma homocysteine concentrations and their effect on risk of coronary artery disease. Am J Clin Nutr 98:668–676. https://doi.org/10.3945/ajcn.112.044545
Teumer A, Chaker L, Groeneweg S, Li Y, Di Munno C, Barbieri C, Schultheiss UT, Traglia M, Ahluwalia TS, Akiyama M, Appel EVR, Arking DE, Arnold A, Astrup A, Beekman M, Beilby JP, Bekaert S, Boerwinkle E, Brown SJ, De Buyzere M, Campbell PJ, Ceresini G, Cerqueira C, Cucca F, Deary IJ, Deelen J, Eckardt K, Ekici AB, Eriksson JG, Ferrrucci L, Fiers T, Fiorillo E, Ford I, Fox CS, Fuchsberger C, Galesloot TE, Gieger C, Gögele M, De Grandi A, Grarup N, Greiser KH, Haljas K, Hansen T, Harris SE, van Heemst D, den Heijer M, Hicks AA, den Hollander W, Homuth G, Hui J, Ikram MA, Ittermann T, Jensen RA, Jing J, Jukema JW, Kajantie E, Kamatani Y, Kasbohm E, Kaufman J, Kiemeney LA, Kloppenburg M, Kronenberg F, Kubo M, Lahti J, Lapauw B, Li S, Liewald DCM, Alizadeh BZ, Boezen HM, Franke L, van der Harst P, Navis G, Rots M, Snieder H, Swertz MA, Wijmenga C, Lim EM, Linneberg A, Marina M, Mascalzoni D, Matsuda K, Medenwald D, Meisinger C, Meulenbelt I, De Meyer T, Meyer zu Schwabedissen HE, Mikolajczyk R, Moed M, Netea-Maier R, Nolte IM, Okada Y, Pala M, Pattaro C, Pedersen O, Petersmann A, Porcu E, Postmus I, Pramstaller PP, Psaty BM, Ramos YFM, Rawal R, Redmond P, Richards JB, Rietzschel ER, Rivadeneira F, Roef G, Rotter JI, Sala CF, Schlessinger D, Selvin E, Slagboom PE, Soranzo N, Sørensen TIA, Spector TD, Starr JM, Stott DJ, Taes Y, Taliun D, Tanaka T, Thuesen B, Tiller D, Toniolo D, Uitterlinden AG, Visser WE, Walsh JP, Wilson SG, Wolffenbuttel BHR, Yang Q, Zheng H, Cappola A, Peeters RP, Naitza S, Völzke H, Sanna S, Köttgen A, Visser TJ, Medici M, Lifelines CS (2018) Genome-wide analyses identify a role for SLC17A4 and AADAT in thyroid hormone regulation. Nat Commun 9:4455. https://doi.org/10.1038/s41467-018-06356-1
Lagou V, Mägi R, Hottenga JJ, Grallert H, Perry JRB, Bouatia-Naji N, Marullo L, Rybin D, Jansen R, Min JL, Dimas AS, Ulrich A, Zudina L, Gådin JR, Jiang L, Faggian A, Bonnefond A, Fadista J, Stathopoulou MG, Isaacs A, Willems SM, Navarro P, Tanaka T, Jackson AU, Montasser ME, O’Connell JR, Bielak LF, Webster RJ, Saxena R, Stafford JM, Pourcain BS, Timpson NJ, Salo P, Shin S, Amin N, Smith AV, Li G, Verweij N, Goel A, Ford I, Johnson PCD, Johnson T, Kapur K, Thorleifsson G, Strawbridge RJ, Rasmussen-Torvik L, Esko Tõ, Mihailov E, Fall T, Fraser RM, Mahajan A, Kanoni S, Giedraitis V, Kleber ME, Silbernagel G, Meyer J, Müller-Nurasyid M, Ganna A, Sarin A, Yengo L, Shungin D, Luan J, Horikoshi M, An P, Sanna S, Boettcher Y, Rayner NW, Nolte IM, Zemunik T, Iperen Ev, Kovacs P, Hastie ND, Wild SH, McLachlan S, Campbell S, Polasek O, Carlson O, Egan J, Kiess W, Willemsen G, Kuusisto J, Laakso M, Dimitriou M, Hicks AA, Rauramaa R, Bandinelli S, Thorand B, Liu Y, Miljkovic I, Lind L, Doney A, Perola M, Hingorani A, Kivimaki M, Kumari M, Bennett AJ, Groves CJ, Herder C, Koistinen HA, Kinnunen L, Faire Ud, Bakker SJL, Uusitupa M, Palmer CNA, Jukema JW, Sattar N, Pouta A, Snieder H, Boerwinkle E, Pankow JS, Magnusson PK, Krus U, Scapoli C, de Geus EJCN, Blüher M, Wolffenbuttel BHR, Province MA, Abecasis GR, Meigs JB, Hovingh GK, Lindström J, Wilson JF, Wright AF, Dedoussis GV, Bornstein SR, Schwarz PEH, Tönjes A, Winkelmann BR, Boehm BO, März W, Metspalu A, Price JF, Deloukas P, Körner A, Lakka TA, Keinanen-Kiukaanniemi S, Saaristo TE, Bergman RN, Tuomilehto J, Wareham NJ, Langenberg C, Männistö S, Franks PW, Hayward C, Vitart V, Kaprio J, Visvikis-Siest S, Balkau B, Altshuler D, Rudan I, Stumvoll M, Campbell H, van Duijn CM, Gieger C, Illig T, Ferrucci L, Pedersen NL, Pramstaller PP, Boehnke M, Frayling TM, Shuldiner AR, Peyser PA, Kardia SLR, Palmer LJ, Penninx BW, Meneton P, Harris TB, Navis G, Harst Pvd, Smith GD, Forouhi NG, Loos RJF, Salomaa V, Soranzo N, Boomsma DI, Groop L, Tuomi T, Hofman A, Munroe PB, Gudnason V, Siscovick DS, Watkins H, Lecoeur C, Vollenweider P, Franco-Cereceda A, Eriksson P, Jarvelin M, Stefansson K, Hamsten A, Nicholson G, Karpe F, Dermitzakis ET, Lindgren CM, McCarthy MI, Froguel P, Kaakinen MA, Lyssenko V, Watanabe RM, Ingelsson E, Florez JC, Dupuis J, Barroso I, Morris AP, Prokopenko I, Meta-Analyses of Glucose and Insulin-related traits Consortium, (MAGIC) (2021) Sex-dimorphic genetic effects and novel loci for fasting glucose and insulin variability. Nat Commun 12:24. https://doi.org/10.1038/s41467-020-19366-9
Robertson CC, Inshaw JRJ, Onengut-Gumuscu S, Chen W, Santa Cruz DF, Yang H, Cutler AJ, Crouch DJM, Farber E, Bridges SL, Edberg JC, Kimberly RP, Buckner JH, Deloukas P, Divers J, Dabelea D, Lawrence JM, Marcovina S, Shah AS, Greenbaum CJ, Atkinson MA, Gregersen PK, Oksenberg JR, Pociot F, Rewers MJ, Steck AK, Dunger DB, Wicker LS, Concannon P, Todd JA, Rich SS, Type 1 Diabetes GC (2021) Fine-mapping, trans-ancestral and genomic analyses identify causal variants, cells, genes and drug targets for type 1 diabetes. Nat Genet 53:962-71. https://doi.org/10.1038/s41588-021-00880-5
Vujkovic M, Keaton JM, Lynch JA, Miller DR, Zhou J, Tcheandjieu C, Huffman JE, Assimes TL, Lorenz K, Zhu X, Hilliard AT, Judy RL, Huang J, Lee KM, Klarin D, Pyarajan S, Danesh J, Melander O, Rasheed A, Mallick NH, Hameed S, Qureshi IH, Afzal MN, Malik U, Jalal A, Abbas S, Sheng X, Gao L, Kaestner KH, Susztak K, Sun YV, DuVall SL, Cho K, Lee JS, Gaziano JM, Phillips LS, Meigs JB, Reaven PD, Wilson PW, Edwards TL, Rader DJ, Damrauer SM, O’Donnell CJ, Tsao PS, Atkinson MA, Powers AC, Naji A, Kaestner KH, Abecasis GR, Baras A, Cantor MN, Coppola G, Economides AN, Lotta LA, Overton JD, Reid JG, Shuldiner AR, Beechert C, Forsythe C, Fuller ED, Gu Z, Lattari M, Lopez AE, Schleicher TD, Padilla MS, Toledo K, Widom L, Wolf SE, Pradhan M, Manoochehri K, Ulloa RH, Bai X, Balasubramanian S, Barnard L, Blumenfeld AL, Eom G, Habegger L, Hawes A, Khalid S, Maxwell EK, Salerno WJ, Staples JC, Yadav A, Jones MB, Mitnaul LJ, Aguayo SM, Ahuja SK, Ballas ZK, Bhushan S, Boyko EJ, Cohen DM, Concato J, Constans JI, Dellitalia LJ, Fayad JM, Fernando RS, Florez HJ, Gaddy MA, Gappy SS, Gibson G, Godschalk M, Greco JA, Gupta S, Gutierrez S, Hammer KD, Hamner MB, Harley JB, Hung AM, Huq M, Hurley RA, Iruvanti PR, Ivins DJ, Jacono FJ, Jhala DN, Kaminsky LS, Kinlay S, Klein JB, Liangpunsakul S, Lichy JH, Mastorides SM, Mathew RO, Mattocks KM, McArdle R, Meyer PN, Meyer LJ, Moorman JP, Morgan TR, Murdoch M, Nguyen XT, Okusaga OO, Oursler KK, Ratcliffe NR, Rauchman MI, Robey RB, Ross GW, Servatius RJ, Sharma SC, Sherman SE, Sonel E, Sriram P, Stapley T, Striker RT, Tandon N, Villareal G, Wallbom AS, Wells JM, Whittle JC, Whooley MA, Xu J, Yeh S, Aslan M, Brewer JV, Brophy MT, Connor T, Argyres DP, Do NV, Hauser ER, Humphries DE, Selva LE, Shayan S, Stephens B, Whitbourne SB, Zhao H, Moser J, Beckham JC, Breeling JL, Romero JPC, Huang GD, Ramoni RB, Pyarajan S, Sun YV, Cho K, Wilson PW, O’Donnell CJ, Tsao PS, Chang K, Gaziano JM, Muralidhar S, Chang K, Voight BF, Saleheen D, The HC, Regeneron GC, VA Million VP (2020) Discovery of 318 new risk loci for type 2 diabetes and related vascular outcomes among 1.4 million participants in a multi-ancestry meta-analysis. Nat Genet 52:680-91. https://doi.org/10.1038/s41588-020-0637-y
Ha E, Bae SC, Kim K (2021) Large-scale meta-analysis across East Asian and European populations updated genetic architecture and variant-driven biology of rheumatoid arthritis, identifying 11 novel susceptibility loci. Ann Rheum Dis 80:558–565. https://doi.org/10.1136/annrheumdis-2020-219065
Liu JZ, van Sommeren S, Huang H, Ng SC, Alberts R, Takahashi A, Ripke S, Lee JC, Jostins L, Shah T, Abedian S, Cheon JH, Cho J, Daryani NE, Franke L, Fuyuno Y, Hart A, Juyal RC, Juyal G, Kim WH, Morris AP, Poustchi H, Newman WG, Midha V, Orchard TR, Vahedi H, Sood A, Sung JJY, Malekzadeh R, Westra H, Yamazaki K, Yang S, Barrett JC, Franke A, Alizadeh BZ, Parkes M, Thelma BK, Daly MJ, Kubo M, Anderson CA, Weersma RK, International Multiple Sclerosis GC, International IBD GC (2015) Association analyses identify 38 susceptibility loci for inflammatory bowel disease and highlight shared genetic risk across populations. Nat Genet 47:979-86. https://doi.org/10.1038/ng.3359
Styrkarsdottir U, Stefansson OA, Gunnarsdottir K, Thorleifsson G, Lund SH, Stefansdottir L, Juliusson K, Agustsdottir AB, Zink F, Halldorsson GH, Ivarsdottir EV, Benonisdottir S, Jonsson H, Gylfason A, Norland K, Trajanoska K, Boer CG, Southam L, Leung JCS, Tang NLS, Kwok TCY, Lee JSW, Ho SC, Byrjalsen I, Center JR, Lee SH, Koh J, Lohmander LS, Ho-Pham L, Nguyen TV, Eisman JA, Woo J, Leung P, Loughlin J, Zeggini E, Christiansen C, Rivadeneira F, van Meurs J, Uitterlinden AG, Mogensen B, Jonsson H, Ingvarsson T, Sigurdsson G, Benediktsson R, Sulem P, Jonsdottir I, Masson G, Holm H, Norddahl GL, Thorsteinsdottir U, Gudbjartsson DF, Stefansson K (2019) GWAS of bone size yields twelve loci that also affect height, BMD, osteoarthritis or fractures. Nat Commun 10:2054. https://doi.org/10.1038/s41467-019-09860-0
Nikpay M, Goel A, Won H, Hall LM, Willenborg C, Kanoni S, Saleheen D, Kyriakou T, Nelson CP, Hopewell JC, Webb TR, Zeng L, Dehghan A, Alver M, Armasu SM, Auro K, Bjonnes A, Chasman DI, Chen S, Ford I, Franceschini N, Gieger C, Grace C, Gustafsson S, Huang J, Hwang S, Kim YK, Kleber ME, Lau KW, Lu X, Lu Y, Lyytikäinen L, Mihailov E, Morrison AC, Pervjakova N, Qu L, Rose LM, Salfati E, Saxena R, Scholz M, Smith AV, Tikkanen E, Uitterlinden A, Yang X, Zhang W, Zhao W, de Andrade M, de Vries P,S., van Zuydam N,R., Anand SS, Bertram L, Beutner F, Dedoussis G, Frossard P, Gauguier D, Goodall AH, Gottesman O, Haber M, Han B, Huang J, Jalilzadeh S, Kessler T, König I,R., Lannfelt L, Lieb W, Lind L, Lindgren CM, Lokki M, Magnusson PK, Mallick NH, Mehra N, Meitinger T, Memon F, Morris AP, Nieminen MS, Pedersen NL, Peters A, Rallidis LS, Rasheed A, Samuel M, Shah SH, Sinisalo J, Stirrups KE, Trompet S, Wang L, Zaman KS, Ardissino D, Boerwinkle E, Borecki IB, Bottinger EP, Buring JE, Chambers JC, Collins R, Cupples LA, Danesh J, Demuth I, Elosua R, Epstein SE, Esko Tõ, Feitosa MF, Franco OH, Franzosi MG, Granger CB, Gu D, Gudnason V, Hall AS, Hamsten A, Harris TB, Hazen SL, Hengstenberg C, Hofman A, Ingelsson E, Iribarren C, Jukema JW, Karhunen PJ, Kim B, Kooner JS, Kullo IJ, Lehtimäki T, Loos RJF, Melander O, Metspalu A, März W, Palmer CN, Perola M, Quertermous T, Rader DJ, Ridker PM, Ripatti S, Roberts R, Salomaa V, Sanghera DK, Schwartz SM, Seedorf U, Stewart AF, Stott DJ, Thiery J, Zalloua PA, O'Donnell C,J., Reilly MP, Assimes TL, Thompson JR, Erdmann J, Clarke R, Watkins H, Kathiresan S, McPherson R, Deloukas P, Schunkert H, Samani NJ, Farrall M, the CC (2015) A comprehensive 1000 Genomes–based genome-wide association meta-analysis of coronary artery disease. Nat Genet 47:1121-30. https://doi.org/10.1038/ng.3396
Privé F, Arbel J, Vilhjálmsson BJ (2020) LDpred2: better, faster, stronger. Bioinformatics 36:5424–5431. https://doi.org/10.1093/bioinformatics/btaa1029
Zou H, Hastie T (2005) Regularization and variable selection via the Elastic Net. Journal of the Royal Statistical Society. Series B (Statistical Methodology) 67:301–320
Cosman F, de Beur SJ, LeBoff MS, Lewiecki EM, Tanner B, Randall S, Lindsay R, Foundation NO (2014) Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int 25:2359–2381. https://doi.org/10.1007/s00198-014-2794-2
Bulik-Sullivan B, Finucane HK, Anttila V, Gusev A, Day FR, Loh P, Duncan L, Perry JRB, Patterson N, Robinson EB, Daly MJ, Price AL, Neale BM, Consortium R, Psychiatric GC, Genetic Consortium for Anorexia Nervosa of the Wellcome Trust Case Control, Consortium 3 (2015) An atlas of genetic correlations across human diseases and traits. Nat Genet 47:1236-41. https://doi.org/10.1038/ng.3406
Xiao X, Wu Q (2023) The clinical utility of the BMD-related comprehensive genome-wide polygenic score in identifying individuals with a high risk of osteoporotic fractures. Osteoporos Int. https://doi.org/10.1007/s00198-022-06654-x
Acknowledgements
The research and analysis described in the current publication were supported by a grant (R21MD013681) from the National Institute on Minority Health and Health Disparities, a grant (R01AG080017) from the National Institute of Aging, and a grant (P20GM121325) from the National Institute of General Medical Sciences. The funding sponsors were not involved in the study design, genotype imputation, data analysis, interpretation of the analysis results, or the manuscript’s preparation, review, or approval. In addition, the National Supercomputing Institute at the University of Nevada Las Vegas provided facilities for bioinformatical analysis in this study. The authors thank Dr. Ann Vuong from the Department of Epidemiology and Biostatistics, School of Public Health, the University of Nevada Las Vegas, for reviewing and editing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This research work was approved by the UK Biobank and the institutional review board at the University of Nevada, Las Vegas. This study uses the UK Biobank Data Resource under application number 58122.
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Xiao, X., Wu, Q. Enhanced fracture risk prediction: a novel multi-trait genetic approach integrating polygenic scores of fracture-related traits. Osteoporos Int (2024). https://doi.org/10.1007/s00198-024-07105-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00198-024-07105-5