Abstract
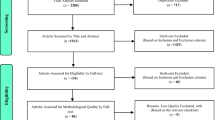
This systematic review and meta-analysis estimated the global, regional prevalence, and risk factors of osteoporosis. Prevalence varied greatly according to countries (from 4.1% in Netherlands to 52.0% in Turkey) and continents (from 8.0% in Oceania to 26.9% in Africa). Osteoporosis is a common metabolic bone disorder in the elderly, usually resulting in bone pain and an increased risk of fragility fracture, but few summarized studies have guided global strategies for the disease. Therefore, we pooled the epidemiologic data to estimate the global, regional prevalence, and potential risk factors of osteoporosis. We conducted a comprehensive literature search through PubMed, EMBASE, Web of Science, and Scopus, to identify population-based studies that reported the prevalence of osteoporosis based on the World Health Organization (WHO) criteria. Meta-regression and subgroup analyses were used to explore the sources of heterogeneity. The study was registered in the PROSPERO database (CRD42021285555). Of the 57,933 citations evaluated, 108 individual studies containing 343,704 subjects were included. The global prevalence of osteoporosis and osteopenia was 19.7% (95%CI, 18.0%–21.4%) and 40.4% (95%CI, 36.9%–43.8%). Prevalence varied greatly according to countries (from 4.1% in Netherlands to 52.0% in Turkey) and continents (from Oceania 8.0% to 26.9% in Africa). The prevalence was higher in developing countries (22.1%, 95%CI, 20.1%–24.1%) than in developed countries (14.5%, 95%CI, 11.5%–17.7%). Our study indicates a considerable prevalence of osteoporosis among the general population based on WHO criteria, and the prevalence varies substantially between countries and regions. Future studies with robust evidence are required to explore risk factors to provide effective preventive strategies for the disease.




Similar content being viewed by others
Data availability
The data that supports the findings of this study are available in the supplementary material of this article.
Code availability
Not applicable.
References
Johnell O, Kanis JA (2006) An estimate of the worldwide prevalence and disability associated with osteoporotic fractures. Osteoporos Int 17:1726-33. https://doi.org/10.1007/s00198-006-0172-4
Hernlund E, Svedbom A, Ivergård M et al. (2013) Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteopor 8:136. https://doi.org/10.1007/s11657-013-0136-1
Gourlay ML, Brown SA (2004) Clinical considerations in premenopausal osteoporosis. Arch Internal Med 164:603-14. https://doi.org/10.1001/archinte.164.6.603
Cummings SR, Melton LJ (2002) Epidemiology and outcomes of osteoporotic fractures. Lancet (London, England) 359:1761-7. https://doi.org/10.1016/s0140-6736(02)08657-9
Si L, Winzenberg TM, Jiang Q, Chen M, Palmer AJ (2015) Projection of osteoporosis-related fractures and costs in China: 2010-2050. Osteoporos Int 26:1929-37. https://doi.org/10.1007/s00198-015-3093-2
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet (London, England) 359:1929-36. https://doi.org/10.1016/s0140-6736(02)08761-5
Blake GM, Fogelman I (2001) Peripheral or central densitometry: does it matter which technique we use? J Clin Densitometry 4:83-96. https://doi.org/10.1385/jcd:4:2:083
Gerber LM, Bener A, Al-Ali HM, Hammoudeh M, Liu LQ, Verjee M (2015) Bone mineral density in midlife women: the Study of Women's Health in Qatar. Climacteric 18:316-22. https://doi.org/10.3109/13697137.2014.944495
Bakir MA, Hammad KB, Habil KM (2018) Bone mineral density in healthy Syrian women measured by dual energy X-ray absorptiometry. https://doi.org/10.2478/anre-2018-0002
Marwaha RK, Tandon N, Garg MK, Kanwar R, Bhadra K (2010) Bone health in healthy Indian population aged 50 years and above. Osteoporos Int 21:S690–S691. https://doi.org/10.1007/s00198-010-1433-9
Mahussain S, Badr H, Al-Zaabi K, Mohammad M, Alnafisi N (2006) Bone mineral density in healthy Kuwaiti women. Arch Osteoporos 1:51-57. https://doi.org/10.1007/s11657-006-0008-z
Zhang Z-L, Qin Y-J, Huang Q-R et al. (2006) Bone mineral density of the spine and femur in healthy Chinese men. Asian J Androl 8:419-427. https://doi.org/10.1111/j.1745-7262.2006.00170.x
Choi YJ, Oh HJ, Kim DJ, Lee Y, Chung Y-S (2012) The prevalence of osteoporosis in Korean adults aged 50 years or older and the higher diagnosis rates in women who were beneficiaries of a national screening program: The Korea National Health and Nutrition Examination Survey 2008-2009. J Bone Miner Res 27:1879-1886. https://doi.org/10.1002/jbmr.1635
Aggarwal A, Pal R, Bhadada SK et al. (2012) Bone mineral density in healthy adult Indian population: the Chandigarh Urban Bone Epidemiological Study (CUBES). Arch Osteoporos 16:17. https://doi.org/10.1007/s11657-020-00868-4
Fahimfar N, Noorali S, Yousefi S et al. (2021) Prevalence of osteoporosis among the elderly population of Iran. Arch Osteoporos 16:16. https://doi.org/10.1007/s11657-020-00872-8
Olmos JM, Hernández JL, Martínez J et al. (2018) Prevalence of vertebral fracture and densitometric osteoporosis in Spanish adult men: The Camargo Cohort Study. J Bone Miner Metabol 36:103-110. https://doi.org/10.1007/s00774-017-0812-0
Looker AC, Sarafrazi Isfahani N, Fan B, Shepherd JA (2017) Trends in osteoporosis and low bone mass in older US adults, 2005–2006 through 2013–2014. Osteoporos Int 28:1979-1988. https://doi.org/10.1007/s00198-017-3996-1
Zeng Q, Li N, Wang Q et al. (2019) The Prevalence of Osteoporosis in China, a Nationwide, Multicenter DXA Survey. J Bone Miner Res 34:1789-1797. https://doi.org/10.1002/jbmr.3757
Zamani M, Zamani V, Heidari B, Parsian H, Esmaeilnejad-Ganji SM (2018) Prevalence of osteoporosis with the World Health Organization diagnostic criteria in the Eastern Mediterranean Region: a systematic review and meta-analysis. Arch Osteoporos 13:129. https://doi.org/10.1007/s11657-018-0540-7
Salari N, Ghasemi H, Mohammadi L et al. (2021) The global prevalence of osteoporosis in the world: a comprehensive systematic review and meta-analysis. J Orthop Surg ResJ Orthop Surg Res 16:609. https://doi.org/10.1186/s13018-021-02772-0
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ (Clinical research ed);2009;339:b2535. https://doi.org/10.1136/bmj.b2535
Kanis JA, Melton LJ, 3rd, Christiansen C, Johnston CC, Khaltaev N (1994) The diagnosis of osteoporosis. J Bone Miner 9:1137-41. https://doi.org/10.1002/jbmr.5650090802
Hoy D, Brooks P, Woolf A et al. (2012) Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol 65:934-9. https://doi.org/10.1016/j.jclinepi.2011.11.014
Peters JL, Sutton AJ, Jones DR, Abrams KR, Rushton L (2006) Comparison of two methods to detect publication bias in meta-analysis. Jama 295:676-80. https://doi.org/10.1001/jama.295.6.676
Tobias JH, Cook DG, Chambers TJ, Dalzell N (1994) A comparison of bone mineral density between Caucasian, Asian and Afro-Caribbean women. Clin Sci (London, England : 1979) 87:587-91. https://doi.org/10.1042/cs0870587
del Rio Barquero L, Romera Baures M, Pavia Segura J et al. (1992) Bone mineral density in two different socio-economic population groups. Bone Miner 18:159-68. https://doi.org/10.1016/0169-6009(92)90856-9
Paruk F, Tsabasvi M, Kalla AA (2021) Osteoporosis in Africa-where are we now. Clin Rheumatol 40:3419-3428. https://doi.org/10.1007/s10067-020-05335-6
Xiao PL, Hsu CJ, Ma YG et al. (2022) Prevalence and treatment rate of osteoporosis in patients undergoing total knee and hip arthroplasty: a systematic review and meta-analysis. Arch Osteoporos 17:16. https://doi.org/10.1007/s11657-021-01055-9
Lo JC, Chandra M, Lee C, Darbinian JA, Ramaswamy M, Ettinger B (2020) Bone Mineral Density in Older U.S. Filipino, Chinese, Japanese, and White Women. J Am Geriatr Soc 68:2656-2661. https://doi.org/10.1111/jgs.16785
Roy D, Swarbrick C, King Y et al. (2005) Differences in peak bone mass in women of European and South Asian origin can be explained by differences in body size. Osteoporos Int 16:1254-62. https://doi.org/10.1007/s00198-005-1837-0
Maalouf G, Salem S, Sandid M et al. (2000) Bone mineral density of the Lebanese reference population. Osteoporos Int 11:756-64. https://doi.org/10.1007/s001980070054
Jiang Z, Pu R, Li N et al. (2021) High prevalence of vitamin D deficiency in Asia: A systematic review and meta-analysis. Crit Rev Food Sci Nutr:1-10. https://doi.org/10.1080/10408398.2021.1990850
Du Y, Zhao LJ, Xu Q, Wu KH, Deng HW (2017) Socioeconomic status and bone mineral density in adults by race/ethnicity and gender: the Louisiana osteoporosis study. Osteoporos Int 28:1699-1709. https://doi.org/10.1007/s00198-017-3951-1
Schousboe JT, Shepherd JA, Bilezikian JP, Baim S (2013) Executive summary of the 2013 International Society for Clinical Densitometry Position Development Conference on bone densitometry. J Clin Densitometry 16:455-66. https://doi.org/10.1016/j.jocd.2013.08.004
Moayyeri A, Soltani A, Tabari NK, Sadatsafavi M, Hossein-Neghad A, Larijani B (2005) Discordance in diagnosis of osteoporosis using spine and hip bone densitometry. BMC Endocr Disord 5:3. https://doi.org/10.1186/1472-6823-5-3
Mounach A, Abayi DA, Ghazi M et al. (2009) Discordance between hip and spine bone mineral density measurement using DXA: prevalence and risk factors. Semin Arthrit Rheumat 38:467-71. https://doi.org/10.1016/j.semarthrit.2008.04.001
Lane NE (2006) Epidemiology, etiology, and diagnosis of osteoporosis. Am J Obstetr Gynecol 194:S3-11. https://doi.org/10.1016/j.ajog.2005.08.047
Aaron JE, Johnson DR, Paxton S, Kanis JA (1989) Secondary osteoporosis and the microanatomy of trabecular bone. Clin Rheumatol 8 Suppl 2:84-8. https://doi.org/10.1007/bf02207240
Kohrt WM, Snead DB, Slatopolsky E, Birge SJ, Jr (1995) Additive effects of weight-bearing exercise and estrogen on bone mineral density in older women. J Bone Miner Res 10:1303-11. https://doi.org/10.1002/jbmr.5650100906
Hamdy RC, Petak SM, Lenchik L (2002) Which central dual X-ray absorptiometry skeletal sites and regions of interest should be used to determine the diagnosis of osteoporosis? J Clin Densitometry 5 Suppl:S11-8. https://doi.org/10.1385/jcd:5:3s:s11
Chen P, Li Z, Hu Y (2016) Prevalence of osteoporosis in China: a meta-analysis and systematic review. BMC Publ Health 16:1039. https://doi.org/10.1186/s12889-016-3712-7
Holm JP, Hyldstrup L, Jensen JB (2016) Time trends in osteoporosis risk factor profiles: a comparative analysis of risk factors, comorbidities, and medications over twelve years. Endocrine 54:241-255. https://doi.org/10.1007/s12020-016-0987-5
De Laet C, Kanis JA, Odén A et al. (2005) Body mass index as a predictor of fracture risk: a meta-analysis. Osteoporos Int 16:1330-8. https://doi.org/10.1007/s00198-005-1863-y
Allali F, Rostom S, Bennani L, Abouqal R, Hajjaj-Hassouni N (2010) Educational level and osteoporosis risk in postmenopausal Moroccan women: A classification tree analysis. Clin Rheumatol 29:1269-1275. https://doi.org/10.1007/s10067-010-1535-y
Ho SC, Chen YM, Woo JL (2005) Educational level and osteoporosis risk in postmenopausal Chinese women. Am J Epidemiol 161:680-90. https://doi.org/10.1093/aje/kwi047
Li H, Wallin M, Barregard L et al. (2020) Smoking-Induced Risk of Osteoporosis Is Partly Mediated by Cadmium From Tobacco Smoke: The MrOS Sweden Study. J Bone Miner Res 35:1424-1429. https://doi.org/10.1002/jbmr.4014
Parizad N, Baghi V, Karimi EB, Ghanei Gheshlagh R (2019) The prevalence of osteoporosis among Iranian postmenopausal women with type 2 diabetes: A systematic review and meta-analysis. Diab Metabol Synd 13:2607-2612. https://doi.org/10.1016/j.dsx.2019.07.036
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes--a meta-analysis. Osteoporos Int 18:427-44. https://doi.org/10.1007/s00198-006-0253-4
Agius R, Galea R, Fava S (2016) Bone mineral density and intervertebral disc height in type 2 diabetes. J Diab Complic 30:644-50. https://doi.org/10.1016/j.jdiacomp.2016.01.021
Richards JB, Zheng HF, Spector TD (2012) Genetics of osteoporosis from genome-wide association studies: advances and challenges. Nat Rev Genet 13:576-88. https://doi.org/10.1038/nrg3228
Funding
This study was supported by grants from the National Natural Science Foundation of China (NO. 81772384 and 81902242).
Author information
Authors and Affiliations
Contributions
Conceptualization, Pei-Lun Xiao, Ai-Yong Cui, and Hua-Ding Lu; Data curation, Pei-Lun Xiao and Ai-Yong Cui; Formal analysis, Pei-Lun Xiao, Xiang-He Xu, Ai-Yong Cui, Chi-Jen Hsu, and Hua-Ding Lu; Investigation, Pei-Lun Xiao, Chi-Jen Hsu, and Yong-Guang Ma; Methodology, Pei-Lun Xiao, Xiang-He Xu, and Hua-Ding Lu; Project administration, Pei-Lun Xiao, Xiang-He Xu, and Hua-Ding Lu; Software, Pei-Lun Xiao, Yong-Guang Ma, and Hua-Ding Lu; Visualization, Pei-Lun Xiao, Ding-Liu, and Rong-Peng; Writing—original draft, Pei-Lun Xiao, Rong -Peng, and Hua-Ding Lu; Writing—review & editing, Pei-Lun Xiao, Xiang-He Xu, Ning-Jiang, and Hua-Ding Lu.
Corresponding authors
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable
Conflicts of interest
Pei-Lun Xiao, Ai-Yong Cui, Chi-Jen Hsu, Rong-Peng, Ning-Jiang, Xiang-He Xu, Yong-Guang Ma, Ding-Liu and Hua-Ding Lu declare that they have no conflict of interest.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Xiao, PL., Cui, AY., Hsu, CJ. et al. Global, regional prevalence, and risk factors of osteoporosis according to the World Health Organization diagnostic criteria: a systematic review and meta-analysis. Osteoporos Int 33, 2137–2153 (2022). https://doi.org/10.1007/s00198-022-06454-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06454-3