Abstract
Summary
Hip fractures are associated with significant healthcare costs. In frail institutionalized patients, the costs of nonoperative management are less than operative management with comparable short-term quality of life. Nonoperative management of hip fractures in patients at the end of life should be openly discussed with SDM.
Purpose
The aim was to describe healthcare use with associated costs and to determine cost-utility of nonoperative management (NOM) versus operative management (OM) of frail institutionalized older patients with a proximal femoral fracture.
Methods
This study included institutionalized patients with a limited life expectancy aged ≥ 70 years who sustained a proximal femoral fracture in the Netherlands. Costs of hospital- and nursing home care were calculated. Quality adjusted life years (QALY) were calculated based on EuroQol-5D-5L utility scores at day 7, 14, and 30 and at 3 and 6 months. The incremental cost-effectiveness ratio (ICER) was calculated from a societal perspective.
Results
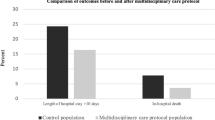
Of the 172 enrolled patients, 88 (51%) patients opted for NOM and 84 (49%) for OM. NOM was associated with lower healthcare costs at 6 months (NOM; €2425 (SD 1.030), OM; €9325 (SD 4242), p < 0.001). The main cost driver was hospital stay (NOM; €738 (SD 841) and OM; €3140 (SD 2636)). The ICER per QALY gained in the OM versus NOM was €76,912 and exceeded the threshold of €20,000 per QALY. The gained QALY were minimal in the OM group in patients who died within 14- and 30-day post-injury, but OM resulted in more than triple the costs.
Conclusion
OM results in significant higher healthcare costs, mainly due to the length of hospital stay. For frail patients at the end of life, NOM of proximal femoral fractures should be openly discussed in SDM conversations due to the limited gain in QoL.
Trial registration.
Netherlands Trial Register (NTR7245; date 10–06-2018).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The economic burden of disease of proximal femur fractures increases annually, and progressive aging is expected to be an important driver for healthcare service allocation and costs. Currently, approximately 1.3 million persons around the globe sustain a proximal femoral fracture annually. By 2050, this number is expected to increase to 7.3 million patients worldwide with annual costs of $131 billion due to progressive aging [1,2,3]. Approximately 20–25% of the proximal femoral fractures occur in patients who reside in long-term care facilities [4]. Especially in these frail patients, proximal femoral fractures are a devastating injury with a high impact on their already limited life expectancy and result in poor functional outcomes [5,6,7]. Because of these poor outcomes, proximal femoral fractures in frail older patients can be seen as a life-threatening condition. Therefore, in selected cases of patients with a limited life expectancy due to frailty, a more holistic, palliative care-related approach could be applied. Nonoperative management (NOM) with a palliative care approach of proximal femoral fractures can be considered as an alternative in patients with a limited life expectancy, but only if this aligns with the intended individual goals of care. This accounts especially in cases where poor outcomes are expected and operative management (OM) might not contribute to the patient’s health-related quality of life (HRQoL), because of the high risk of adverse events and unsuccessful rehabilitation [7,8,9].
However, due to the limited evidence on outcomes of NOM, it is underexposed in current guidelines as a treatment strategy for selected patients with a limited life expectancy and/or limited quality of life. Consequently, OM is the standard treatment and over 95% of the patients are treated surgically in the Netherlands [10,11,12,13]. It is remarkable that, considering the high prevalence of proximal femoral fractures in nursing home residents, few studies have described healthcare utilization, HRQoL, and cost-utility data of these institutionalized patients who sustain a proximal femoral fracture [8, 14, 15]. Detailed information on healthcare costs are gaining importance as burden of disease keeps increasing annually. Identifying service utilization patterns enables future healthcare planning identify cost drivers, possible areas of improvement and cost-reduction, without compromising the quality of life for this expanding population.
The FRAIL-HIP study aimed to compare QoL, functional outcome, treatment satisfaction, and cost outcomes of OM versus NOM in frail institutionalized older patients with a limited life expectancy in a multicenter cohort study [9, 16]. The study showed that NOM is non-inferior to OM with regards to QoL and results in high treatment satisfaction [16]. The aim of the present study was to describe the healthcare utilization and total medical costs and to evaluate the cost-utility of NOM versus OM in frail institutionalized older patients with a limited life expectancy who sustained a proximal femoral fracture.
Methods
Study design and participants
The economic evaluation study is based on data from the FRAIL-HIP study [9]. This was a multicenter prospective cohort study conducted to evaluate the effect of NOM versus OM with regard to QoL and other key outcomes of frail institutionalized older patients with a limited life expectancy who sustained a proximal femoral fracture. The study was registered at the Netherlands Trial Register (NTR7245). The study protocol and results of this study have been published elsewhere [9]. The study was approved by the Medical Research Ethics Committees of all participating centers.
A total of 25 hospitals participated and enrolled 172 patients between September 1, 2018, and April 25, 2020. Patients were enrolled if they were aged ≥ 70 years, sustained a proximal femoral fracture (femoral neck or trochanteric; AO/OTA-type 31-A.1–3), resided in a nursing home pre-trauma, and were classified as frail. Frail was defined as either malnutrition (body mass index (BMI) of < 18.5 km/m2 or cachexia), existing mobility issues (Functional Ambulation Category (FAC) ≤ 2), or severe comorbidities (American Society of Anesthesiologists (ASA) class 4 or 5). Patients were excluded if they sustained a subtrochanteric fracture, bilateral proximal femoral fractures, and periprosthetic fracture, had a delay of diagnosis of more than seven days, had known metastatic disease and a confirmed pathological fracture, had insufficient comprehension of the Dutch language, or participated in another surgical intervention or drug study that could have influenced the results.
Treatment and assessment
Treatment decision was reached following a structured shared decision process, in which pros and cons of both operative and nonoperative management were discussed with the patient if mentally capable, his/her relatives, and all relevant care providers involved. After shared decision-making (SDM), patients or their proxy opted for NOM or OM.
The main outcomes of this study were healthcare consumption, total direct medical costs, and quality adjusted life years (QALYs). Data were prospectively obtained at 7, 14, and 30 days and 3- and 6-month post-trauma by physical interviews. During these visits, EuroQol-5D-5L (EQ-5D) questionnaires were completed, and healthcare consumption was registered via a predefined case report form [17].
Healthcare consumption and cost assessment
Healthcare consumption included emergency department (ED) and hospital care use, medical interventions, outpatient follow-up, hospital readmissions, nursing home care, hospice care, involved medical specialists and other healthcare providers (e.g., physical therapists and dieticians), and additional medication use during follow-up. Data were collected by a questionnaire at each visit that was based on the Medical Consumption Questionnaire [18].
Indirect costs due to productivity loss were considered zero since the study population consisted of older nursing home patients only. Therefore, only direct medical costs were determined.
Costs were calculated by multiplying consumption volumes with the corresponding unit prices (Table 1). Costs of the interventions were estimated using a microcosting study and consisted of costs of the operating room (costs per minute including overhead costs) and costs of the implants. Prices of the operating room and implants were derived from previous Dutch studies and financial departments of participating hospitals [19, 20]. Most other cost prices of healthcare resources were derived from the Dutch manual on cost research, methods, and standards costs in economic healthcare evaluations in accordance with economic guidelines [21]. Unit costs of all diagnostic procedures (radiology or laboratory studies) were derived from the NZA (Nederlandse Zorgautoriteit; Dutch Healthcare Authority) [22]. Costs for medication use were calculated using standard prices per dose as described by the Dutch Health Care Insurance Board [23]. Prices for wheelchairs and other walking aids were not included, since most patients in the study already used these aids prior to the trauma. Cost prices of non-academic hospitals were used, since only one study participant was treated in an academic hospital. As the study population concerned pre-fracture long-term care residents, the out of hospital costs were primarily presented without the costs for nursing home stay as these were not additional costs since all included study participants resided in a nursing home pre-trauma and since these costs were mainly dependent on life expectancy. However, total healthcare costs were presented with and without the costs of nursing home stay. Direct costs of adverse events were based on costs of return visits to the ED, readmission to the hospital, and reinterventions.
Subgroup analyses were performed with respect to gender, fracture type (femoral neck or trochanteric), and three frailty parameters (ASA classification (≤ 3 or > 3), BMI (< 18.5 or ≥ 18.5), and FAC- score (≤ 2 and > 2).
Health-related quality of life
Health-related quality of life (HRQOL) was expressed in utilities derived from the EQ-5D. The EQ-5D is often used in femoral fracture patients and especially for economic assessments in trauma patients [24]. This generic instrument is used to measure health status using five health dimensions (mobility, self-care, usual activities, pain/discomfort, and anxiety/depression) with each dimension having five response levels. For the purpose of this study, the proxy-patient version was completed by proxies due to the degree of cognitive impairment of most patients [25]. All measurements per patient were completed by the same proxy. Health status descriptions from the EQ-5D can be valued using tariffs from preference elicitation studies to calculate utilities, which can be used to calculate QALYs. Utility scores were derived from the EQ-5D using the Dutch value set [26]. Negative values were also possible and represent health states worse than death. Utility values calculated with the Dutch value set range from − 0.329 to 1.000. The utility values were presented for patients alive at each specific time point.
QALYs were calculated based on the measured EQ-5D utility scores at day 7, day 14, day 30, and 3 and 6 months. The number of QALYs between two follow-up moments was valued using the average utility value of the two measurement points. In case of missing utility values at a follow-up moment, the following known utility value was used to determine the average utility value for the period between the two time points. If patients died prior to the end of follow-up, the last known utility score of the last known measurement was used to calculate the QALY from the last known measurement until the date of decease. Since the follow-up of the current study was 6 months and utilities are maximized at 1.00, the maximum QALY value in this study was 0.5.
Cost-utility analysis
Cost-utility analyses was performed in a Dutch setting from a societal perspective applying a lifetime horizon with costs expressed in 2020 Euros and effects in QALYs. Cost-utility was determined with the incremental cost-effectiveness ratio (ICER). The ICER was calculated by dividing the difference in mean costs of OM and NOM by the difference in gained QALYs between these groups. Cost-effectiveness was determined based on the reference values of the maximum costs per QALY gained. As established by the Zorginstituut Nederland (National health Care Institute of the Netherlands), these maximum costs were €20,000 per gained QALY for the threshold of 0.1–0.4 QALY gained in our study [27].
Statistical analysis
Data were analyzed using the Statistical Package for the Social Sciences (SPSS) version 25 (SPSS, Chicago, Ill., USA) and reported following the STrengthening the Reporting of OBservational studies in Epidemiology (STROBE) guidelines [28]. Missing data were not imputed, since the proportion of missing data was minimal. Continuous data were reported as means with standard deviation (SD), means with 95% confidence intervals (95% CI), or median with 25th percentile–75th percentile (P25–P75) and categorical data as numbers with percentages (%). Univariate comparison between the groups was done using a Student’s T test, Mann–Whitney U test, and chi-squared or Fisher’s exact test (as applicable). Costs of medical care were compared between the nonoperative and operative group using independent T test with bootstrap, drawing 1000 samples. We used bootstrap for the group comparisons to prevent outliers from affecting our conclusion on whether or not two groups were significantly different. Outliers are considered as potentially unreliable, as they are potentially caused by overreporting or underreporting healthcare use. The analyses were performed on a per-protocol basis. Despite the usual skewness in the distribution of costs, it is the arithmetic mean that is the most informative measure. Measures other than the arithmetic mean do not provide information about the cost of treating all patients, which are needed as the basis for healthcare policy decisions. Statistical analysis comparing medians using standard non-parametric methods may provide misleading conclusions [29]. As the utility scores were repeatedly measured over time, these were compared between treatment groups using linear mixed-effects regression models. The multilevel model included random effects for the intercepts of the model and time coefficient of individual patients. Since the outcome measures were not linearly related with time, the time points were entered as factor. The models included fixed effects for treatment group, age, gender, and ASA classification. The interaction between treatment group and time was included in the model to test for differences between the groups over time. For each follow-up moment, the estimated marginal mean with 95% confidence interval was computed per treatment group. Costs were reported in Euro and based on the currency exchange rate in July 22, 2021 (1 Euro = 1.155 US dollar).
Results
Out of the 172 enrolled patients, 88 (51%) patients opted for NOM and 84 (49%) for OM after SDM (Fig. 1). Patient characteristics did not significantly differ between the NOM and OM group. The median age of the study group was 88 years old (P25–P75 85–92), and most patients were female (76%). Patients were frail with a significant number of comorbidities and high level of pre-trauma activities of daily living dependence. Most patients suffered from cognitive impairment in both the NOM group (n = 83 (94%)) and in the OM group (n = 75 (89%)) (Table 1). Fracture type did not differ between the study groups (p = 0.301). The 6-month mortality rate was high (NOM; n = 83 (94%) and OM; n = 40 (48%)) (Fig. 1).
Costs and healthcare utilization
NOM was associated with significantly lower healthcare costs and healthcare utilization than OM in the first 6 months after injury (Table 2). The mean total costs per patient were €2425 for NOM and €9325 for OM (p < 0.001). The total costs of intramural hospital care were €2226 for NOM and €8630 for OM (p < 0.001).
Total costs per patient per day of survival were higher in the NOM group (€320, versus €227 in OM group, p = 0.024). A detailed overview of the costs is provided in Appendix Table 2.
The main cost drivers were costs of hospital stay €738 and €3140 for NOM and OM, respectively) and costs for surgical interventions in the OM group (€2783). The costs for hospital stay in the NOM group were significantly lower than in the OM group (p < 0.001), as only 49 patients (56%) of the NOM group were admitted to a hospital ward after ED presentation compared to 84 (100%) in the OM group. Furthermore, the median hospital length of stay was 2 days (P25–P75 2–3) in the NOM group and 6 days (P25–P75 4–7) in the OM group.
Additional healthcare consumption during the primary hospital stay was lower in nonoperatively managed patients with regards to diagnostic tests and consultations (Table 2). In the NOM group, for patients who were admitted to a ward, an average of 1.4 (SD 1.2, range 0–6) inpatient consultations by other specialists were requested. This was 1.6 (SD 1.3, range 0–7) in the OM group. In addition, 20 (22%) patients in the OM group required blood transfusions at an average cost of €110 per patient.
Mean costs for readmission due to adverse events in the OM group were €782. These costs were caused by 12 patients who were readmitted to the ED or hospital. The mean costs for hospital readmission for these 12 patients were €5477 (SD 4940) per patient. Five patients (6%) were re-operated due to surgery related adverse events at an average cost of €3066 (SD 996) per patient. None of the NOM patients were readmitted to the hospital during the study period.
Inclusion of costs of nursing home stay in the total costs increased the average costs per patient to €6796 in the NOM group and €30,246 in the OM group (p < 0.001, p < 0.001 with bootstrapping (Table 2)). The median duration of nursing home stay was 6 days (P25–P75 3–13) in the NOM group and 168 days (P25–P75 24–192) in the OM group. Mean costs of nursing home stay were € 4,371 for NOM and €20,925 for OM (p < 0.001). This comprised 66% and 69% of the total costs including nursing home stay for NOM and OM, respectively. The large difference was mainly caused by the shorter life expectancy (median time till death of 7 days (P25–P75 5–12) in the NOM group and 29 days (P25–P75 12–62) in the OM group). Total costs per patient per day of survival including nursing home stay was relatively higher in the NOM group (NOM; €453 (SD 213), OM; €375 (SD 249), p = 0.029).
Subgroup analysis
Total healthcare costs in the NOM group were higher for patients with an ASA class ≥ 4 (n = 29) than with an ASA class < 4 (n = 55) (€2927 vs 2,151, p = 0.001). This was mainly due to higher in-hospital costs (€2649 versus €1990). For NOM patients with ASA class ≥ 4, the costs of hospital stay were twofold for ASA ≥ 4 (€1116 vs €532, p = 0.001), 30% higher for laboratory tests (€139 vs €104, p = 0.001), and threefold for clinical consults (€66 vs €24, p ≤ 0.001). This statistical difference in total healthcare costs for the ASA classification was not found in the OM group (p = 0.402).
Costs excluding nursing home stay in the NOM or OM group did not differ for FAC ≤ 2 or higher, BMI < 18.5 or higher, or fracture type (femoral neck or trochanteric). Within the OM group, the mean costs for the surgical intervention were significantly higher for the femoral neck fractures (€2958) than the pertrochanteric fractures (€2581) for the primary surgery (p = 0.001).
For male patients in the OM group (n = 16), mean total healthcare costs were significantly higher (€6892) than for female patients (n = 68; €3218) (p = 0.039). When one male patient was excluded from this analysis (due to costs of €28,756), the statistical difference in costs of the primary hospital admission was no longer found (p = 0.378).
HRQoL and cost-effectiveness
The EQ5D utility scores are shown in Table 3. NOM lead to 0.01 (95% CI 0.01–0.02) QALYs, while OM resulted in 0.11 (95% CI 0.08–0.13) QALYs within the 6-month study period (p < 0.001). OM lead to a 0.10 increase in QALYs compared with NOM. With the total mean costs per patient for NOM being €2423 (95% CI €2200–€4648) and OM being €9322 (95% CI €8405–€10,238), the ICER per QALY gained in the OM versus NOM was €76,912 (95% CI 50.090–79,551) and therefore exceed the threshold of €20.000 per QALY.
The ICER for total costs per QALY for OM versus NOM group including nursing home stay was €248,395 (95% CI 221,362–282,000) and therefore even more exceeding the threshold of €20.000 per QALY. The ICER including nursing home stay was largely influenced by the longer life expectancy in the OM group that consequently increased the nursing home stay but with a limited gain in QALY.
No statistically significant differences were found within the NOM or OM group for QALYs based on ASA class ≥ 4 or lower, FAC ≤ 2 or higher, gender, BMI < 18.5, or higher or fracture type (femoral neck or trochanteric).
The QALYs gained for patients who died within 14 days after the injury between the NOM and OM group (NOM; 0.003 and OM 0.005, p < 0.001) were minimal, while mean total costs for NOM and OM were €2245 and €7823, respectively, were found. The same was found for patients who died within 30-day post-injury with NOM resulting in 0.003 QALYs and OM in 0.008 QALYs at the total costs of €2238 and €7957. For those who did not die within 30-day post-injury, NOM resulted in significantly lower QALY (0.056) than in the OM group (0.133) with p < 0.001 at total costs of €3333 and €9766, respectively.
Discussion
This study showed that the treatment of frail older institutionalized patients with a proximal femoral fracture results in significant healthcare costs. OM was associated with significantly more healthcare consumption and costs per patient than NOM (€9322 ($10,767) versus €2425 ($2,801)), mainly due to longer hospital stay, costs related to surgery, and costs due to readmissions.
The costs of nursing home stay were highly dependent on the differences in survival between both groups, as the NOM group had a shorter life expectancy. Although OM lead to a 0.10 increase in QALY compared to NOM, the ICER per QALY gained was €76,912 and therefore exceeded the costs per QALY limit of €20,000 according to the cost-utility norms of in the Netherlands [27]. Furthermore, this study showed that QALYs between the NOM and OM group in case patients died in the first month post-injury were minimal, but OM resulted in more than triple the costs.
Although the authors feel that decision-making on NOM or OM of the most frail older patients with a proximal femoral fracture should not be heavily influenced by costs, this study together with the results of the FRAIL-HIP study provides extra arguments that NOM should be openly discussed with frail patients who have pre-fracture limited life expectancy and QoL [16]. Because of the limited gain in QALY, patient selection of whom NOM should be seriously discussed with should only focus on those who have a short life expectancy after the proximal femoral fracture, as there was a clear gain in QALY in OM patients who survived more than 30 days compared to those who in the NOM group. Especially this category of patients can benefit from personalized shared decision-making as many factors, like frailty, HRQoL and QoL, pre-fracture mobility, and most important, the patient’s goals of care, have to be accounted for.
As all included patients were already residing in a nursing home prior to the fracture, it was chosen to mainly display the total costs without the costs of nursing home stay as the costs of nursing home stay were not additional healthcare costs. Furthermore, the costs of nursing home stay are mainly dependent on the life expectancy, as there was a distinct difference between the NOM and OM group. The costs of nursing home stay therefore would have less adequately reflected the true cost difference between the groups, but rather the differences in life expectancy. In case nursing home costs were included in the cost-utility analysis, the ICER increased to €248,395 (95% CI 221,362–282,000) per gained QALY.
The main cost drivers of the total hospital costs were the costs of ED visits and hospital admission (92% of total in the NOM and 84% in the OM group). These in-hospital costs of patients with an operatively treated proximal femoral fracture were comparable to previously published studies [19, 20, 30, 31]. Burgers et al. described Dutch patients with a proximal femoral fracture who were treated with an hemi-arthroplasty or total hip arthroplasty and found in-hospital associated costs of €9026 [20]. These slightly higher costs can be attributed to a higher number of patients undergoing expensive arthroplasties (100% versus 48% in the current study) and a longer hospital length of stay (9.9 (SD 5.2) days versus 6.6 (SD 6.6) days). The longer length of stay in the study of Burgers et al. can be explained by the possible additional waiting time for hospital discharge to an available rehabilitation center, as 56% of the patients were not discharged to their previous home. The in-hospital costs reported by Zielinski et al. were lower than in our study (€6031), but can be related to the fact that patients were less frail and were all treated with relatively cheaper internal fixation [19]. A meta-analysis by Williamson et al. also confirms that costs of hospitalization accounts for the majority of costs during the first year of follow-up and calculated mean pooled costs of hospitalization of $10,075 (95% CI $8832–$11,828) and total costs of $13,820 (SD $13,293) [30]. The lower mean total costs per operated patient in our study ($11,000) could be attributed to the more limited life expectancy.
Gu et al. are the only to report on direct medical costs of NOM. They reported mean total direct medical costs (including loss of productivity) of $40,795 and $34,509 for intra- and extracapsular proximal femoral fractures, respectively. [32] These costs significantly differed from our findings, as Gu et al. included non-frail patients with most likely rehabilitative goals or care, and not frail patients with a limited life expectancy in a more palliative care focused setting. For their cost estimation, they assumed that 50% of the patients could walk at the conclusion of the treatment, which is not a realistic expectation for our study population. Therefore, these costs cannot be compared.
Another cost driver in the OM group was costs of unplanned ED/hospital readmissions (8% of total costs). The costs of in-hospital adverse events could not be established based on the used dataset. Despite the occurrence of 64 adverse events within the OM group after their hospital discharge, only 12 patients (14%) revisited the ED within 6 months because of adverse events at a mean cost of €782 per person (SD 2636) for the total group. Remarkably, none of the patients in the NOM group were readmitted to the hospital. Compared with the 33% reported by Burgers et al. and 24% after 3 months reported by Lin et al. in nonagenarians, the number of readmissions of OM patients in our study was relatively low [20, 33]. This is arguably caused by the fact that some nursing home residents in our study were not hospitalized following adverse events (e.g., patients with hemiarthroplasty dislocation, wound infection, delirium, pneumonia, or fractures due to recurrent fall), as this was thought to be of no additional value for their QoL and/or did no longer match with the goals of care/patient’s preferences. Readmission to the hospital due to adverse events significantly affects the prognosis with a mortality risk in nonagenarians of 37% in 3 months. [33] Carefully re-evaluating patient goals of care and possible do-not-hospitalize directives in frail patients with a limited life expectancy could reduce additional costs in the case of an event with such a high impact as a proximal femoral fracture.
In case re-admission to the hospital for an adverse event is thought to be of no additional value for the patient’s quality of life, the costs reduction would be significant, as re-admission resulted in mean total costs of €5477 ($6326) per patient.
If it would be decided in the nursing home not to present a frail patient to the hospital and thus manage the patient nonoperatively, a significant cost reduction of approximately €2200 ($2,541) per patient could be achieved without altering the care received. In case a 25–50% reduction of ED admissions in 5% out of 20,000 annual NOM patients with a proximal femoral fracture in the Netherlands, a yearly cost reduction of approximately €1.1–2.2 million could be achieved. This emphasizes the importance of advance care planning in long-term care facilities.
Some limitations of the current study need to be mentioned. First, the costs for equipment and implants were derived from previous studies. Costs for the surgical intervention could be an under- or overestimation depending on local price agreements and choice of implants. Secondly, the type and organization of health care may vary (inter)nationally. Extrapolation of the study results to other healthcare systems should therefore be performed with caution. The Netherlands, for example, has expert nursing homes with in-house rehabilitation led by elderly care physicians who are dedicated to provide long-term care in these long-term care facilities. Consequently, additional costs for in-house rehabilitation of patients who already resided in a nursing home were difficult to establish other than visits from physiotherapists and additional medication. Thirdly, costs of nursing home stay could not be adjusted for changes in the intensity of care packages (ZZP). Finally, the variability in limited life expectancy in the operative group of this study resulted in large variation of total healthcare costs, as is reflected by the high standard deviations. However, this does reflect the current practice and heterogeneity is also seen in previous literature [30]. In addition, the ICER is dependent on the duration of follow-up, as most direct medical costs are made in the first weeks after the trauma. The chosen 6-month time frame is a limitation. A longer study period would likely increase the QALY in the operative group and therefore improve cost-effectiveness. However, the 6-month time frame for follow-up was mainly chosen due to limited life expectancy of the nonoperative patients and that the most functional recovery occurs within the first 3- to 6-month post-trauma.
With these limitations in mind, this study further adds to the evidence on important cost drivers for proximal femoral fracture patients. In addition, to our knowledge, this is the first cost-utility analysis on nonoperative and operative treatment of patients with frail proximal femoral fractures with a limited life expectancy. In the FRAIL-HIP study, we showed that, after SDM, nonoperative treatment of proximal femoral fractures is a viable, non-inferior treatment option to operative management in patients with a limited life expectancy, [16] where this studies shows that in this specific group of patients, there is limited gain in QALY and OM exceeds the Dutch threshold of €20,000 per gained QALY according to economic guidelines. This shows that both NOM and OM should be openly discussed with SDM in frail patients with a limited life expectancy who sustain a proximal femoral fracture while accounting for many factors.
Conclusion
Management of frail institutionalized older patients with a proximal femoral fracture is associated with significant healthcare utilization and healthcare costs. The mean total healthcare costs per person of NOM and OM were €2425 and €9322, respectively. The main cost driver was hospital admission. The ICER of total costs per QALY from operative treatment was €76,912 and exceeded the threshold of €20,000 per QALY. For frail patients at the end of life, NOM of proximal femoral fractures should be openly discussed in SDM conversations. Cost reduction could potentially be achieved via advance care planning in long-term care facilities by consequently reducing ED admissions if patients decide on NOM in their nursing home.
Data sharing
Relevant anonymized data on individual patients for meta-analysis purposes can be provided upon reasonable request to the principal investigator.
Change history
17 January 2023
A Correction to this paper has been published: https://doi.org/10.1007/s00198-023-06673-2
References
Cooper C, Campion G, Melton LJ 3rd (1992) Hip fractures in the elderly: a world-wide projection. Osteoporos Int 2(6):285–289
Gullberg B, Johnell O, Kanis JA (1997) World-wide projections for hip fracture. Osteoporos Int 7(5):407–413
Johnell O (1997) The socioeconomic burden of fractures: today and in the 21st century. Am J Med 103(2A):20S-5S; discussion 5S-6S.
Berry SD, Lee Y, Zullo AR, Kiel DP, Dosa D, Mor V (2016) Incidence of hip fracture in U.S. nursing homes. J Gerontol A Biol Sci Med Sci 71(9):1230–4
Crotty M, Miller M, Whitehead C, Krishnan J, Hearn T (2000) Hip fracture treatments–what happens to patients from residential care? J Qual Clin Pract 20(4):167–170
Beaupre LA, Cinats JG, Jones CA, Scharfenberger AV, William CJD, Senthilselvan A et al (2007) Does functional recovery in elderly hip fracture patients differ between patients admitted from long-term care and the community? J Gerontol A Biol Sci Med Sci 62(10):1127–1133
Berry SD, Rothbaum RR, Kiel DP, Lee Y, Mitchell SL (2018) Association of clinical outcomes with surgical repair of hip fracture vs nonsurgical management in nursing home residents with advanced dementia. JAMA Intern Med 178(6):774–780
van de Ree CLP, De Jongh MAC, Peeters CMM, de Munter L, Roukema JA, Gosens T (2017) Hip fractures in elderly people: surgery or no surgery? A systematic review and meta-analysis. Geriatr Orthop Surg Rehabil 8(3):173–180
Joosse P, Loggers SAI, Van de Ree C, Van Balen R, Steens J, Zuurmond RG et al (2019) The value of nonoperative versus operative treatment of frail institutionalized elderly patients with a proximal femoral fracture in the shade of life (FRAIL-HIP); protocol for a multicenter observational cohort study. BMC Geriatr 19(1):301
NICE. Hip Fracture management [Available from: www.nice.org.uk/guidance/cg1242014]. last Accessed 05–04–2020
Federatie Medisch Specialisten, Richtlijn Generieke zorgpad bij de behandeling van kwetsbare ouderen rondom chirurgische ingrepen NVKG [Available from: https://richtlijnendatabase.nl/richtlijn/behandeling_kwetsbare_ouderen_bij_chirurgie/generieke_zorgpad.html]. last Accessed 05–04–2020
Cram P, Yan L, Bohm E, Kuzyk P, Lix LM, Morin SN et al (2017) Trends in operative and nonoperative hip fracture management 1990–2014: a longitudinal analysis of Manitoba administrative data. J Am Geriatr Soc 65(1):27–34
Dutch Hip Fracture Audit, Jaarrapportage 2019, [Available from: https://dica.nl/jaarrapportage-2019/dhfa]. Last accessed 250–06–2021
Beaupre LA, Lier D, Magaziner JS, Jones CA, Johnston DWC, Wilson DM et al (2020) An outreach rehabilitation program for nursing home residents after hip fracture may be cost-saving. J Gerontol A Biol Sci Med Sci 75(10):e159–e165
Heinrich S, Rapp K, Rissmann U, Becker C, Konig HH (2011) Service use and costs of incident femoral fractures in nursing home residents in Germany: the Bavarian fall and fracture prevention project (BF2P2). J Am Med Dir Assoc 12(6):459–466
Loggers SAI, Willems HC, Van Balen R, Gosens T, Polinder S, Ponsen KJ et al (2022) Evaluation of quality of life after nonoperative or operative management of proximal femoral fractures in frail institutionalized patients: the FRAIL-HIP study. JAMA Surg 157(5):424–434
Brooks RR, RE Eds, DC (2003) The measurement and valuation of health status using EQ-5D: a European perspective. Europe: Kluwer Academic Publishers
Bouwmans CHRL, Koopmanschap M. Guideline iMTA Medical Cost Questionnaire (iMCQ). Rotterdam: iMTA. Erasmus University Rotterdam
Zielinski SM, Bouwmans CA, Heetveld MJ, Bhandari M, Patka P, Van Lieshout EM et al (2014) The societal costs of femoral neck fracture patients treated with internal fixation. Osteoporos Int 25(3):875–885
Burgers PT, Hoogendoorn M, Van Woensel EA, Poolman RW, Bhandari M, Patka P et al (2016) Total medical costs of treating femoral neck fracture patients with hemi- or total hip arthroplasty: a cost analysis of a multicenter prospective study. Osteoporos Int 27(6):1999–2008
Hakkaart-van Roijen LLN, Bouwmans C, Kanters T, Tan SS (2016) Van goede zorg verzekerd, BIJLAGE 1: Kostenhandleiding: Methodologie van kostenonderzoek en referentieprijzen voor economische evaluatie in de gezondheidszorg
Nederlandse zorgautoriteit (Dutch Healthcare Authority), Tariefbeschikking Eerstelijnsdiagnostiek 2014,[Available from: https://puc.overheid.nl/doc/PUC_5720_22]. Last accessed 15–02–2021
College voor Zorgverzekeringen (Health Care Insurance Board), Medicijnkosten, [available from: www.medicijnkosten.nl]. Last accessed on 25–04–2021
Neugebauer E, Bouillon B, Bullinger M, Wood-Dauphinee S (2002) Quality of life after multiple trauma–summary and recommendations of the consensus conference. Restor Neurol Neurosci 20(3–4):161–167
Tol M, Kuipers JP, Willigenburg NW, Willems HC, Poolman RW (2021) How are you doing in the eyes of your spouse? Level of agreement between the self-completed EQ-5D-5L and two proxy perspectives in an orthopaedic population: a randomized agreement study. Health Qual Life Outcomes 19(1):35
Lamers LM, Stalmeier PF, McDonnell J, Krabbe PF, van Busschbach JJ (2005) [Measuring the quality of life in economic evaluations: the Dutch EQ-5D tariff] Kwaliteit van leven meten in economische evaluaties: het Nederlands EQ-5D-tarief. Ned Tijdschr Geneeskd 149(28):1574-8.
Zorginstituut Nederland (National Healthcare Insitutute of The Netherlands). De theorie en praktijk van het berekenen van ziektelast bij pakketbeoordelingen 2018 [Available from: https://www.zorginstituutnederland.nl/binaries/zinl/documenten/rapport/2018/05/07/ziektelast-in-de-praktijk/Ziektelast+in+de+praktijk_definitief.pdf]. Last accessed 04–05–2020
von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP et al (2007) The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet 370(9596):1453–1457
Thompson SG, Barber JA (2000) How should cost data in pragmatic randomised trials be analysed? BMJ 320(7243):1197–1200
Williamson S, Landeiro F, McConnell T, Fulford-Smith L, Javaid MK, Judge A et al (2017) Costs of fragility hip fractures globally: a systematic review and meta-regression analysis. Osteoporos Int 28(10):2791–2800
Haentjens P, Autier P, Barette M, Boonen S, Belgian Hip Fracture Study G (2001) The economic cost of hip fractures among elderly women. A one-year, prospective, observational cohort study with matched-pair analysis. Belgian Hip Fracture Study Group. J Bone Joint Surg Am 83(4):493–500
Gu Q, Koenig L, Mather RC 3rd, Tongue J (2014) Surgery for hip fracture yields societal benefits that exceed the direct medical costs. Clin Orthop Relat Res 472(11):3536–3546
Lin JC, Liang WM (2017) Mortality, readmission, and reoperation after hip fracture in nonagenarians. BMC Musculoskelet Disord 18(1):144
Acknowledgements
We would like to acknowledge the societies for surgery; Dutch Association for Surgery (NVvH), Dutch Association for Trauma Surgery (NVT), Dutch Orthopedic Association (NOV), Dutch Association for Orthopedic Trauma Surgery (NVOT)), clinical geriatrics (Dutch Association for Clinical Geriatrics (NVKG)), elderly care (Association of Elderly Care Physicians (VERENSO)), and the Dutch Patient Federation for their support. Furthermore, we would like to acknowledge all the participating staff and physicians in the nursing homes for the collaboration and support with the data curation.
Funding
This study was funded by the Netherlands Organization for Health Research and Development (ZonMw; ref.nr. 843004120) and Osteosynthesis and Trauma Care Foundation (ref.nr. 2019-PJKP); no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; and no other relationships or activities that could appear to have influenced the submitted work.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Ethical approval
This study has been exempted by the Medical Research Ethics Committee (MREC) of VU University Medical Center according to article 7 of the Medical Research Involving Human Subjects Act (ref.no. 2018.208). All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Supplementary information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Loggers, S.A.I., Geraerds, A.J.L.M., Joosse, P. et al. Nonoperative versus operative management of frail institutionalized older patients with a proximal femoral fracture: a cost-utility analysis alongside a multicenter prospective cohort study. Osteoporos Int 34, 515–525 (2023). https://doi.org/10.1007/s00198-022-06638-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06638-x