Abstract
Summary
Human body height loss of 3–4 cm or more may be considered a simple indicator of increasing fracture risk, where the information is very similar to the results from fracture risk assessments by available online calculators, all of them based on a multiple variable approaches.
Introduction
The aim of the study was to assess the relationship between body height loss (HL) and fracture risk in postmenopausal women from the Gliwice Osteoporosis (GO) Study.
Methods
The study sample included 1735 postmenopausal women, aged over 55 years and recruited at the Osteoporotic Outpatient Clinic. The mean age of the study participants was 68.15 ± 8.16 years. Fracture risk was established, using the fracture risk assessment tool (FRAX) (10-year probability of major and hip fractures), the Garvan calculator (any and hip fractures, 5 and 10 years) and the Polish (POL-RISK) algorithm, available at www.fracture-risk.pl (any fractures, 5 years). Bone densitometry at the femoral neck was performed, using a Prodigy device (Lunar, GE, USA). Body heights were measured before bone densitometry, using a wall stadiometer and compared with the maximum body heights, measured in early adulthood and reported by the study participants themselves.
Results
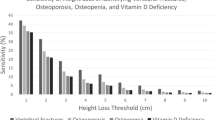
In 199 women, the body heights, measured during the study, did not change in comparison to their corresponding values in early adulthood, while being decreased in the other 1536 women. The mean height loss (HL) in the whole study group was 3.95 ± 3.24 cm. That HL correlated significantly with the calculated fracture risk (the r range from 0.13 to 0.39, p < 0.0001). In general, regarding the patients with fracture risk close to the recommended therapeutic thresholds, HL was around 3–4 cm, except of the values from the FRAX calculator for major fractures, where the commonly used therapeutic threshold (20%) was related to HL of approximately 6.5 cm. In subjects with HL between 3.5 and 4 cm (n = 208), the FRAX value for major fractures was 6.83 ± 3.74.
Conclusions
Body height measurements, carried out to establish HL, provide an important information for clinical practice, where HL of 3–4 cm or more may be considered a simple indicator of increasing fracture risk.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the recent decades, osteoporosis has been becoming an important medical issue in today’s human population. The first fracture, being the consequence of low-trauma events, is not only a short-term complication but also a rather strong predictor for future fractures. Therefore, an important point is to identify early signs of osteoporosis—prior to the first osteoporotic fracture. Several clinical risk factors for osteoporosis have been identified and included in predictive models, available as online calculators, such as FRAX [1], the Garvan algorithm [2, 3] and the Polish POL-RISK method [4], all of which are very helpful to assess the clinical condition and design an effective therapeutic programme. However, the data, which can be entered into a calculator formula, often do not fully reflect the actual patient’s health status. Therefore, these diagnostic tools should rather be regarded as complementary means to direct patient examination. The calculated risks and conclusions from the medical examination, including, among others, body height measurement, give a complete picture of the patient's clinical condition. The body height belongs to the input data in the FRAX and POL-RISK algorithms. Height loss (HL) may be considered to be a symptom of prevalent vertebral fractures and, in many today’s reports, HL has been described as a sign of the risk for future fractures, particularly for hip fractures [5,6,7,8,9,10,11,12,13,14,15]. However, HL is not included in the available calculators as a fracture risk factor.
Height loss is an important clinical indicator among the elderly and, at least in theory, it is easily measurable in daily practice. It must be admitted, however, that the accurate measurement of HL may not be as easy as it seems, especially, when we consider the obvious problems with establishing the historical body height in young adulthood. Nevertheless, the currently observed widespread use of electronic medical records, which ensure an easy access to lifelong medical data, may significantly improve the situation in the near future. HL may then be used on a large scale as a factor which may be helpful in the early identification of bone loss.
The aim of the study was to assess the relationship between HL and fracture risk in postmenopausal women, the latter factor being obtained from the available online calculators.
Material and methods
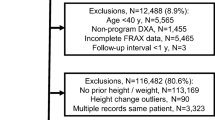
The study group included a cohort of 1735 women over 55 years of age, recruited from the database of an outpatient osteoporotic clinic in the southern Poland. The study was called the ‘Gliwice Osteoporosis Study’ (GO Study). The total number of registered patients was 2354. Women with available data, necessary to perform the required assessments (DXA measurement, HL calculation plus the risk factors, required in all the three fracture risk calculators), were enrolled into the reported study. Two other papers, based on the GO Study database, have recently been published [16, 17], and a more detailed description of the study group can be found in the first publication.
The data, regarding clinical risk factors for osteoporosis and fractures, were collected from all the patients, using a structured questionnaire. Bone densitometry (DXA) at femoral neck (FN) was performed by a Prodigy device (Lunar, GE, USA). All the measurements were carried out by one experienced operator. Body height was measured on the day of DXA exam, using a wall stadiometer (Seca, Germany), mounted according to the manufacturer’s recommendations.
The measured body height was compared with the maximum body height in early adulthood, as reported by the patient. All the body height measurements were performed by one DXA technician. Fracture risk was established, using the FRAXTM tool (www.sheffield.ac.uk, major and hip fractures, 10 years), the Garvan calculator (www.fractureriskcalculator.com, any and hip fractures, 5 and 10 years) and the Polish (POL-RISK) algorithm, available at www.fracture-risk.pl (any fractures, 5 years). FRAX scores express fracture probability within 10 years, limited by life expectancy, and the other two algorithms provide fracture risk assessments. Briefly, the FRAX algorithm takes into account: age, weight, height, femoral neck T-score and several clinical risk factors; the Garvan calculator includes age, the number of fractures after the age of 50 years, the number of falls during the previous year and femoral neck T-scores, while the POL-RISK algorithm takes into account steroid use, body height, prior fracture(s) after the age of 40 years, falls during previous 12 months and femoral neck T-scores. In order to establish HL values with regards to the fracture risk level, the following thresholds were assumed: FRAX: 20% and 3% (major and hip fractures, respectively); the Garvan calculator—any fractures risk during 5 years: <3%, 3–9% and >9%; the Garvan calculator—hip fracture risk during 5 years: <2%, 2–5% and >5%; the Garvan calculator—any fracture risk during 10 years: <14%, 14–26% and >26%; and the Garvan calculator—hip fracture risk during 10 years: <8%, 8–13% and >13%. The POL-RISK algorithm used the same thresholds as for the 5-year risk of any fracture in the Garvan model, i.e. <3%, 3–9% and >9%. The thresholds for the FRAX 10-year fracture risk were chosen, according to the National Osteoporosis Foundation’s recommendations. The corresponding thresholds for the Garvan model were used in line with the recommendations provided on the web page. Since no specific recommendations for the Pol-RISK 5-year fracture risk had been established till the time of the reported study, the same thresholds as in the for Garvan model were used.
A local ethics committee gave their official consent to the study protocol.
Statistics
A statistical analysis was performed, using the Statistica software (StatSoft, Tulsa, OK, USA). The mean values and standard deviations were used for descriptive statistics of continuous variables. The normality of data distribution was verified by the Shapiro-Wilk test. The Student’s t-test for independent samples or the Mann-Whitney U test was used (for data with and without a normal distribution, respectively) and was applied for comparative analyses. When more than two subgroups were compared, the analysis of variance (ANOVA) and post hoc verification with the least significant difference test (LSD) were applied. The Spearman correlation test was used for correlation analysis. The significance of results in all the statistical analyses was assumed at p < 0.05.
In addition, height loss (HL) was established in subsets of the patients who scored their individual fracture risk within a 90–100% risk range, assumed to be the therapeutic threshold (separately for each of the analysed calculators). Those ranges corresponded to FRAX hip (2.7–3%), FRAX major fractures (18–20%), Garvan 5-year hip fractures (4.5–5%), Garvan 5-year any fractures (8.1–9%), Garvan 10-year hip fractures (11.7–13%), Garvan 10-year any fractures (23.4–26%) and POL-RISK (8.1–9%).
Results
The mean age, body height, body weight and BMI were 68.15 ± 8.14 years, 157.14 ± 6.29 cm, 69.31 ± 12.98 kg and 28.08 ± 5.06 kg/m2, respectively. Out of that group, 1069 women had no fractures (61.6%), and 666 (38.4%) reported at least one fracture. Altogether, 1153 osteoporotic fractures were reported. As many as 372 women (21.5% of the study group) experienced one fracture, 167 (9.6%) had two fractures and 127 (7.3%) recalled three or more fractures. The number of women, reporting, at least, one major osteoporotic fracture (localised at spine, hip, forearm or arm region) was 557. See Table 1 for the exact number of major osteoporotic fractures at each of the listed skeletal region (including multiple fractures at the same site and multiple fractures at different sites in the same person).
The following clinical risk factors were identified in the examined women: hip fracture in parents—18, steroid use—115, rheumatoid arthritis—26, smoking—211, secondary reasons of osteoporosis—93 and falls during previous 12 months in 211 subjects. Alcohol consumption was not reported.
See Table 2 for demographic data and fracture risk assessment results. The heights, measured in 199 women, did not change in comparison to the previous heights of the same women in their early adulthood, while in 1536 women, their body height decreased by the mean value of 3.95 ± 3.24 cm. The mean T-score for FN BMD was −1.74 ± 0.92. HL correlated positively with age (r = 0.47, p < 0.0001), BMI (r = 0.21, p < 0.0001) and negatively with FN T-score (r = −0.21, p < 0.0001).
See Table 3 for the correlation analysis of HL with fracture risk assessment, where HL correlated significantly with all the fracture risk expressing variables.
The HL figures, observed in the studied subgroups, were stratified by assessed FRAX, Garvan and POL-RISK fracture risk levels—see Table 4. In general, HL increased together with the rising fracture risk.
Table 5 presents HL figures, observed in the subgroups with individual fracture risks, established in the range of 90–100% of the risk, assumed to be a therapeutic threshold in the analysed algorithms (see the sect. “Statistics” for details of the applied methodology). In general, the mean HL in those subjects, representing that fracture risk category was, around 3–4 cm, except of the FRAX calculator for major fractures in which the commonly used therapeutic threshold (20%) was related to HL close to 6.5 cm.
Because only in case of the FRAX major fractures, the height loss related to the therapeutic threshold of fracture risk was, clearly bigger than the corresponding figures, obtained in all the other calculators; an additional analysis was performed. The subjects with HL between 3.5 and 4 cm were selected from the whole study group in order to establish the mean FRAX value for major fractures in the subset of patients. As many as 208 women met that criterion, their average FRAX for major fractures was 6.83 ± 3.74%.
Discussion
Height loss in the elderly is a well-known phenomenon, but its clinical significance is still not fully comprehended. To our knowledge, the role of HL has not, so far, been studied with regards to fracture risk levels, established by available online methods. This issue gives then the reported study an innovative aspect. In many reports of other authors, HL was juxtaposed with fracture incidence [6,7,8,9,10,11,12,13,14,15], but its relationship with the level of fracture risk was not a dominating matter. A major point in our study was the establishment of HL magnitude as an indicator of fracture risk, recommended to be the treatment threshold, see Table 5.
Therefore, a simple measurement of body height, followed by the establishment of HL value in a subject diagnosed for osteoporosis, may be fairly helpful in daily practice. We believe that HL of 3–4 cm can be considered an additional indication to measure fracture risk. Height measurement should then be an integral part of osteoporotic diagnostics as the juxtaposition of the current height with its former maximal value provides an additional, valuable indicator of skeletal health. Several results in our study support this general conclusion. The HL range of approximately 3–4 cm was obtained for all the methods and fracture sites (hip, any fractures or major fractures) as the value corresponding with high fracture risk level, except of the FRAX calculator for major fractures. This diagnostic tool, applied in the subgroup of women with 18–20% risk of major fracture, corresponding to 90–100% of the risk assumed as the therapeutic threshold; the mean HL value was almost 6.5 cm. Therefore, one may hypothesise that the level of 20% is too high and patients with lower fracture risk, established by FRAX for major fractures, may be considered signals to launch treatment. When analysing the number of subjects in each risk category of the calculators (see Table 4), it is not so surprising that, in the high-risk group, processed by the FRAX calculator for major fractures, the mean HL value is significantly higher than for all the other calculators. Only 67 patients (3.8% of the study cohort) were classified as high-risk in the FRAX algorithm for major fractures, while in the remaining calculators, the number of subjects varied from 414 to 1088 (23.8–62.7% of the study cohort). This is an important signal that the therapeutic thresholds for risk calculators are not universal and may thus require local validation. In our cohort, when comparing the risk values to the HL scale, the FRAX fracture risk for major fractures of 7% corresponds to the high-risk group in the other calculators. Namely, the HL of about 3.5–4 cm is repeatedly related to exceeding the high-risk threshold in other calculators and, in parallel, it corresponds to 7% risk in FRAX for major fractures.
In another study, focused on the advantages of fracture risk assessment by FRAX and Garvan models in a group of 801 males, the optimal therapy onset threshold was established, by a ROC analysis at 7.6% for FRAX major fractures and 20.2% for the Garvan model option for any fractures [18]. The value of 7.6%, established in the cited study, is close to 6.83%, obtained in our study as the mean FRAX major fracture risk value for women from the subgroup with HL between 3.5 and 4.0 cm. Similar thresholds were obtained, despite that the former study was performed in males and the methodology (ROC analysis), applied to establish the optimal cut-off levels for sensitivity and specificity was different. One should also note that the optimal risk level, established by the Garvan model (20.2%), was only slightly lower from the recommended threshold of 26%.
One should remember that fracture incidence in patients with osteoporosis is an issue of key significance. This means that the methods, used to assess fracture risks, play an additional role only. Of course, the more accurate is fracture prediction, the results of these methods are more reliable. Therefore, reports of other authors support our results. The relationships between fracture incidence and HL scale, observed by other authors [8, 10, 11, 13,14,15], are consistent with the data presented in our study. The studies of other authors have shown that HL around 4 cm should be considered a significant risk factor for fracture incidence. The conformity between real fracture incidence and the thresholds, defined by online fracture assessment tools, is one of the highlights in our study. We may hypothesise that the therapeutic thresholds, presented in Table 4, can be considered useful in everyday clinical practice. Only the FRAX major fracture risk threshold should be lower (around 7%) according to the results in our study.
When planning the reported study, we did not assume that HL could be an additional and independent factor which, for example, could be accounted for by risk calculators in the future. Quite on the contrary, we assumed that it was rather a ‘marker’ of the concomitance of various risk factors, and our intention was to find out whether the use of this single, simple parameter can replace risk calculators, at least, in certain situations, e.g. when it is impossible to collect a necessary data input for calculator algorithms.
Our study has also some limitations. No long-term observation was carried out which could thus have provided more reliable information. The study cohort was not representative for the general population. The study was performed only in women. Clinically diagnosed vertebral fractures were included exclusively, while some spinal fractures may have gone unrecognised. No precise maximum body height data were available. Being self-reported by the study participants, the assessment of HL could be subjective and thus different from real values. Based on literature reports, HL overestimation may be assumed, resulting from the tendency to overestimate the self-reported maximum body height values by patients [19]. This problem may easily be solved in the near future by digitisation of medical records, allowing easy access to unbiased archival data from whole patient’s life.
However, the size of the study group and fracture risk data, obtained from three available online models provided important data for practitioners.
Conclusion
The measurement of actual body height to establish height loss (HL) provides an important information for daily clinical practice. HL of 3–4 cm or more may be considered a simple indicator of an increased fracture risk, presenting information very similar to the results from fracture risk calculation by available online calculators, the apparatus of which is based on multiple variable assessments. Further studies are postulated to verify if HL measurements may be sufficient enough to reliably establish medical indications for osteoporosis treatment, especially, if data, which are necessary as the input for fracture risk calculators, are not fully available. Nowadays, as electronic medical records with complete medical history become more and more popular, exact HL values will be easily available and thus its clinical importance may increase. This is especially encouraging to find out whether HL values can play the role of a single predictor of future fractures, preferably in studies based on prospective observations.
References
Kanis JA, Cooper C, Rizzoli R, Reginster JY (2019) Scientific Advisory Board of the European Society for Clinical and Economic Aspects of Osteoporosis and Osteoarthritis (ESCEO) and the Committees of Scientific Advisors and National Societies of the International Osteoporosis Foundation (IOF). Executive summary of European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Aging Clin Exp Res 31:15–17
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2007) Development of a nomogram for individualizing hip fracture risk in men and women. Osteoporos Int 18:1109–1117
Nguyen ND, Frost SA, Center JR, Eisman JA, Nguyen TV (2008) Development of prognostic nomograms for individualizing 5-year and 10-year fracture risks. Osteoporos Int 19:1431–1434
Adamczyk P, Werner A, Bach M, Żywiec J, Czekajło A, Grzeszczak W, Drozdzowska B, Pluskiewicz W (2018) Risk factors for fractures identified in the algorithm developed in 5-year follow-up of postmenopausal women from RAC-OST-POL study. J Clin Densitom 21(2):213–219
Armstrong MEG, Kirichek O, Cairns BJ et al (2016) Relationship of height to site-specific fracture risk in postmenopausal women. J Bone Miner Res 31(4):725–731
Vogt TM, Ross PD, Palermo L et al (2000) Vertebral fracture prevalence among women screened for the fracture intervention trial and a simple clinical tool to screen for undiagnosed vertebral fractures. Fracture Intervention Trial Research Group. Mayo Clin Proc 75:888–896
Nguyen TV, Center JR, Sambrook PN, Eisman JA (2001) Risk factors for proximal humerus, forearm, and wrist fractures in elderly men and women: the DUBBO osteoporosis epidemiology study. Am J Epidemiol 153:587–583
Moayyeri A, Luben RN, Bingham SA, Welch AA, Wareham NJ, Khaw KT (2008) Measured height loss predicts fractures in middle-aged and older men and women: the EPIC-Norfolk prospective population study. J Bone Miner Res 23:425–432
Hillier T, Liu L-Y, Kado DM et al (2012) Height loss in older women: risk of hip fracture and mortality independent of vertebral fractures. J Bone Miner Res 27:153–159
Hannan MT, Broe KE, Cupples LA, Dufour AB, Rockwell M, Kiel DP (2012) Height loss predicts subsequent hip fractures in men and women of the Framingham Study. J Bone Miner Res 27:146–152
Mikula AL, Hetzel SJ, Binkley N, Anderson PA (2017) Validity of height loss as a predictor for prevalent vertebral fractures, low bone mineral density, and vitamin D deficiency. Osteoporos Int 28:1659–1665
Leslie WD, Schousboe JT, Morin SR et al (2020) Measured height loss predicts incident clinical fractures independently from FRAX: a registry-based cohort study. Osteoporos Int 31:1079–1087
Kamimura M, Nakamura Y, Sugino N et al Associations of self-reported height loss and kyphosis with vertebral fractures in Japanese women 60 years and older: a cross-sectional survey. Sci Rep 6:29199. https://doi.org/10.1038/srep29199
Yoh K, Kuwabara A, Tanaka K (2014) Detective value of historical height loss and current height/knee height ratio for prevalent vertebral fracture in Japanese postmenopausal women. J Bone Miner Metab 32:533–538
Krege JH, Kendler D, Krohn K, Genant H, Alam J, Berclaz PY, Coffey B, Loghin C (2015) Relationship between vertebral fracture burden, height loss, and pulmonary function in postmenopausal women with osteoporosis. J Clin Densitom 18:506–511
Pluskiewicz W, Adamczyk P, Drozdzowska B (2021 Jan) The significance of height loss in postmenopausal women. The results from GO Study. Int J Clin Pract 7:e14009. https://doi.org/10.1111/ijcp.14009
Pluskiewicz W, Adamczyk P, Drozdzowska B (2021) Low dietary calcium intake does not modify fracture risk but increases falls frequency: the results of GO Study. Endokrynol Pol. On-line first; doi: 10.5603/EP.a2021.0021
Pluskiewicz W, Adamczyk P, Franek E, Sewerynek E, Leszczynski P, Wichrowska H, Napiórkowska L, Stuss M, Ptaszek A, Kostyk T, Golba KS, Garbacz W, Drozdzowska B (2014) FRAX calculator and Garvan nomogram in male osteoporotic population. Aging Male 17:174–182
Krul AJ, Daanen HA, Choi H (2011) Self-reported and measured weight, height and body mass index (BMI) in Italy, the Netherlands and North America. Eur J Pub Health 21:414–419
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Pluskiewicz, W., Adamczyk, P. & Drozdzowska, B. Height loss in postmenopausal women—do we need more for fracture risk assessment? Results from the GO Study. Osteoporos Int 32, 2043–2049 (2021). https://doi.org/10.1007/s00198-021-05941-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-021-05941-3