Abstract
Summary
Oral glucocorticoids may increase major osteoporotic fracture risk (MOF) in myasthenia gravis patients. To assess this risk, we performed a case–control study including all Danish patients with a MOF between 1995 and 2011. We also pooled our data with data from another study. We found no increased risk. Osteoporosis prevention remains advisable.
Purpose/introduction
The prolonged use of high doses of oral glucocorticoids (GCs), a common treatment in patients with myasthenia gravis (MG), may increase major osteoporotic fracture (MOF) risk. Previous epidemiological studies did not exclusively focus on patients with MG or had relatively few GC-exposed MG patients. Aims were to evaluate the risk of MOF in MG patients using oral GCs in a large study population and to perform a pooled analysis with data from previous work.
Methods
A population-based case–control study (1995–2011) was conducted using the Danish National Health Service. Cases had sustained a MOF, and controls had not. All were aged ≥ 18 years. Multivariate conditional logistic regression estimated odds ratios (ORs) among MG patients using oral GCs versus non-users. Adjustments were made for comorbidities and comedications. In the pooled analysis, results were pooled by the use of generic inverse variance methods, assuming a random-effects model.
Results
We identified 376,858 cases and 376,858 controls. MOF risk was not elevated in MG patients currently using oral GCs compared to MG patients not on oral GCs (ORadj.: 1.26 (95% CI 0.68–2.33)). The use of the highest cumulative dose of oral GCs (≥ 7 g) did not show an increased risk of MOF among MG patients (ORadj.: 2.00 (95% CI 0.90–4.44)). Our pooled analysis also showed no association between oral GC use and MOF risk.
Conclusion
This study showed that oral GC use in patients with MG was not associated with increased risk of MOF in our case–control study and pooled analysis. Osteoporosis prevention in MG patients based on clinical guidelines remains advisable.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Oral glucocorticoids (GCs) play an important role in the treatment of patients with myasthenia gravis (MG), an autoimmune neuromuscular disease leading to fluctuating muscle weakness and fatigability of skeletal muscles. Patients with MG are at an increased risk of developing osteoporosis. This risk may increase further when they use oral GCs [1]. Among MG patients, long-term high doses of oral GCs are one of the treatment options. The prednisone rapid induction regimen starts with 1–1.5 mg/kg/day (max. 100 mg) for a period of 2–4 weeks, followed by a maintenance dose at the same level daily or every other day, for 4–8 weeks. After improvement, a tapering schedule with 5–10 mg a month can be initiated [2]. The resulting prolonged exposure and high cumulative dose may carry a considerable risk of major osteoporotic fracture (MOF) [3,4,5]. Epidemiological studies have shown that the GC-induced fracture risk increases with daily dose and cumulative dose and occurs rapidly after starting therapy [4, 6, 7]. This has indirectly been supported by a study in patients which showed, through bone histomorphometry, significant thinner, and less connected trabeculae after high cumulative doses of oral GCs (> 10 g prednisone equivalent) compared to a lower cumulative dose of oral GCs (< 10 g prednisone equivalent) [8]. The authors conclude that their observation suggests a possible threshold at which bone recovery after withdrawal of oral GCs would be impossible due to a dramatic disruption of the trabecular network.
The aforementioned epidemiological studies did not exclusively focus on patients with MG, but evaluated the GC use and the risk of osteoporotic fracture in general [3,4,5,6,7]. Clinical guidelines recommend the prescription of prophylaxis (e.g., bisphosphonates) based on the risk assessment [9, 10] and/or based on age, GC dose, and/or duration of the GC therapy [11]. Among patients with MG, few observational studies have evaluated the risk of osteoporotic fracture with oral GC use and showed contrasting results [12, 13]. A cohort study using a large UK primary care database did not support a causal relationship between oral GC use and the risk of MOF among MG patients [12]. Even when the daily dose was ≥ 15 mg or the cumulative exposure ≥ 5 g prednisolone equivalents, no association was found. A cross-sectional survey which included 363 Japanese patients with MG found that the duration but not the daily dose of prednisolone was associated with osteoporotic fractures [13]. The absence of an association between long-term high-dose oral GC use and MOF risk among MG patients in these studies remains intriguing, although small numbers of long-term high-dose oral GC use may be an alternative explanation. Therefore, the primary objective was to evaluate the risk of MOF in MG patients using oral GC in a different, large study population. The secondary objective was to pool these data with the results of a cohort study performed by our group [12] to gain more statistical power.
Methods
Case–control study
Data source
In Denmark, separate registers of computerized medical records on all contacts to hospitals and on the use of drugs can be linked for the entire population (approximately 5.5 million inhabitants). Information on hospital admissions is kept in the National Hospital Discharge Register. The register was founded in 1977 and covers all inpatient contacts from 1977 to 1994 and from 1995 also all outpatient visits to hospitals, outpatient clinics, and emergency rooms. Upon discharge, the physician codes the reason for the contact according to the International Classification of Diseases, 8th and 10th revision (ICD8/ICD10). The register has nationwide coverage of public hospitals with an almost 100% completeness of recordings and a high precision of diagnoses [14, 15], particularly for fracture [16].
The Danish Medicines Agency keeps a nationwide dispensing database, the Register of Medicinal Product Statistics, with key information on prescriptions for refundable drugs. The dispensing database includes information on the patient’s civil registry number, the type and amount of drug prescribed according to the Anatomical Therapeutical Chemical classification system (ATC) [17], and the data when the prescription was filled. The database was started on January 1, 1995, and updated hereafter. As was previously shown, all registers can be linked through the use of the civil registry number that is assigned to all Danish citizens [18].
Study population
A population-based case–control study was conducted using data from the Danish National Healthcare Service (DNHS) registries. Cases were all subjects aged 18 years and older, who had sustained a major osteoporotic fracture (MOF) between January 1, 1995, and December 31, 2011. A MOF was defined as a fracture of the hip (ICD10 code S72.0-S72.2), radius/ulna (S52), vertebrae (S12, S22.0-S22.1, S32.0-S32.2, S32.7, S32.8, T08), or humerus (S42.2-S42.4) according to the World Health Organization’s (WHO) definition [19]. To each case, a control subject who did not sustain a MOF was randomly matched by gender and year of birth using the incidence-density sampling technique [20]. The date of the first MOF defined the index date. Controls were assigned the same index date as their matched cases. Major osteoporotic fractures were considered as the primary outcome of interest. Given the fact that oral GC use affects all fracture types, any fracture (S02, S12, S22, S32, S42, S52, S62, S72, S82, S92, T02, T08, T10 and T12) was a secondary outcome of interest.
Exposure
The presence of MG before the index date was defined based on ICD-10 code G70.0, G70.1, and G70.8. Patients without a record for MG before the index date were classified as no MG patients. We evaluated the oral GC use before the index date for all patients. Based on the time since the most recent oral GC dispensing, patients were classified as current (1–91 days), recent (92–182 days), past (183–364 days), or distant past (over 364 days) users. The classification was derived from an article by van Staa et al. that describes the risk of different kinds of fractures before, during, and after oral corticosteroid use [4]. For each current user, we estimated both the cumulative and average daily oral GC exposure. The cumulative dose was calculated by adding up all previous oral GC dispensing using defined daily dosages (DDDs) according to the WHO definition [21]. The average daily dose was calculated by dividing the cumulative oral GC exposure by the treatment time (i.e., the time between the first oral GC dispensing and the index date). The GC exposure was expressed as oral prednisolone equivalents. We defined our cumulative dose categories as < 1.0 g, 1.0–6.9 g, and ≥ 7.0 g. The average daily dose was broken down into the following categories: < 7.5 mg, 7.5–14.9 mg, and ≥ 15 mg. Cut-offs were based on a paper by de Vries et al. on oral GC use and fracture risk and on the cumulative dose for a “typical” high-dose regimen mentioned in a paper on MG treatment [2, 6].
Potential confounders
We considered the following potential confounders before the index date: a history of chronic obstructive pulmonary disease (COPD), fracture, rheumatoid arthritis, inflammatory bowel disease (IBD), asthma, cancer, type 2 diabetes mellitus, dementia, congestive heart failure, cerebrovascular disease, or secondary osteoporosis (type 1 diabetes mellitus, hyperthyroidism, hypogonadism, and renal failure). Other potential confounders included a dispensing in 6 months before the index date of the following drugs: bisphosphonates, vitamin D, calcium, raloxifene, strontium ranelate, denosumab, calcitonin, parathyroid hormone, hormone replacement therapy, inhaled corticosteroids, inhaled bronchodilators, antipsychotics, antidepressants, hypnotics/anxiolytics, anticonvulsants, or anti-Parkinson drugs.
Statistical analyses
Conditional logistic regression was used to estimate odds ratios (ORs) for major osteoporotic fracture risk and risk of any fracture (SAS software version 9.3, SAS Institute Inc., Cary, North Carolina, USA). Analyses were stratified by age, gender, and myasthenia gravis. The current oral GC use was stratified by cumulative and average daily dose. All results were presented as OR with the corresponding 95% confidence intervals (CIs). In all analyses, potential confounders were included if they independently changed the beta-coefficient for current oral GC exposure by at least 5% or when consensus about inclusion existed within the team of researchers, supported by clinical evidence from the literature. In a sensitivity analysis, we additionally adjusted the main analysis for the use of bisphosphonates in 6 months prior to the index date.
Pooled analysis
In order to increase the power, we combined the present results, of our case–control study, with the results of a cohort study performed in the British population [12], resulting in a pooled analysis. From both studies, we extracted the data on average and cumulative oral GC dose with the risk of major osteoporotic and any fracture. The cumulative daily dose categories were not similar between studies; therefore, we redefined our cumulative dose categories to < 2.5 g, 2.5–5.0 g, and ≥ 5.0 g, to make them similar to those used in the paper by Pouwels. No adjustment was needed for the average daily dose categories.
Results from the cumulative and average daily dose analyses were then pooled by the use of generic inverse variance methods, assuming a random effects model. This was done separately for major osteoporotic and any fractures. Heterogeneity was assessed by the Cochrane Q statistic and the I2 statistic. Analyses were performed using RevMan Version 5.3 (Cochrane Collaboration, Oxford, UK). Heterogeneity was characterized as low (values < 30%), moderate (30–49%), or high (> 50%). A p value of < 0.05 was considered to be statistically significant.
Results
Case–control study
Table 1 shows the baseline characteristics for the total population. The study population consisted of 376,858 cases, aged 18 years and older, and the same number of controls. Both the cases and controls had a mean age of 64.2 years, and 68.7% of the study population were women. A higher proportion of patients with a MOF (5.2%) had used oral GC within 6 months prior to index date versus controls (3.6%). The proportion of MG patients within cases and controls was comparable (0.03%). Table 2 shows baseline characteristics for MG patients.
Table 3 shows that the risk of MOF was not elevated among MG patients who were the current oral GC users as compared to the non-users (adj. OR 1.26 (95% CI 0.68–2.33)). In patients without MG, the risk of MOF was significantly higher with the current oral GC use as compared to non-users (adj. OR 1.37 (95% CI 1.34–1.41)). Further stratified analyses suggested that the risk of MOF in MG patients was highest among those current users who received the highest cumulative dose of oral GC (≥ 7 g), although this did not reach statistical significance adj. (OR 2.00 (95% CI 0.90–4.44)). When the current use was stratified by an average daily dose of oral GC, the risk estimates for MOF were not significantly elevated. Furthermore, the MOF risk did not differ significantly among MG patients with the recent oral GC use (adj. OR 1.39 (95% CI 0.31–6.23)), past oral GC use (adj. OR 1.92 (95% CI 0.56–6.54)), and distant past oral GC (adj. OR 1.02 (95% CI 0.61–1.69)). In contrast, the risk of MOF was significantly elevated in patients without MG using oral GC (any exposure type) compared with patients not using oral GC. Additional adjustments for the use of bisphosphonates did not materially alter our results.
The current oral GC exposure was not associated with the risk of any fracture among MG patients (OR 1.08 (95% CI 0.69–1.70)) compared to non-users (Table 4). Further stratified analyses suggested that the risk of any fracture in MG patients tended to be strongest for the highest cumulative dose (≥ 7 g) (adj. OR 1.65 (95% CI 0.93–2.91)). However, the difference did not reach statistical significance. The stratification of the current oral GC use by the average daily dose of the oral GC did not modify the risk. Similarly, the recent oral GC use (adj. OR 1.25 (95% CI 0.54–2.89)), past oral GC use (adj. OR 2.73 (95% CI 0.97–7.70)), and distant past oral GC use (adj. OR 1.06 (95% CI 0.71–1.58) did not substantially change the risk of any fracture among MG patients, when compared with non-GC use. Finally, among patients without a MG diagnosis, the risk of any fracture was significantly increased in every subgroup of an oral GC exposure compared to non-GC use.
Pooled analysis
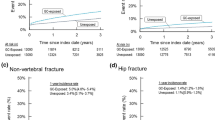
Table 5 demonstrates the results of aggregating findings from British [12] and Danish data (current study). The risk of MOF among MG patients using oral GC was not increased in any of the sub-analysis of our pooled analysis. For MOF, no heterogeneity was reported across studies.
The results of the pooled data for the risk of any fracture showed the same trend as for MOF and were not significant when the current oral GC use was stratified by cumulative exposure or average daily dose (Table 5). For any fracture, high heterogeneity (> 50%) was observed in the categories of cumulative exposure across studies. No heterogeneity was detected in the categories of average daily dose across studies.
For this pooled analysis, we recalculated the results of the current (case–control) study to match those used in the study by Pouwels et al. [12]. For the risk of MOF, we found an adj. OR of 0.31 (95% CI 0.03–3.14) with < 2.5 g of oral GC use, an adj. OR of 0.36 (95% CI 0.07–1.87) with 2.5–5.0 g of oral GC use, and an adj. OR of 1.97 (95% CI 0.92–4.24) for the highest cumulative dose of ≥ 5.0 g of oral GC use (data not shown).
For the risk of any fracture, we found an adj. OR of 0.13 (95% CI 0.02–0.92) with < 2.5 g of oral GC use, adj. OR of 0.29 (95% CI 0.06–1.42) with 2.5–5.0 g of oral GC use, and adj. OR of 0.73 (95% CI 0.28–1.95) with ≥ 5.0 g of oral GC use among MG patients (data not shown).
Discussion
The present study showed that there was no significant association with the current oral GC use and risk of major osteoporotic fracture (MOF) among MG patients. When stratifying current oral GC use by cumulative dose or average daily dose, there was no association with the risk of MOF, both in our case–control study and after we had aggregated those results with previous findings [12] in a pooled analysis.
Our findings of the case–control study are in agreement with those reported by a population-based cohort study in patients with MG using data from the UK Clinical Practice Research Datalink (CPRD) [12]. It comprised a large study including patients representative for the total UK population and found no association with risk of MOF and oral GC use, not even when the cumulative exposure had exceeded 5 g of prednisolone equivalents (adj. HR 0.99 (95% CI 0.31–3.14)). While our study was performed as a case–control study, it should yield similar results as a study with a cohort design [22]. The major difference between CPRD and our database is that in de CPRD, the data is collected by the general practitioners (GPs) and our database is based on hospitalization registries linked to community pharmacy dispensing records. The capture of fractures that require an inpatient hospitalization or accident and emergency visit in our study is therefore probably higher. A cross-sectional study [13] found that the duration of GC use (cumulative exposure) was associated with osteoporotic fractures among MG patients.
We observed that our results of the case–control study in patients without MG are in line with the main result found by Van Staa et al. [4]. They showed that the use of oral GCs was associated with a 1.6-fold increased risk of non-vertebral fracture in the general population, for patients with an average daily dose of ≥ 7.5 mg per day. They also observed a 5.2-fold higher risk of vertebral fractures for patients who were prescribed ≥ 7.5 mg of prednisolone equivalents per day.
Although MG patients are frequently exposed to prolonged periods of high doses of prednis(ol)one, no increased risk in MOF fracture was observed in our study. This could be due to the limited number of MG patients in our study. To increase the sample size and further investigate whether a true association exists between oral GC use in MG patients and risk of MOF, we performed a pooled analysis. Albeit still limited in statistical power, we did not observe a difference in major osteoporotic or any fracture risk among MG patients with oral GC use in our pooled analysis. Differences in the definition of major osteoporotic fractures were present between the studies. Another difference was the level of detail of recorded diagnosis and symptoms. Hospitalization registries, such as DNHS, are coded using the ICD system 8th and 10th revision, while the CPRD used Read coding which contains much more detail than ICD8 and 10 [23].
It is possible that MG itself has an effect on the risk of fractures, for example, a decreased risk due to reduced mobility, patients being more cautious or physiological reasons, or an increased risk due to muscle weakness. In a study by Kassardjian et al., it was shown that MG patients had a significantly lower risk of fracture compared to non-MG patients [24].
It has been reported that acetylcholine receptors are present in human osteoblasts [25, 26]. Acetylcholine is an important neurotransmitter which plays a role in regulating the proliferation and differentiation of various cell types, including osteoblasts [25]. Acetylcholinesterase inhibitors used in MG may have a positive effect on bone remodeling, counteracting the effects of GC use on bone. A study in mice showed an increase in trabecular bone mass after administration of galantamine, an acetylcholinesterase inhibitor that passes the blood–brain barrier (BBB) [27]. This mechanism could be an explanation for our results. On the contrary, in the same study, the administration of pyridostigmine, a mostly peripheral acting acetylcholinesterase inhibitor that is used in MG, resulted in trabecular bone loss [27]. It is unclear how these findings translate to humans.
There is evidence from randomized trials that bisphosphonates (BPs) reduce corticosteroid-induced osteoporosis, and their use is mentioned in several guidelines [9,10,11]. BPs could suppress bone turnover, increase BMD, and reduce fracture risk in patients receiving GC treatment [9]. It is likely that a significant part of patients would have received anti-osteoporosis medication during oral GC use. In one particular study, up to 52% of MG patients with oral GC use did receive medical prophylaxis (BPs) [13]. Although initially we considered anti-osteoporosis medication to be a potential confounder, we have not adjusted for it, as we think that the use of anti-osteoporosis medication is in the causal pathway between GC use and MOF. A true confounder should be associated with both the exposure and the outcome and not in the causal pathway [28, 29]. Additional adjustment in a sensitivity analysis for the use of bisphosphonates did not alter our results.
Wakata et al. concluded that prednisolone-treated patients with MG have an acceptable risk of bone loss if prophylactic medication is administered [30]. However, other factors such as the age of the patient, the severity of the disease, and dietary intake or decreased physical activity confer to increased fracture risk in MG patients with oral GC use.
The main strengths of our case–control study include that it had one of the largest possible sample sizes (cases and controls were sampled from the full country of Denmark). As a result, it was also population-based. This makes selection bias unlikely. In Denmark, almost all patients with fractures are managed in the hospital system (also including emergency rooms), and even fractures sustained abroad are registered upon return for insurance reasons. The capture of fractures is thus very high. There was detailed longitudinal information on drug prescribing in our study population, which enabled us to reliable estimate average and cumulative oral GC exposure. We were also able to adjust for a wide range of covariates. A particular strength of our pooled analysis is its use of the same cumulative and average daily dose categories which allowed us to use the same definition across the studies.
There are several limitations to our case–control study. Despite the large total sample size, we had small numbers in the different GC groups among MG patients, and these subgroups may have been underpowered. This study relies on diagnoses recorded by physicians. Underreporting could influence our results. Confounding and distortion of findings by unknown causes are of considerable concern in an observational study. Data on smoking, alcohol exposure, and body mass index (BMI) were not available. We could not adjust for these potential confounders. A limitation of our pooled analysis was the high heterogeneity (> 50%) in the cumulative exposure categories of any fracture exposure across studies. Other limitations are the relatively small number of major osteoporotic fractures and the fact that in there we included only two studies in our pooled analysis. The included studies have adjusted for different sets of confounders, which may have biased our results.
In conclusion, our study showed that oral GC use in patients with MG was not associated with an increased risk of MOF compared to controls, also when stratified by cumulative and average daily dose. However, only small numbers of MG patients with oral GC use were included in the subgroup analyses. For this reason, these data should be interpreted with caution. Further investigation could provide more clarification, although achieving enough power in such a study or meta-analysis might be difficult. Our recommendation is to co-prescribe bisphosphonates according to the current country-specific clinical guidelines for the treatment of GC-induced osteoporosis.
Data availability
The electronic health data that was used for data management and data analysis is available during confidential on-site data audits, subject to further agreement and permission from the data licensor (Statistics Denmark, project number 703381). The current GDPR regulations limit the access of data to licensed researchers and preclude reports of counts of 5 or fewer patients in tables or text.
Code availability
Computer coding that was used for data management and data analysis is available during confidential on-site data audits, subject to further agreement.
References
Yeh J-H, Chen H-J, Chen Y-K, Chiu H-C, Kao C-H (2014) Increased risk of osteoporosis in patients with myasthenia gravis: a population-based cohort study. Neurology 83(12):1075–1079. https://doi.org/10.1212/WNL.0000000000000804
Farmakidis C, Pasnoor M, Dimachkie MM, Barohn RJ (2018) Treatment of myasthenia gravis. Neurol Clin 36(2):311–337. https://doi.org/10.1016/j.ncl.2018.01.011
Vestergaard P, Olsen ML, Paaske Johnsen S, Rejnmark L, Sørensen HT, Mosekilde L (2003) Corticosteroid use and risk of hip fracture: a population-based case-control study in Denmark. J Intern Med 254(5):486–493. https://doi.org/10.1046/j.1365-2796.2003.01219.x
Van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Use of oral corticosteroids and risk of fractures. J Bone Miner Res 15(6):993–1000. https://doi.org/10.1359/jbmr.2000.15.6.993
Vestergaard P, Rejnmark L, Mosekilde L (2005) Fracture risk associated with systemic and topical corticosteroids. J Intern Med 257(4):374–384. https://doi.org/10.1111/j.1365-2796.2005.01467.x
De Vries F, Bracke M, Leufkens HGM, Lammers J-WJ, Cooper C, Van Staa TP (2007) Fracture risk with intermittent high-dose oral glucocorticoid therapy. Arthritis Rheum 56(1):208–214. https://doi.org/10.1002/art.22294
van Staa TP, Leufkens HG, Abenhaim L, Zhang B, Cooper C (2000) Oral corticosteroids and fracture risk: relationship to daily and cumulative doses. Rheumatology 39(12):1383–1389. https://doi.org/10.1093/rheumatology/39.12.1383
Dalle Carbonare L, Bertoldo F, Valenti MT et al (2005) Histomorphometric analysis of glucocorticoid-induced osteoporosis. Micron 36(7–8):645–652. https://doi.org/10.1016/j.micron.2005.07.009
Buckley L, Guyatt G, Fink HA et al (2017) American College of Rheumatology Guideline for the prevention and treatment of glucocorticoid-induced osteoporosis. Arthritis Rheumato 69(8):1521–1537. https://doi.org/10.1002/art.40137
The National Osteoporosis Guideline Group (NOGG), Compston J, Cooper A (2017) UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos 12(1):43. https://doi.org/10.1007/s11657-017-0324-5
Lems WF, Appelman CLM (2011) Derde herziene richtlijn osteoporose en fractuurpreventie. Nederlandse Vereniging voor Reumatologie. https://www.volksgezondheidenzorg.info/bestanden/documenten/cbo-richtlijn-osteoporose-en-fractuurpreventie-2011 Accessed February 4, 2021
Pouwels S, de Boer A, Javaid MK et al (2013) Fracture rate in patients with myasthenia gravis: the general practice research database. Osteoporos Int 24(2):467–476. https://doi.org/10.1007/s00198-012-1970-5
Konno S, Suzuki S, Masuda M et al (2015) Association between glucocorticoid-induced osteoporosis and myasthenia gravis: a cross-sectional study. PLoS ONE 10(5):e0126579. https://doi.org/10.1371/journal.pone.0126579
Andersen TF, Madsen M, Jørgensen J, Mellemkjoer L, Olsen JH (1999) The Danish National Hospital Register. A valuable source of data for modern health sciences. Dan Med Bull 46(3):263–268
Mosbech J, Jørgensen J, Madsen M, Rostgaard K, Thornberg K, Poulsen TD (1995) The national patient registry. Evaluation of data quality Ugeskr Laeger 157(26):3741–3745
Vestergaard P, Mosekilde L (2002) Fracture risk in patients with celiac disease, Crohn’s disease, and ulcerative colitis: a nationwide follow-up study of 16,416 patients in Denmark. Am J Epidemiol 156(1):1–10. https://doi.org/10.1093/aje/kwf007
Nielsen GL, Sørensen HT, Zhou W, Steffensen FH, Olsen J (1997) The Pharmacoepidemiologic Prescription Database of North Jutland - a valid tool in pharmacoepidemiological research. Int J Risk Saf Med 10(3):203–205. https://doi.org/10.3233/JRS-1997-10309
Vestergaard P, Prieto-Alhambra D, Javaid MK, Cooper C (2013) Fractures in users of antidepressants and anxiolytics and sedatives: effects of age and dose. Osteoporos Int 24(2):671–680. https://doi.org/10.1007/s00198-012-2043-5
Kanis J. Assessment of osteoporosis at the primary health-care level (2007) https://www.sheffield.ac.uk/FRAX/pdfs/WHO_Technical_Report.pdf
Wacholder S, McLaughlin JK, Silverman DT, Mandel JS (1992) Selection of controls in case-control studies. I Principles Am J Epidemiol 135(9):1019–1028. https://doi.org/10.1093/oxfordjournals.aje.a116396
WHO. ATC classification index with DDDs. https://www.whocc.no/atc_ddd_index/
Lalmohamed A, van Staa TP, Vestergaard P et al (2016) Statins and risk of lower limb revision surgery: the influence of differences in study design using electronic health records from the United Kingdom and Denmark. Am J Epidemiol 184(1):58–66. https://doi.org/10.1093/aje/kwv311
Stuart-Buttle CD, Read JD, Sanderson HF, Sutton YM (1996) A language of health in action: read codes, classifications and groupings. Proc Conf Am Med Inform Assoc AMIA Fall Symp 75–9. https://pubmed.ncbi.nlm.nih.gov/8947631/
Kassardjian C, Widdifield J, Paterson JM, et al. Fracture risk in patients with myasthenia gravis: a population-based cohort study. JND. Published online February 4, 2021:1–8. https://doi.org/10.3233/JND-200612
Sato T, Abe T, Chida D et al (2010) Functional role of acetylcholine and the expression of cholinergic receptors and components in osteoblasts. FEBS Lett 584(4):817–824. https://doi.org/10.1016/j.febslet.2010.01.001
En-Nosse M, Hartmann S, Trinkaus K et al (2009) Expression of non-neuronal cholinergic system in osteoblast-like cells and its involvement in osteogenesis. Cell Tissue Res 338(2):203–215. https://doi.org/10.1007/s00441-009-0871-1
Ma Y, Elefteriou F (2020) Brain-derived acetylcholine maintains peak bone mass in adult female mice. J Bone Miner Res 35(8):1562–1571. https://doi.org/10.1002/jbmr.4024
Strom B, Kimmel S, Hennessy S (2013) Textbook of pharmacoepidemiology. Wiley-Blackwell, Hoboken
Rothman K, Greenland S, Lash T (2008) Modern epidemiology. Lippincott Williams & Wilkins, Philadelphia
Wakata N, Nemoto H, Sugimoto H et al (2004) Bone density in myasthenia gravis patients receiving long-term prednisolone therapy. Clin Neurol Neurosurg 106(2):139–141. https://doi.org/10.1016/j.clineuro.2003.12.001
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
1.) Intellectual concept and design of the research: FV, ZS, and JD.
2.) Acquisition of data: PV.
3.) Analysis of data: JD.
4.) Interpretation of data: all authors.
5.) Original writing: ZS and RZ; Critical editing of written text: all authors.
6.) Approval of the definitive version of the manuscript: all authors.
7.) Accountable for legal and ethical aspects of the work: PV.
8.) Accountable for all other aspects of the work: JD.
Corresponding author
Ethics declarations
Conflict of interest
ZS: No conflict of interest.
JD: No conflict of interest.
JB: No conflict of interest.
PJ: No conflict of interest.
PV is the head of research at Steno Diabetes Center North Jutland, funded by the Novo Nordisk Foundation.
FV currently supervises three PhD students who are employed with F. Hoffmann La Roche Ltd. (Basel, Switzerland, and Welwyn Garden City, UK). He has not received any feeds or reimbursements for this. The topics of their PhD theses do not relate to the current manuscript.
RZ: No conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Safipour, Z., van der Zanden, R., van den Bergh, J. et al. The use of oral glucocorticoids and the risk of major osteoporotic fracture in patients with myasthenia gravis. Osteoporos Int 33, 649–658 (2022). https://doi.org/10.1007/s00198-021-06101-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-06101-3