Abstract
Summary
In pre- and early perimenopausal women, prediabetes (with blood glucose ≥ 110 mg/dL) and greater insulin resistance are associated with worse trabecular bone quality (as assessed by trabecular bone score).
Purpose
Diabetes mellitus (DM) is associated with lower trabecular bone score (TBS) and fracture; less certain is whether the precursor states of prediabetes and increased insulin resistance are also related to adverse bone outcomes. We examined, in women who do not have DM, the associations of glycemic status (prediabetes vs. normal) and insulin resistance with TBS.
Methods
This was a cross-sectional analysis of baseline data collected from 42- to 52-year-old, pre- and perimenopausal participants in the Study of Women’s Health Across the Nation (SWAN) TBS Study. Women with prediabetes were categorized as having either high prediabetes if their fasting glucose was between 110 and 125 mg/dL or low prediabetes if their fasting glucose was between 100 and 109 mg/dL. Normoglycemia was defined as a fasting glucose below 100 mg/dL.
Results
In multivariable linear regression, adjusted for age, race/ethnicity, menopause transition stage, cigarette use, calcium and vitamin D supplementation, lumbar spine bone mineral density, and study site, women with high prediabetes had 0.21 (p < 0.0001) standard deviations (SD) lower TBS than those with normoglycemia. Low prediabetes was not associated with lower TBS. When HOMA-IR levels were ≥ 1.62, each doubling of HOMA-IR was associated with a 0.11 SD decrement in TBS (p = 0.0001).
Conclusion
Similar to diabetics, high prediabetics have lower TBS than normoglycemic individuals. Women with greater insulin resistance have lower TBS even in the absence of DM. Future studies should examine the associations of high prediabetes and insulin resistance with incident fracture.
Similar content being viewed by others
Introduction
There is mounting recognition that “diabetic bone disease” [1] and fractures are end-organ complications of diabetes mellitus (DM) [2,3,4,5]. Although DM is often associated with higher bone mineral density (BMD) [5], one critical feature of diabetic bone disease is diminished bone quality [1]. One bone quality parameter that is altered in DM is trabecular microarchitecture, which can be indirectly assessed using trabecular bone score (TBS). TBS is a textural parameter derived from DXA-based lumbar spine (LS) images and correlates with HR-qQCT measurements of trabecular microstructure [6]. Indeed, the pathophysiologic importance of impaired trabecular microarchitecture in diabetic bone disease is supported by studies showing that TBS is lower in diabetics versus non-diabetics [7,8,9,10,11,12,13], and in persons with DM, lower TBS predicts fracture risk independent of BMD [8, 14].
Although the negative relation between DM and trabecular microarchitecture is well-studied [7,8,9,10,11,12,13], whether prediabetes is similarly associated with lower TBS is less certain [10, 11, 15]. This knowledge is important because it could shed light on whether prediabetes has clinical implications beyond increased risk for developing DM. Clinicians disagree on how aggressively to treat prediabetes [16, 17], in part, because not every prediabetic develops diabetes, and prediabetes on its own has not been definitively linked to end-organ complications. To address this knowledge gap, we set out to determine if prediabetes is associated with lower TBS. Because a rise in insulin resistance precedes the onset of prediabetes and DM, our second objective was to examine whether greater insulin resistance is related to lower TBS, even in the absence of DM.
To accomplish our objectives, we conducted a cross-sectional analysis of participants in the Trabecular Bone Score (TBS) Study, which was done as part of the Study of Women’s Health Across the Nation (SWAN). SWAN is a cohort study of the menopause transition in a multi-racial/ethnic community sample. For this analysis, we used data from the SWAN TBS Study baseline visit, at which time participants were between 42 and 52 years.
Methods
SWAN is a multi-center, longitudinal study of 3,302 diverse, community-dwelling women. At study inception, participants were between 42 and 52 years, and in premenopause (no change from usual menstrual bleeding) or early perimenopause (less predictable menstrual bleeding at least once every three months). Potential volunteers were excluded if they did not have an intact uterus and at least one ovary or were using sex steroid hormones. A total of seven clinical sites recruited study participants: Boston, Chicago, Detroit, Pittsburgh, Los Angeles, Newark, and Oakland. The SWAN Bone Cohort was composed of 2,407 women from five sites (excludes Chicago and Newark, where BMD assessments were not performed). In turn, the SWAN TBS Study included 1,436 women from three Bone Cohort sites (Boston, Detroit, and Los Angeles). Pittsburgh and Oakland were not TBS Study sites because TBS could not be measured using scans acquired from their older DXA machines. Participants provided written informed consent, and each site obtained institutional review board approval.
Samples
Of the 1,436 women from the SWAN TBS Study, we excluded those who reported taking either bone-beneficial medications (hormone therapy, calcitonin, calcitriol, bisphosphonates, denosumab, or parathyroid hormone) or bone-detrimental medications (oral or injectable glucocorticoids, aromatase inhibitors, gonadotropin releasing hormone agonists, or anti-epileptic medications) at the time of the first TBS measurement (N = 61), women with DM (fasting glucose ≥ 126 mg/dL, or use of DM medications [metformin, sulfonylurea, meglitinide, thiazolidinedione, DPP-IV inhibitor, GLP-agonist, insulin]) (N = 70) and those for whom HOMA-IR could not be calculated (N = 58). This left us with a sample of 1,248 women.
Outcomes
The outcome in analyses was TBS, a textural parameter derived from lumbar spine (LS) BMD scans. SWAN TBS Study sites measured LS BMD using Hologic 4500A instruments. For the LS region of interest, vertebrae were excluded if local structural change or artifact was visualized. In addition, anatomically abnormal vertebrae were removed if there was a > 1.0 T-score difference between the vertebra in question and adjacent vertebrae. A standard BMD quality-control program, conducted in collaboration with Synarc, Inc. (Newark, CA), included daily phantom measurements, SWAN site cross-calibration with a circulating anthropomorphic spine standard, local site review of all scans, and central review of scans that met problem-flagging criteria.
The SWAN TBS Study baseline data consists of TBS values calculated from the first available LS BMD from SWAN baseline through follow-up visit 3. The study used thickness-corrected TBS (Med-Imaps, Pessac, France), which corrects for errors due to overlying soft tissue, by using direct measures of thickness by DXA. Earlier versions of Med-Imaps software (iNsight v3.0 and older) used BMI as a surrogate for soft tissue thickness to estimate the soft-tissue correction. This led to a residual negative correlation between BMI and earlier TBS estimates on scans acquired using Hologic densitometers [18]. One validation study of TBS corrected for directly measured soft tissue thickness reported no correlation between BMI and TBS [19]. The SWAN TBS study confirmed that there was no correlation between BMI and TBS for BMI in the middle range, 24 to 31 kg/m2. However, there was a positive correlation for BMI < 24 kg/m2 and negative correlation when BMI was greater than 31 kg/m2 [20]. We therefore accounted for BMI in analyses using splines (see the “Data analysis” section).
Primary exposures
For our first analysis, the primary exposure was glycemic status (prediabetes vs. normal fasting glucose), determined from blood glucose measured from a fasting morning draw, and medication use determined by an inventory of pill bottles brought by the participant to the study visit. Serum glucose was measured using a hexokinase-coupled reaction (Roche Molecular Biochemicals Diagnostics, Indianapolis, IN). Prediabetes was defined as a fasting glucose ≥ 100 and ≤ 125 mg/dL without use of DM medications. For our analyses, we divided prediabetics into 2 groups, low prediabetes (those with fasting glucose 100–109 mg/dL), and high prediabetes (those with fasting glucose 110–125 mg/dL). We made this distinction based on prior data that fasting glucose levels ≥ 110 mg/dL, specifically, are associated with adverse health markers [21, 22]. Participants that did not fall into either low or high prediabetes categories were defined as normoglycemic.
The primary exposure for the second analysis was insulin resistance, as assessed by HOMA-IR, calculated as fasting blood glucose (mg/dL) times fasting serum insulin (U/mL) divided by the constant 405. Insulin was measured from the same fasting blood sample as glucose. Serum insulin was measured using a radioimmunoassay (Coat-a-Count; Diagnostic Products Corp., Los Angeles, CA). The quality control program for serum insulin in SWAN has been previously described [23].
Covariates
Factors that could impact the TBS outcome were included as covariates in analyses. These included self-reported age (years), race/ethnicity, menopause transition (MT) stage (premenopause [no change in menstrual bleeding] vs. perimenopause [less predictable menstrual bleeding at least once every 12 months]), supplemental vitamin D use (yes/no), supplemental calcium use (yes/no), cigarette use (yes/no), and BMI calculated from measured height and weight.
Our fully adjusted models also included lumbar spine (LS) BMD as a covariate. DXA estimates LS BMD by quantifying the average gray-level over all pixels within the LS image region of interest, and TBS indexes the variation in gray-level between pixels in the same region [6]. In SWAN, there was a positive, biphasic relation between LS BMD and TBS with an inflection point at a BMD value of 1.080 g/cm2 (more positive before, less positive after). We, therefore, accounted for LS BMD in analyses using splines (see the “Data analysis” section). Conceptually, controlling for BMD permits us to quantify the associations of glycemic status or insulin resistance with variation in pixel gray-level (TBS) for a given amount of average gray-level (BMD). Prior studies confirm that adjusting for BMD strengthens the association between DM and TBS [8].
Data analysis
In our first analysis, we examined the association of glycemic status (high prediabetes, low prediabetes, normoglycemia) with TBS, using multivariable linear regression with TBS as outcome and glycemic status as categorical primary predictor. Our initial model included the following covariates: age, race/ethnicity, BMI, MT stage (pre- vs. perimenopause), supplemental vitamin D use (yes/no), supplemental calcium use (yes/no), cigarette use (yes/no), and study site. The final, fully adjusted model also controlled for LS BMD. We adjusted for BMI and LS BMD using splines because the relations of these variables with TBS were non-linear [24]. In the case of BMI and TBS, the non-linear relation was tri-phasic (positive for BMI < 24 kg/m2, flat for BMI from 24 to 31 kg/m2, and negative for BMI > 31 kg/m2) [20]. Thus, to adjust for BMI, we used a 3-piece linear spline, with knots (inflection points where the slope changes) at 24 kg/m2 and 31 kg/m2 to model this relationship as piece-wise linear. Specifically, this 3-piece spline allows for different slopes between BMI and TBS in the three BMI categories [24]. Analogously, the relation between BMD and TBS was also non-linear (bi-phasic: positive when LS BMD < 1.080 g/cm2, less positive for LS BMD ≥ 1.080 g/cm2). Therefore, to account for BMD in the model, we used a 2-piece linear spline (with knot at 1.080 g/cm2).
Our second analysis assessed whether greater insulin resistance (assessed by HOMA-IR) is related to lower TBS. We used multivariable linear regression with TBS as the outcome, and HOMA-IR (base 2 log transformed) as continuous primary predictor. We first explored the shape of the relationship between log2HOMA-IR and TBS using LOESS (Fig. 1) and found a biphasic relation with an inflection point at log2HOMA-IR level of 0.7 (corresponding to a raw HOMA-IR value of 1.62). We therefore modeled log2(HOMA-IR) using a 2-piece linear spline with a single knot at 0.7. The decision to assess for a non-linear relation between HOMA-IR and TBS was made a priori, based on experimental data that insulin can have anabolic properties on bone [25, 26], but in insulin resistant states, insulin signaling leads to expansion of bone marrow adipose tissue and decreased trabecular BMD [27]. Covariates were again handled in a two-step fashion as in the first analysis.
Results
Sample characteristics
Table 1 presents participant characteristics. Mean age, log2HOMA-IR, TBS, and LS BMD were 46 years, 0.97, 1.443, and 1.073 g/cm2, respectively. Thirty-two percent of women were Black, 21% Japanese, and the remaining White. Six and 14% were categorized as having high and low prediabetes, respectively. Two hundred three women had BMI values ≥ 35 kg/m2.
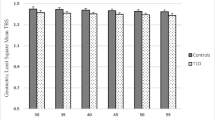
Glycemic status and trabecular bone score
Adjusted for age, race/ethnicity, MT stage, BMI, cigarette use, calcium and vitamin D supplementation, and study site, in multivariable regression, compared to TBS in the normoglycemic state, TBS was significantly lower in high prediabetes (p = 0.01), but not in low prediabetes (p = 0.4) (Table 2). After accounting for lumbar spine BMD, TBS was 0.21 SD lower in women with high prediabetes (p = 0.007) vs. those with normal blood glucose (Table 2).
Insulin resistance and trabecular bone score
On visual inspection of the LOESS plot, the relation between HOMA-IR and TBS was non-linear (Fig. 1), with an inflection point at log2HOMA-IR value of 0.7 (corresponding to raw HOMA-IR level of 1.62). Forty-four percent of participants had HOMA-IR measurements < 1.62; median [IQR] HOMA-IR in these women was 1.20 [0.99, 1.39]. The remaining 56% of women had HOMA-IR levels ≥ 1.62 (median [IQR] = 2.61 [2.05, 3.81]).
In multivariable linear regression adjusting for age, race/ethnicity, MT stage, smoking, calcium and vitamin D supplementation, and study site, TBS was not associated with log2(HOMA-IR) when HOMA-IR was < 1.62 (p = 0.3) but was negatively associated with log2(HOMA-IR) when HOMA-IR was ≥ 1.62 (p = 0.02) (Table 3). After additionally accounting for lumbar spine BMD, each doubling of HOMA-IR was associated with 0.15 SD greater TBS when HOMA-IR was < 1.62 (p = 0.01) and 0.15 SD lower TBS when HOMA-IR was ≥ 1.62 (p < 0.0001) (Table 3).
Discussion
The overarching goal of this cross-sectional analysis was to determine whether, in women without diabetes, prediabetes and insulin resistance are associated with lower TBS. We report that women with high prediabetes (fasting glucose 110–125 mg/dL) have lower TBS than women with normal blood sugars. In addition, more insulin resistance was associated with lower TBS when HOMA-IR was ≥ 1.62.
A negative relation between DM and TBS has been reported in numerous studies [7,8,9,10,11,12,13]. However, few studies to date have examined the potential associations of prediabetes or insulin resistance (in the absence of DM) with TBS [10, 11, 15], and the results of these studies are inconsistent. One possible explanation for these discrepancies is that hyperglycemia and insulin resistance may not adversely impact trabecular microarchitecture until they exceed certain thresholds. In this analysis, TBS was lower in prediabetes, but only among those with fasting glucose ≥ 110 mg/dL. Similarly, when HOMA-IR was < 1.62, there was a positive association between insulin resistance and TBS, suggesting an anabolic effect of insulin at lower levels [25]. However, once HOMA-IR was ≥ 1.62, greater insulin resistance was related to lower TBS. This is consistent with in vivo models demonstrating that in insulin resistant states, insulin signaling leads to expansion of bone marrow adipose tissue and decreased trabecular bone mineral density (BMD) [27]. Osteoblasts may also become resistant to insulin signaling in insulin resistant states [28].
Knowing that high prediabetes (fasting glucose 110–125 mg/dL) may lead to skeletal complications would be important for public health and clinical reasons. Nearly 20% of US adults have prediabetes with fasting glucose in this range [29], but clinicians remain unsure about how aggressively to treat it. Our results suggest that impaired trabecular bone quality (one mechanism of skeletal fragility in DM) may also affect those with fasting glucose ≥ 110 mg/dL. If high prediabetes also leads to fractures, treating it to prevent adverse bone outcomes could be warranted. Several studies testing for a potential relation between prediabetes and fracture have led to inconsistent results [30,31,32,33], but none specifically focused on individuals with fasting blood sugars ≥ 110 mg/dL or with HOMA-IR levels ≥ 1.62. Future studies should ascertain whether prediabetes is indeed a risk factor for incident fracture and, if it is, whether treating it improves trabecular microarchitecture and prevents fractures. Although a prior SWAN analysis reported that TBS did not predict fracture, independent of BMD in midlife women [34], identifying risk factors for lower TBS in this cohort is nonetheless important. This is because TBS does predict fracture, even when accounting for BMD, in older adults [7, 8], and women with lower TBS in midlife are more likely to have lower TBS in later life [20]. This is similar to how women with lower peak bone mass will have lower BMD in older age [35, 36].
This study has limitations that warrant mention. First, is the cross-sectional study design, which limits our ability to draw causal inference. Our results, nonetheless, lay the foundation for future work to examine the associations of prediabetes (with fasting glucose ≥ 110 mg/dL) and HOMA-IR ≥ 1.62 µU/mL as predictors of change in TBS. The second limitation is that we did not include bone quality parameters other than TBS as outcomes in our analysis. Beyond altered trabecular microarchitecture, increased cortical porosity [37], accumulation of advanced glycation end products [38], and decreased bone material strength [39] are features of the diabetic bone phenotype. Unfortunately, cortical microarchitectural assessments were not available in the full SWAN cohort [40], and measuring bone material strength is not feasible in large cohorts. Third, TBS measures are artifactually affected by the thickness of soft tissue (which increases with BMI). Although we used soft-tissue-thickness-corrected TBS, there remained a relationship between TBS and BMI at the low and high ends (below 24 and above 31 kg/m2). To account for this, we modeled BMI using a 3-segment linear spline. Lastly, we had a relatively small number of participants who had fasting glucose ≥ 110 mg/dL.
In conclusion, we report that high prediabetes (fasting glucose 110–125 mg/dL), and greater HOMA-IR (when HOMA-IR is ≥ 1.62) were associated with lower TBS. Future studies should examine the longitudinal associations of prediabetes with higher fasting glucose and HOMA-IR levels above 1.62 µU/mL with longitudinal declines over time in measures of bone strength, including BMD, TBS, and composite strength indices, as well as with incident fracture.
Data availability
Some or all datasets generated during and/or analyzed during the current study are not publicly available but are available from the corresponding author on reasonable request.
References
Shanbhogue VV, Hansen S, Frost M, Brixen K, Hermann AP (2017) Bone disease in diabetes: another manifestation of microvascular disease? Lancet Diabetes Endocrinol 5(10):827–838. https://doi.org/10.1016/s2213-8587(17)30134-1
Khalil N, Sutton-Tyrrell K, Strotmeyer ES, Greendale GA, Vuga M, Selzer F, Crandall CJ, Cauley JA (2011) Menopausal bone changes and incident fractures in diabetic women: a cohort study. Osteoporos Int 22(5):1367–1376. https://doi.org/10.1007/s00198-010-1357-4
Vilaca T, Schini M, Harnan S, Sutton A, Poku E, Allen IE, Cummings SR, Eastell R (2020) The risk of hip and non-vertebral fractures in type 1 and type 2 diabetes: a systematic review and meta-analysis update. Bone 137:115457. https://doi.org/10.1016/j.bone.2020.115457
Koromani F, Oei L, Shevroja E, Trajanoska K, Schoufour J, Muka T, Franco OH, Ikram MA, Zillikens MC, Uitterlinden AG, Krestin GP, Anastassiades T, Josse R, Kaiser SM, Goltzman D, Lentle BC, Prior JC, Leslie WD, McCloskey E, Lamy O, Hans D, Oei EH, Rivadeneira F (2020) Vertebral fractures in individuals with type 2 diabetes: more than skeletal complications alone. Diabetes Care 43(1):137–144. https://doi.org/10.2337/dc19-0925
Vestergaard P (2007) Discrepancies in bone mineral density and fracture risk in patients with type 1 and type 2 diabetes—a meta-analysis. Osteoporos Int 18(4):427–444. https://doi.org/10.1007/s00198-006-0253-4
Silva BC, Leslie WD, Resch H, Lamy O, Lesnyak O, Binkley N, McCloskey EV, Kanis JA, Bilezikian JP (2014) Trabecular bone score: a noninvasive analytical method based upon the DXA image. J Bone Miner Res 29(3):518–530. https://doi.org/10.1002/jbmr.2176
McCloskey EV, Odén A, Harvey NC, Leslie WD, Hans D, Johansson H, Barkmann R, Boutroy S, Brown J, Chapurlat R, Elders PJM, Fujita Y, Glüer CC, Goltzman D, Iki M, Karlsson M, Kindmark A, Kotowicz M, Kurumatani N, Kwok T, Lamy O, Leung J, Lippuner K, Ljunggren Ö, Lorentzon M, Mellström D, Merlijn T, Oei L, Ohlsson C, Pasco JA, Rivadeneira F, Rosengren B, Sornay-Rendu E, Szulc P, Tamaki J, Kanis JA (2016) A meta-analysis of trabecular bone score in fracture risk prediction and its relationship to FRAX. J Bone Miner Res 31(5):940–948. https://doi.org/10.1002/jbmr.2734
Leslie WD, Aubry-Rozier B, Lamy O, Hans D (2013) TBS (trabecular bone score) and diabetes-related fracture risk. J Clin Endocrinol Metab 98(2):602–609. https://doi.org/10.1210/jc.2012-3118
Dhaliwal R, Cibula D, Ghosh C, Weinstock RS, Moses AM (2014) Bone quality assessment in type 2 diabetes mellitus. Osteoporos Int 25(7):1969–1973. https://doi.org/10.1007/s00198-014-2704-7
Holloway KL, De Abreu LLF, Hans D, Kotowicz MA, Sajjad MA, Hyde NK, Pasco JA (2018) Trabecular bone score in men and women with impaired fasting glucose and diabetes. Calcif Tissue Int 102(1):32–40. https://doi.org/10.1007/s00223-017-0330-z
Kim JH, Choi HJ, Ku EJ, Kim KM, Kim SW, Cho NH, Shin CS (2015) Trabecular bone score as an indicator for skeletal deterioration in diabetes. J Clin Endocrinol Metab 100(2):475–482. https://doi.org/10.1210/jc.2014-2047
Xue Y, Baker AL, Nader S, Orlander P, Sanchez AJ, Kellam J, Rianon NJ, Ambrose CG (2018) Lumbar spine trabecular bone score (TBS) reflects diminished bone quality in patients with diabetes mellitus and oral glucocorticoid therapy. J Clin Densitom 21(2):185–192. https://doi.org/10.1016/j.jocd.2017.09.003
Zhukouskaya VV, Eller-Vainicher C, Gaudio A, Privitera F, Cairoli E, Ulivieri FM, Palmieri S, Morelli V, Grancini V, Orsi E, Masserini B, Spada AM, Fiore CE, Chiodini I (2016) The utility of lumbar spine trabecular bone score and femoral neck bone mineral density for identifying asymptomatic vertebral fractures in well-compensated type 2 diabetic patients. Osteoporos Int 27(1):49–56. https://doi.org/10.1007/s00198-015-3212-0
Bonaccorsi G, Fila E, Messina C, Maietti E, Ulivieri FM, Caudarella R, Greco P, Guglielmi G (2017) Comparison of trabecular bone score and hip structural analysis with FRAX(®) in postmenopausal women with type 2 diabetes mellitus. Aging Clin Exp Res 29(5):951–957. https://doi.org/10.1007/s40520-016-0634-2
Ho-Pham LT, Tran B, Do AT, Nguyen TV (2019) Association between pre-diabetes, type 2 diabetes and trabecular bone score: The Vietnam Osteoporosis Study. Diabetes Res Clin Pract 155:107790. https://doi.org/10.1016/j.diabres.2019.107790
Herman WH, Ratner RE (2020) Metformin should be used to treat prediabetes in selected individuals. Diabetes Care 43(9):1988–1990. https://doi.org/10.2337/dci20-0030
Davidson MB (2020) Metformin should not be used to treat prediabetes. Diabetes Care 43(9):1983–1987. https://doi.org/10.2337/dc19-2221
Mazzetti G, Berger C, Leslie WD, Hans D, Langsetmo L, Hanley DA, Kovacs CS, Prior JC, Kaiser SM, Davison KS, Josse R, Papaioannou A, Adachi JR, Goltzman D, Morin SN (2017) Densitometer-specific differences in the correlation between body mass index and lumbar spine trabecular bone score. J Clin Densitom 20(2):233–238. https://doi.org/10.1016/j.jocd.2016.11.003
Shevroja E, Lamy O, Aubry-Rozier B, Hans G, Rodriguez EG, Stoll D, Hans D the impact of a beta trabecular bone score (TBS) algorithm accounting for soft tissue thickness correction on the prediction of incident major osteoporotic fracture (MOF) risk in postmenopausal women: the OsteoLaus study. In: JOURNAL OF BONE AND MINERAL RESEARCH, 2018. WILEY 111 RIVER ST, HOBOKEN 07030–5774, NJ USA, pp 396–396
Greendale GA, Huang M, Cauley JA, Liao D, Harlow S, Finkelstein JS, Hans D, Karlamangla AS (2020) Trabecular bone score declines during the menopause transition: the Study of Women’s Health Across the Nation (SWAN). J Clin Endocrinol Metab 105 (4). doi:https://doi.org/10.1210/clinem/dgz056
Phillips LS, Weintraub WS, Ziemer DC, Kolm P, Foster JK, Vaccarino V, Rhee MK, Budhwani RK, Caudle JM (2006) All pre-diabetes is not the same: metabolic and vascular risks of impaired fasting glucose at 100 versus 110 mg/dl. The Screening for Impaired Glucose Tolerance Study 1 (SIGT 1) 29 (6):1405–1407. https://doi.org/10.2337/dc06-0242
Sorkin JD, Muller DC, Fleg JL, Andres R (2005) The relation of fasting and 2-h postchallenge plasma glucose concentrations to mortality. Data from the Baltimore Longitudinal Study of Aging with a critical review of the literature 28 (11):2626-2632. doi:https://doi.org/10.2337/diacare.28.11.2626
Santoro N, Torrens J, Crawford S, Allsworth JE, Finkelstein JS, Gold EB, Korenman S, Lasley WL, Luborsky JL, McConnell D, Sowers MF, Weiss G (2005) Correlates of circulating androgens in mid-life women: the study of women’s health across the nation. J Clin Endocrinol Metab 90(8):4836–4845. https://doi.org/10.1210/jc.2004-2063
Smith PL (1979) Splines as a useful and convenient statistical tool. Am Stat 33(2):57–62
Hashizume M, Yamaguchi M (1993) Stimulatory effect of beta-alanyl-L-histidinato zinc on cell proliferation is dependent on protein synthesis in osteoblastic MC3T3-E1 cells. Mol Cell Biochem 122(1):59–64. https://doi.org/10.1007/bf00925737
Wergedal JE, Baylink DJ (1984) Characterization of cells isolated and cultured from human bone. Proc Soc Exp Biol Med 176(1):60–69. https://doi.org/10.3181/00379727-176-41843
Tencerova M, Figeac F, Ditzel N, Taipaleenmäki H, Nielsen TK, Kassem M (2018) High-fat diet-induced obesity promotes expansion of bone marrow adipose tissue and impairs skeletal stem cell functions in mice. J Bone Miner Res 33(6):1154–1165. https://doi.org/10.1002/jbmr.3408
Wei J, Ferron M, Clarke CJ, Hannun YA, Jiang H, Blaner WS, Karsenty G (2014) Bone-specific insulin resistance disrupts whole-body glucose homeostasis via decreased osteocalcin activation. J Clin Invest 124(4):1–13. https://doi.org/10.1172/jci72323
Hostalek U (2019) Global epidemiology of prediabetes - present and future perspectives. Clin Diabetes Endocrinol 5:5–5. https://doi.org/10.1186/s40842-019-0080-0
Park HY, Han K, Kim Y, Kim YH, Sur YJ (2021) The risk of hip fractures in individuals over 50 years old with prediabetes and type 2 diabetes - a longitudinal nationwide population-based study. Bone 142:115691. https://doi.org/10.1016/j.bone.2020.115691
Chen C, Chen Q, Nie B, Zhang H, Zhai H, Zhao L, Xia P, Lu Y, Wang N (2020) Trends in bone mineral density, osteoporosis, and osteopenia among U.S. adults with prediabetes, 2005–2014. Diabetes Care 43 (5):1008–1015. doi:https://doi.org/10.2337/dc19-1807
Looker AC, Eberhardt MS, Saydah SH (2016) Diabetes and fracture risk in older U.S. adults. Bone 82:9–15. https://doi.org/10.1016/j.bone.2014.12.008
Napoli N, Strotmeyer ES, Ensrud KE, Sellmeyer DE, Bauer DC, Hoffman AR, Dam T-TL, Barrett-Connor E, Palermo L, Orwoll ES, Cummings SR, Black DM, Schwartz AV (2014) Fracture risk in diabetic elderly men: the MrOS study. Diabetologia 57(10):2057–2065. https://doi.org/10.1007/s00125-014-3289-6
Greendale GA, Huang M, Cauley JA, Harlow S, Finkelstein JS, Karlamangla AS (2020) Premenopausal and early postmenopausal trabecular bone score (TBS) and fracture risk: Study of Women’s Health Across the Nation (SWAN). Bone 140:115543. https://doi.org/10.1016/j.bone.2020.115543
Shieh A, Karlamangla AS, Huang MH, Han W, Greendale GA (2021) Faster lumbar spine bone loss in midlife predicts subsequent fracture independent of starting bone mineral density. J Clin Endocrinol Metab 106(7):e2491–e2501. https://doi.org/10.1210/clinem/dgab279
Heaney RP, Abrams S, Dawson-Hughes B, Looker A, Marcus R, Matkovic V, Weaver C (2000) Peak bone mass. Osteoporos Int 11(12):985–1009. https://doi.org/10.1007/s001980070020
Burghardt AJ, Issever AS, Schwartz AV, Davis KA, Masharani U, Majumdar S, Link TM (2010) High-resolution peripheral quantitative computed tomographic imaging of cortical and trabecular bone microarchitecture in patients with type 2 diabetes mellitus. J Clin Endocrinol Metab 95(11):5045–5055. https://doi.org/10.1210/jc.2010-0226
Rokidi S, Andrade VFC, Borba V, Shane E, Cohen A, Zwerina J, Paschalis EP, Moreira CA (2020) Bone tissue material composition is compromised in premenopausal women with type 2 diabetes. Bone 141:115634. https://doi.org/10.1016/j.bone.2020.115634
Dawson-Hughes B, Bouxsein M, Shea K (2019) Bone material strength in normoglycemic and hyperglycemic black and white older adults. Osteoporos Int 30(12):2429–2435. https://doi.org/10.1007/s00198-019-05140-1
Yu EW, Putman MS, Derrico N, Abrishamanian-Garcia G, Finkelstein JS, Bouxsein ML (2015) Defects in cortical microarchitecture among African-American women with type 2 diabetes. Osteoporos Int 26(2):673–679. https://doi.org/10.1007/s00198-014-2927-7
Acknowledgements
Clinical Centers: University of Michigan, Ann Arbor – Siobán Harlow, PI 2011 to present, MaryFran Sowers, PI 1994–2011; Massachusetts General Hospital, Boston, MA – Sherri‐Ann Burnett‐Bowie, PI 2020 to present; Joel Finkelstein, PI 1999–2020; Robert Neer, PI 1994–1999; Rush University, Rush University Medical Center, Chicago, IL – Imke Janssen, PI 2020 to present; Howard Kravitz, PI 2009–2020; Lynda Powell, PI 1994–2009; University of California, Davis/Kaiser – Elaine Waetjen and Monique Hedderson, PIs 2020 to present; Ellen Gold, PI 1994–2020; University of California, Los Angeles – Arun Karlamangla, PI 2020 to present; Gail Greendale, PI 1994–2020; Albert Einstein College of Medicine, Bronx, NY – Carol Derby, PI 2011 to present, Rachel Wildman, PI 2010–2011; Nanette Santoro, PI 2004–2010; University of Medicine and Dentistry – New Jersey Medical School, Newark – Gerson Weiss, PI 1994–2004; and the University of Pittsburgh, Pittsburgh, PA – Rebecca Thurston, PI 2020 to present; Karen Matthews, PI 1994–2020.
NIH Program Office: National Institute on Aging, Bethesda, MD – Rosaly Correa-de-Araujo 2020 to present; Chhanda Dutta 2016 to present; Winifred Rossi 2012–2016; Sherry Sherman 1994–2012; Marcia Ory 1994–2001; National Institute of Nursing Research, Bethesda, MD – Program Officers.
Central Laboratory: University of Michigan, Ann Arbor – Daniel McConnell (Central Ligand Assay Satellite Services).
Coordinating Center: University of Pittsburgh, Pittsburgh, PA – Maria Mori Brooks, PI 2012 to present; Kim Sutton-Tyrrell, PI 2001–2012; New England Research Institutes, Watertown, MA—Sonja McKinlay, PI 1995–2001.
Steering Committee:Susan Johnson, Current Chair
Chris Gallagher, Former Chair
We thank the study staff at each site and all the women who participated in SWAN.
Funding
The Study of Women’s Health Across the Nation (SWAN) has grant support from the National Institutes of Health (NIH), DHHS, through the National Institute on Aging (NIA), the National Institute of Nursing Research (NINR) and the NIH Office of Research on Women’s Health (ORWH) (Grants U01NR004061; U01AG012505, U01AG012535, U01AG012531, U01AG012539, U01AG012546, U01AG012553, U01AG012554, U01AG012495, and U19AG063720). This study was also supported by grant 5R01AG026463.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Disclaimer
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIA, NINR, ORWH, or the NIH.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Shieh, A., Greendale, G.A., Cauley, J.A. et al. Prediabetes and insulin resistance are associated with lower trabecular bone score (TBS): cross-sectional results from the Study of Women’s Health Across the Nation TBS Study. Osteoporos Int 33, 1365–1372 (2022). https://doi.org/10.1007/s00198-022-06325-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-022-06325-x